Health Transformation Institute (HTI)
research institute, knowledge portal and advisory consulting
Joaquim Cardoso MSc*
Founder, and Chief Researcher & Editor
December 1, 2022
MSc* from London Business School
MIT Sloan Masters Program
Senior Advisor for Health Transformation & Digital Health
This is republication of an excerpted version of the article “Leveraging data to transform healthcare”, with the title above.
Oracle Health
Stephanie Trunzo
Senior Vice President and GM, Oracle Health
March 14, 2022
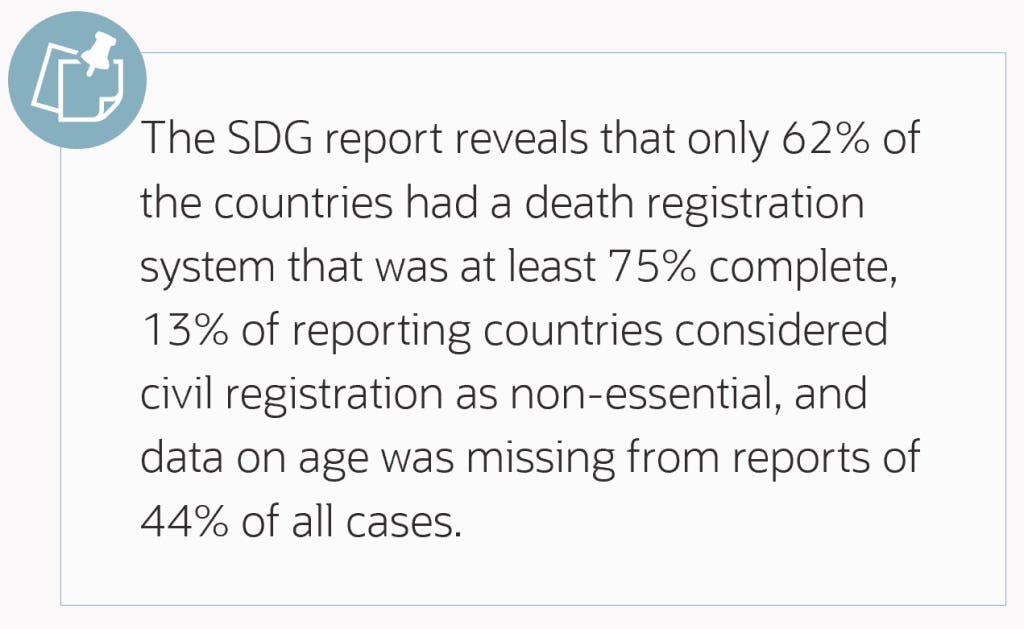
A report by the Global Sustainable Development Goals (SDG) Indicators Database calls for data innovation; it identifies the lack of internationally comparable data as the main impediment to understanding the impact of the COVID-19 pandemic¹.
Despite the challenges, healthcare organizations across the world relied on data to understand the spread of the pandemic, forecast community outbreaks, predict patient admissions, and allocate resources.
the lack of internationally comparable data is the main impediment to understanding the impact of the COVID-19 pandemic
The need of the moment propelled data innovation in developing public health surveillance systems and vaccines.
Using advanced Machine Learning (ML) tools, pharmaceutical companies sped the process of reviewing clinical trial data for vaccines².
In collaboration with the U.S. Government, Oracle built a Cloud-based national central data repository and a suite of public health management applications to help public health agencies manage vaccine distribution and collect and analyze real-time patient data related to COVID-19 vaccines and treatments.
In collaboration with the U.S. Government, Oracle built a Cloud-based national central data repository and a suite of public health management applications
Data is interdisciplinary and we are all connected by it.
If utilized correctly, it helps patients, providers, scientists, and the public in ways that could bolster the overall health arc of our society:
- A traveling patient carries their unified healthcare data in a single longitudinal record
- A provider reviews a patient’s entire medical history and predicts health risks through one click
- A geographically dispersed care team monitors a patient’s vitals in real-time
- International researchers use de-identified data to discover root causes and develop novel treatments
- Analysts use the above data to map trends in population health
Data is interdisciplinary and we are all connected by it. If utilized correctly, it helps patients, providers, scientists, and the public in ways that could bolster the overall health arc of our society
The COVID-19 pandemic has taught us that not only can we meet a moment of crisis, but we also have the tools and brainpower to innovate data for a better future.
The question is, how much are we willing to?
The COVID-19 pandemic has taught us that not only can we meet a moment of crisis, but we also have the tools and brainpower to innovate data for a better future. The question is, how much are we willing to?

What did we learn?
The pandemic highlighted some flaws in how we utilize data in healthcare:
- 1.Data Disparity
- 2.Legacy Systems
- 3.Data Velocity
- 4.Information Barriers
1.Data Disparities
Kimberle Crenshaw ³, a civil rights advocate and scholar, coined the term intersectionality in the late eighties.
This term describes how certain individual characteristics intersects and overlaps to create systems of disadvantage for individuals.
During the pandemic, this powerful approach remained underutilized in revealing inequities in data, such as the role of demographics and other social factors on COVID-19 45.
Disparate data standards and algorithmic bias obstruct population health advancements and reduce health equity due to skewed outcomes. Additional layers provide equitable results, such as race, ethnicity, and language (REaL) data.
Disparate data standards and algorithmic bias obstruct population health advancements and reduce health equity due to skewed outcomes. Additional layers provide equitable results, such as race, ethnicity, and language (REaL) data.
2.Legacy Systems
Legacy systems may lead to information silos between hospital systems and domains.
Hospitals can hoard treatment data that they are unwilling to share with other research centers.
The lack of collaboration inhibits innovation, limits data-driven decision-making, and ultimately affects patients.
