BCG Gamma
Wangjing (Jing) Ke, Aryana Jacobs, Ritin Khangarot & Satty Chandrashekhar
August, 4, 2021
The COVID-19 crisis has illuminated the value of resilience in healthcare, as some organizations have shown themselves better able than others to absorb the shock of the pandemic — and have gone further than others to take advantage of the lasting changes brought about by the crisis.
Healthcare systems and health agencies around the world have mobilized and collaborated across their mandates to contain the spread of the virus, develop vaccines, and save lives.
Core public health services have adopted and accelerated digitization and AI, adapting and innovating to respond to this unprecedented change.
After closely observing many examples of such resilience, we at BCG firmly believe that the use of data & analytics in healthcare has become no less than table-stakes for survival.
To flourish amid a new world of continuous disruption, health systems must implement advanced analytics that, with every passing day, unlock new expressions of human potential.
And yet, many questions remain.
- How can health systems and public health leaders ensure that their organizations carry forward the positive momentum prompted by the crisis?
- How can they convert this momentum into reforms that enable organizations and governments to better serve citizens long after the crisis is over?
- How can they shepherd and shape more resilient public health services?
We are all trying to draw lessons from successful efforts to respond to the crisis, and to apply those lessons to health systems that are — and will likely continue to be — under strain as long as the pandemic continues.
But we must also address questions about how we can prepare for and cope with shocks that may occur in the future.
In this exploratory article about using AI and advanced analytics to build a resilient healthcare system, we focus on the big picture. We define healthcare resilience, and we explain why organizations must build it now.
Index
- Withstand, Adapt to, and Recover from Adversity
- The Tangible Benefits of Resilience
- AI’s Increased Role in Healthcare
- Why is Resilience so Important Now?
- How Can Data, Analytics, and Digital Technology Help Build More Resilient Health Systems?
- Nine Areas for Improved Resilience
- Next Steps
Withstand, Adapt to, and Recover from Adversity
What exactly do we mean by resilience?
The WHO defines health system resilience¹ as the ability to prepare for, manage (absorb, adapt, and transform), and learn from shocks.
Similarly, public health resilience is the ability of a community to use its assets to strengthen public health and healthcare systems and to improve the community’s physical, behavioral, and social health so that it can withstand, adapt to, and recover from adversity.
We believe the key resilience traits for a public health system include the ability to:
- Anticipate and prepare for worst-case scenarios
- Create different types of capabilities to respond to crises
- Connect with a broader system to provide external buffers
- Hold excess capacity and resources to buffer shocks
- Organize in loosely linked modules to isolate the impact
- Build capability to respond quickly to changes
The Tangible Benefits of Resilience
The notion of resilience in a health system context often focuses on preparedness, response, and an ability to cope with specific shocks.
COVID-19, however, has created a perfect storm that calls upon the industry to fundamentally redefine its conception of resilience.
During the pandemic, health systems strove to manage the crisis by unlocking unprecedented levels of funding, upscaling alternative channels of care, loosening regulatory requirements, and forming new, hitherto uncontemplated partnerships.
As they did, they became aware of acute shortcomings in the current health infrastructure including
- badly disrupted supply chains,
- sharp declines in health services, and
- the creation of barriers that disproportionately limited access to care for patients from lower socioeconomic backgrounds.
These are important adaptations, and historical data shows that organizations that adapt, that purposefully develop the ability to tackle the unpredictable and the ambiguous, are more likely to thrive.
According to BCG research² of more than 1,200 transformations over the last 25 years, resilient organizations better absorb the impact of a crisis, and often recover faster and to a greater extent.
Now, with such transformation powered by data & analytics, healthcare systems are even more likely to realize positive, long-term improvements³
- in agility (up to 50%),
- workforce productivity (up to 30%), and
- performance (up to 20% in additional EBIT).
AI’s Increased Role in Healthcare
Clearly, the pandemic has affected all healthcare ecosystem stakeholders:
- emergency healthcare providers,
- non-acute-disease healthcare providers,
- patients,
- the insurance industry,
- and healthcare start-ups.
The crisis has shocked many health systems’ operations, income statements, and staff.
