World AIDS Day 2021 — Dec. 1st — End inequalities. End AIDS
WHO
December 1, 2021
HIV remains a major public health issue that affects millions of people worldwide.
Although the world has made significant progress in recent decades, important global targets for 2020 were not met.
- Division, disparity and disregard for human rights are among the failures that allowed HIV to become and remain a global health crisis.
- Now, COVID-19 is exacerbating inequities and disruptions to services, making the lives of many people living with HIV more challenging.
The theme of World AIDS Day 2021 is “ End inequalities. End AIDS”.
With a special focus on reaching people left behind, WHO and its partners are highlighting the growing inequalities in access to essential HIV services.
On 1 December 2021, WHO is calling on global leaders and citizens to rally to confront the inequalities that drive AIDS and to reach people who are currently not receiving essential HIV services.
Originally published at https://www.who.int on December 1, 2021.

HIV/AIDS
The human immunodeficiency virus (HIV) targets the immune system and weakens people’s defense against many infections…www.who.int
Key facts
- HIV continues to be a major global public health issue, having claimed 36.3 million [27.2–47.8 million] lives so far.
- There is no cure for HIV infection. However, with increasing access to effective HIV prevention, diagnosis, treatment and care, including for opportunistic infections, HIV infection has become a manageable chronic health condition, enabling people living with HIV to lead long and healthy lives.
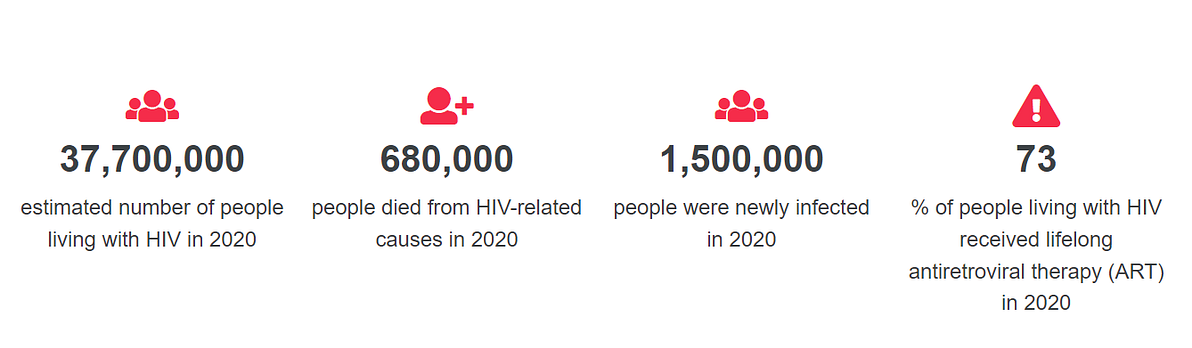
- There were an estimated 37.7 million [30.2–45.1 million] people living with HIV at the end of 2020, over two thirds of whom (25.4 million) are in the WHO African Region.
- In 2020, 680 000 [480 000–1.0 million] people died from HIV-related causes and 1.5 million [1.0–2.0 million] people acquired HIV.
- To reach the new proposed global 95–95–95 targets set by UNAIDS, we will need to redouble our efforts to avoid the worst-case scenario of 7.7 million HIV-related deaths over the next 10 years, increasing HIV infections due to HIV service disruptions during COVID-19, and the slowing public health response to HIV.
The human immunodeficiency virus (HIV) targets the immune system and weakens people’s defense against many infections and some types of cancer that people with healthy immune systems can fight off. As the virus destroys and impairs the function of immune cells, infected individuals gradually become immunodeficient. Immune function is typically measured by CD4 cell count.
The most advanced stage of HIV infection is acquired immunodeficiency syndrome (AIDS), which can take many years to develop if not treated, depending on the individual. AIDS is defined by the development of certain cancers, infections or other severe long-term clinical manifestations.
Signs and symptoms
The symptoms of HIV vary depending on the stage of infection. Though people living with HIV tend to be most infectious in the first few months after being infected, many are unaware of their status until the later stages. In the first few weeks after initial infection people may experience no symptoms or an influenza-like illness including fever, headache, rash or sore throat.
As the infection progressively weakens the immune system, they can develop other signs and symptoms, such as swollen lymph nodes, weight loss, fever, diarrhoea and cough. Without treatment, they could also develop severe illnesses such as tuberculosis (TB), cryptococcal meningitis, severe bacterial infections, and cancers such as lymphomas and Kaposi’s sarcoma.
Transmission
HIV can be transmitted via the exchange of a variety of body fluids from infected people, such as blood, breast milk, semen and vaginal secretions. HIV can also be transmitted from a mother to her child during pregnancy and delivery. Individuals cannot become infected through ordinary day-to-day contact such as kissing, hugging, shaking hands, or sharing personal objects, food or water.
It is important to note that people with HIV who are taking ART and are virally suppressed do not transmit HIV to their sexual partners. Early access to ART and support to remain on treatment is therefore critical not only to improve the health of people with HIV but also to prevent HIV transmission.