As demand has overwhelmed hospital capacity, healthcare workers have faced persistent understaffing, long hours, shortages of diagnostic supplies and personal protective equipment (PPE), and most troubling, the need to make difficult ethical choices amid stressful events.
Our research has found that that the use of digital technology has singularly helped these stakeholders improve their resilience. It has done so by
- supporting containment,
- accelerating the acquisition and distribution of PPE,
- more effectively allocating healthcare capacity to meet surges in demand,
- accelerating vaccine development, and
- creating increasingly resilient supply chains.
Even before Covid-19, several initiatives were begun to build healthcare resilience via digital channels.
- Provider investments in “Digital Front Door” capabilities helped strained systems navigate the typical, pre-pandemic, end-to-end patient journey by introducing seamless patient registration and scheduling processes that decreased hospital lobby traffic⁴, while
- the initiative’s remote patient-monitoring capabilities freed patients from the burden of traveling to healthcare institutions.
Once Covid-19 struck, rapid integration of digital technology and AI served as a conduit for navigating shocks to healthcare systems around the world.
- For example⁵, several countries relied on digital platforms to monitor relevant hospital bed capacity, supply chain volumes, and manufacturing capacity, and to track distributions.
- Telehealth capabilities highlighted significant access gaps (known familiarly as the digital divide) that further exacerbated existing healthcare disparities. (At the same time, many insurance providers lifted restrictions to telehealth-consultation coverage, while several states and service providers relaxed regulations surrounding the use of telehealth, and increased community health worker engagement to aid in increasing telehealth literacy⁶ )
- Robotic process automation (RPA) coupled with AI has emerged as an additional path to resilience⁷, serving as a crucial timesaver for systems experiencing staff shortages and other personal constraints.
The ability of RPAs to manage repetitive, time-consuming tasks such as registering patients, billing, and claims processing freed up already stretched healthcare staff so they could spend more time with COVID-19 patients. And this trend is increasing.
At the time of a 2020 Gartner study, only 5% of healthcare providers were investing in RPA systems.
Since the pandemic, fully half of the healthcare practices surveyed said they planned to increase resilience by investing in RPAs over the next 3 years.
Several EHR companies are also integrating versions of RPA into their software.
Why is Resilience so Important Now?
Resilience is top of mind for many healthcare executives today who understand that they face an increasingly uncertain and volatile world.
For years, public sector entities have been struggling to keep pace with technological change.
This challenge has only accelerated since the Covid 19.
The pandemic has brought into sharp focus the realization that only those entities that have purposefully developed the ability to tackle ambiguity and unpredictability will thrive amid the tumult.
Today, public health agencies are increasingly grappling with key resilience questions, including:
- How do we increase health equity — the ability of all segments of a population to access public health, healthcare, and social services?
- How do we expand communication and collaboration to promote health and wellness?
- How do we enhance surveillance to quickly detect shocks, and then assess their impact?
- How do we identify and engage at-risk individuals earlier in their disease journey?
- In what areas can we reduce waste in the healthcare delivery network
- How do we optimally distribute our human and physical resources so that we can adjust capacity to cope with unforeseen surges in demand?
How Can Data, Analytics, and Digital Technology Help Build More Resilient Health Systems?
With almost every healthcare organization increasingly dependent on data, analytics, digital tools, and automation, digital technologies will constitute an increasingly critical element of public health resilience.
We believe there is a clear path to build digitally resilient public health systems. To do so, these systems must:
- Reinforce data and technology systems for capacity planning and healthcare footprint optimization
- Segment and stratify at-risk populations using social determinants of health to improve access to care, outcomes, and equity across the healthcare system
- Apply advanced analytics to identify and reduce waste (resources, capacity);
- Reinforce data and technology systems for capacity planning and healthcare footprint optimization. This will entail:
- Making care-delivery processes efficient through the use of analytics (i.e., take-out time and cost)
- Simulating resource-allocation contingency scenarios, and measuring their impact
- Establishing “control towers” to provide operational decision support for health agencies with defined metrics and early warning system/trigger points for intervention
- Expanding public health data infrastructures with targeted capabilities to anticipate crises and enable better response measures
- Advancing data & analytics talent
2. Segment and stratify at-risk populations using social determinants of health to improve access to care, outcomes, and equity across the healthcare system.
This will include measuring health outcomes for disadvantaged (e.g., vulnerable) groups to inform policies and social programs, and engaging vulnerable, elderly, and disadvantaged populations via a multi-channel strategy. Success will depend on the organization’s ability to:
- Disseminate timely information on public health, behavioral health, and emergency preparedness measures
- Leverage multiple channels including digital applications and telehealth
3. Apply advanced analytics to identify and reduce waste (resources, capacity), with particular emphasis on:
- Analysis of claims data in conjunction with other data that informs health outcomes (e.g. vaccination records, socio-economic data, etc.)
- Decision support and simulation for Medicaid policy/rate changes
The following three pillars are essential to support these initiatives and to further the transformation toward increased resilience:
1.The right data governance. There is no one-size-fits-all data governance strategy when it comes to healthcare systems. The right data governance will simplify data topology, improve cross-system communication, and help accumulate data asserts for analytics.
2.An interoperable digital data platform (DDP). A DDP that is capable of supporting machine learning models or advanced analytics algorithms is the foundation of any data-based initiative. It provides the physical power to unlock the value of data.
3.A skilled workforce. Investing in data governance and DDP construction is pointless without the right workforce or talent to make the best use of these investments. Both data governance and DDP are continuous efforts. As such, stakeholders need to develop in-house capabilities to capture the value creation and drive changes on a day-to-day basis.
Nine Areas for Improved Resilience
In general, we believe that healthcare organizations must expand their understanding of resilience.
They must go beyond the often inconsistently held definitions to include new capabilities that will help them more predict and prepare for potential system shocks.
To strengthen their data & analytics capabilities in particular, we recommend that commercial and public health organizations focus on nine discrete areas:
Nine ways to build healthcare resilience with advanced analytics
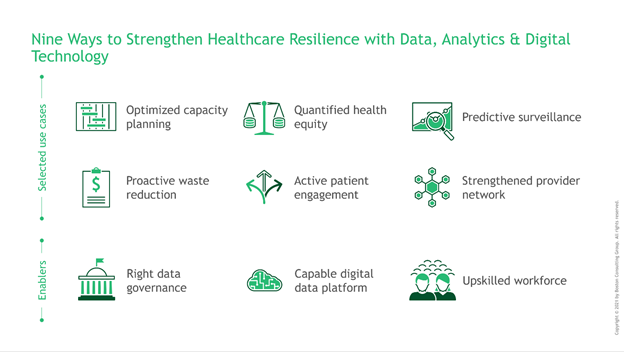
In our experience, these areas are rich with internal and external data; cut across functions, scenarios, and stakeholder journeys; and enable the use of a foundational infrastructure.
Combined with emerging AI approaches, they can make the concept of resilience real for health systems and healthcare organizations.
Leaders must consider each area individually, in combination, and at scale in their resilience efforts.
Next Steps
We propose a gradual and phased approach to building healthcare resilience using AI and advanced analytics.
Given the complexity and diversity of the current healthcare system, even the slightest change can carry profound implications and second-order consequences that executives must thoughtfully assess.
Executives must also consider the challenges of their organizations’ legacy IT infrastructures and workforce growth to ensure the adoption of new mindsets and technology.
In future articles, we will continue to explore selected use cases and examples of infrastructure building that demonstrate how to effectively bring the quality of resilience to your organization.
Citations
- https://www.euro.who.int/__data/assets/pdf_file/0005/351284/resilience-report-20171004-h1635.pdf
- https://www.bcg.com/publications/2020/digital-path-to-business-resilience
- https://www.bcg.com/publications/2020/digital-path-to-business-resilience
- https://www.healthleadersmedia.com/revenue-cycle/how-covid-19-kicked-open-digital-front-door-memorial-health-system
- https://doi.org/10.1038/s41591-021-01381-y
- https://www.tandfonline.com/doi/full/10.1080/17538157.2020.1839467
- https://www.notablehealth.com/blog/augmenting-ai-with-rpa-how-intelligent-automation-solves-healthcare-problems
Originally published at https://medium.com on August 6, 2021.