Risk factors
Behaviours and conditions that put individuals at greater risk of contracting HIV include:
- having unprotected anal or vaginal sex;
- having another sexually transmitted infection (STI) such as syphilis, herpes, chlamydia, gonorrhoea and bacterial vaginosis;
- sharing contaminated needles, syringes and other injecting equipment and drug solutions when injecting drugs;
- receiving unsafe injections, blood transfusions and tissue transplantation, and medical procedures that involve unsterile cutting or piercing; and
- experiencing accidental needle stick injuries, including among health workers
Diagnosis
HIV can be diagnosed through rapid diagnostic tests that provide same-day results. This greatly facilitates early diagnosis and linkage with treatment and care. People can also use HIV self-tests to test themselves. However, no single test can provide a full HIV diagnosis; confirmatory testing is required, conducted by a qualified and trained health or community worker at a community centre or clinic. HIV infection can be detected with great accuracy using WHO prequalified tests within a nationally approved testing strategy.
Most widely-used HIV diagnostic tests detect antibodies produced by the person as part of their immune response to fight HIV. In most cases, people develop antibodies to HIV within 28 days of infection. During this time, people experience the so-called window period — when HIV antibodies haven’t been produced in high enough levels to be detected by standard tests and when they may have had no signs of HIV infection, but also when they may transmit HIV to others. After infection, an individual may transmit HIV transmission to a sexual or drug-sharing partner or for pregnant women to their infant during pregnancy or the breastfeeding period.
Following a positive diagnosis, people should be retested before they are enrolled in treatment and care to rule out any potential testing or reporting error. Notably, once a person diagnosed with HIV and has started treatment they should not be retested.
While testing for adolescents and adults has been made simple and efficient, this is not the case for babies born to HIV-positive mothers. For children less than 18 months of age, serological testing is not sufficient to identify HIV infection — virological testing must be provided as early as birth or at 6 weeks of age. New technologies are now becoming available to perform this test at the point of care and enable same-day results, which will accelerate appropriate linkage with treatment and care.
Prevention
Individuals can reduce the risk of HIV infection by limiting exposure to risk factors. Key approaches for HIV prevention, which are often used in combination, include:
- male and female condom use;
- testing and counselling for HIV and STIs;
- testing and counselling for linkages to tuberculosis (TB) care;
- voluntary medical male circumcision (VMMC);
- use of antiretroviral drugs (ARVs) for prevention;
- harm reduction for people who inject and use drugs; and
- elimination of mother-to-child transmission (MTCT) of HIV.
Treatment
HIV disease can be managed by treatment regimens composed of a combination of three or more antiretroviral (ARV) drugs. Current antiretroviral therapy (ART) does not cure HIV infection but highly suppresses viral replication within a person’s body and allows an individual’s immune system recovery to strengthen and regain the capacity to fight off opportunistic infections and some cancers.
Since 2016, WHO has recommended that all people living with HIV be provided with lifelong ART, including children, adolescents, adults and pregnant and breastfeeding women, regardless of clinical status or CD4 cell count.
By June 2021, 187 countries had already adopted this recommendation, covering 99% of all people living with HIV globally. In addition to the treat all strategy, WHO recommends a rapid ART initiation to all people living with HIV, including offering ART on the same day as diagnosis among those who are ready to start treatment. By June 2021, 82 low- and middle-income countries reported that they have adopted this policy, and approximately half of them reported country-wide implementation.
Globally, 28.2 million people living with HIV were receiving ART in 2021. The global ART coverage rate was 73% [56–88%] in 2020. However, more efforts are needed to scale up treatment, particularly for children and adolescents. Only 54% [37–69%] of children (0–14 years old) were receiving ART at the end of 2020.
WHO response
The Sixty-Ninth World Health Assembly endorsed the “Global health sector strategy on HIV for 2016–2021”. The strategy includes five strategic directions that guide priority actions by countries and by WHO over six years.
The strategic directions are:
- Information for focused action (know your epidemic and response)
- Interventions for impact (covering the range of services needed)
- Delivering for equity (covering the populations in need of services)
- Financing for sustainability (covering the costs of services)
- Innovation for acceleration (looking towards the future).
WHO is a cosponsor of the Joint United Nations Programme on AIDS (UNAIDS). Within UNAIDS, WHO leads activities on HIV treatment and care, and HIV and TB coinfection, and jointly coordinates the work on elimination of MTCT of HIV with UNICEF.
- Global health sector strategy on HIV, 2016–2021
- Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021
- Consolidated HIV strategic information guidelines
- Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach
- Global guidance on criteria and processes for validation: elimination of mother-to-child transmission of HIV, syphilis and hepatitis B virus
- Assessment of HIV testing services and antiretroviral therapy service disruptions in the context of COVID-19: lessons learned and way forward in sub-Saharan Africa