Paper records continue to be used, adding to the operational overload in an age when mobile clinicians can capture and analyze data at a patient’s bedside on a device.
Healthcare organizations acquire tools for specific needs; these tools lack the benefits of comprehensive solutions that improve the patient’s overall journey.
Integrating platforms that offer comprehensive solutions provide better patient outcomes.
The lack of collaboration inhibits innovation, limits data-driven decision-making, and ultimately affects patients. Integrating platforms that offer comprehensive solutions provide better patient outcomes.
3.Data Velocity
The velocity of data is increasing faster than the speed at which we can understand it.
According to RBC Capital Markets, 30% of all the world’s data volume is from the healthcare industry.
Data becomes available from different mediums, such as IoT, Artificial Intelligence (AI), ML, etc.
It needs to be quickly, securely, and accurately captured and analyzed.
Centralized and secured cloud-based data platform enables analysts to move between health disciplines and hospital systems, allowing them to build a standard set of reports to compare data, capture trends, and facilitate decision-making.
The velocity of data is increasing faster than the speed at which we can understand it. … 30% of all the world’s data volume is from the healthcare industry.
Centralized and secured cloud-based data platform enables analysts to move between health disciplines and hospital systems, allowing them to build a standard set of reports to compare data, capture trends, and facilitate decision-making.
4.Information Barriers
Digital health systems remain focused on the business and compliance requirements of an organization, not fully opening to information exchange.
Information exchange within the four walls promotes system-based knowledge transfer and not outcome- or value-based care.
That can change with the final rule of the ONC’s Cures Act 6.
The Act prohibits information blocking practices and promotes innovation in patient-centric technology to foster easy access to health information.
IT developers will require standardized APIs and FHIR technology to support data exchange, and providers are expected to use these technologies in providing care.
Breaking the informational blockage between digital health systems will provide an end-to-end experience for patients.
Information exchange within the four walls promotes system-based knowledge transfer and not outcome – or value-based care.
That can change with the final rule of the ONC’s Cures Act 6 — that prohibits information blocking practices and promotes innovation in patient-centric technology to foster easy access to health information.
Breaking the informational blockage between digital health systems will provide an end-to-end experience for patients.
Simplifying the Complex
In the Oracle CIO Exchange featuring DJ Patil, former Chief Data Scientist of the United States Office of Science and Technology Policy, …
… we talked about driving innovation through data to solve some of the nation’s biggest problems, the intention behind sharing data, as well as the trust that leads to that consent.
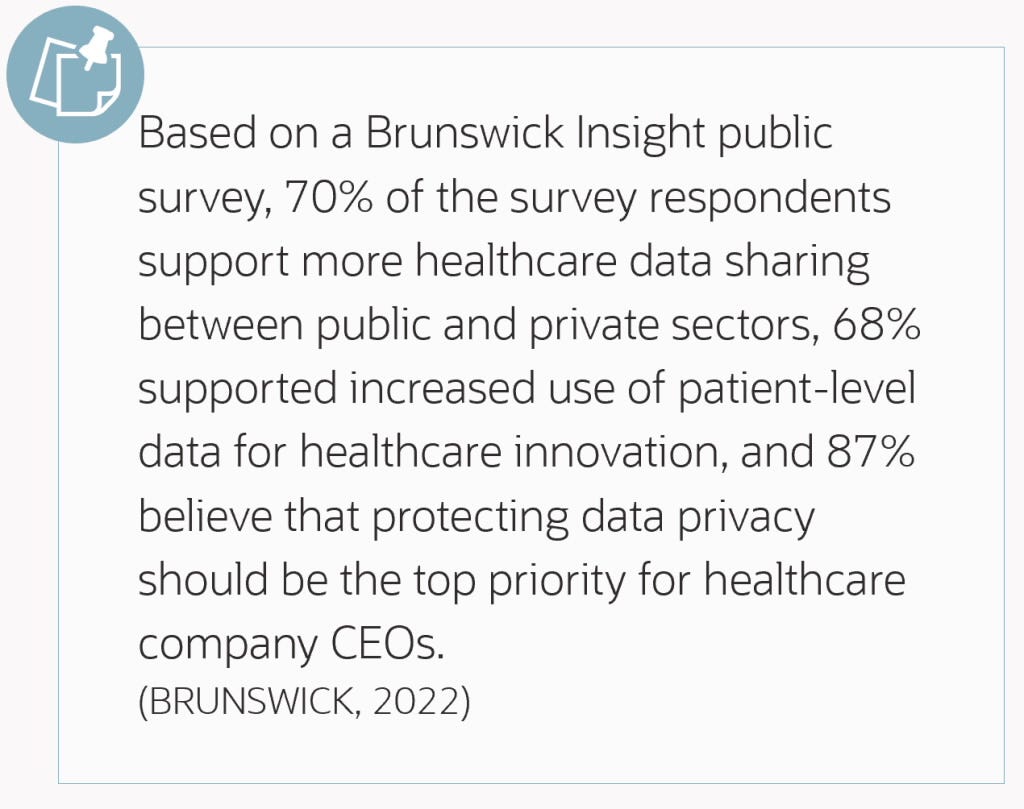
We can leverage data to improve healthcare outcomes, but we cannot do it without public support, and data privacy is crucial to garnering support.
We can leverage data to improve healthcare outcomes, but we cannot do it without public support, and data privacy is crucial to garnering support
The digital revolution in Big Data analytics, AI, and ML is helping providers connect data across different disciplines — from genomics to mental health.
As healthcare organizations become agile in adapting to these technologies and moving towards value-based care, maintaining data integrity, and integrating data insights and information assets into their care delivery model is becoming more critical now than ever.
The digital revolution in Big Data analytics, AI, and ML is helping providers connect data across different disciplines — from genomics to mental health.
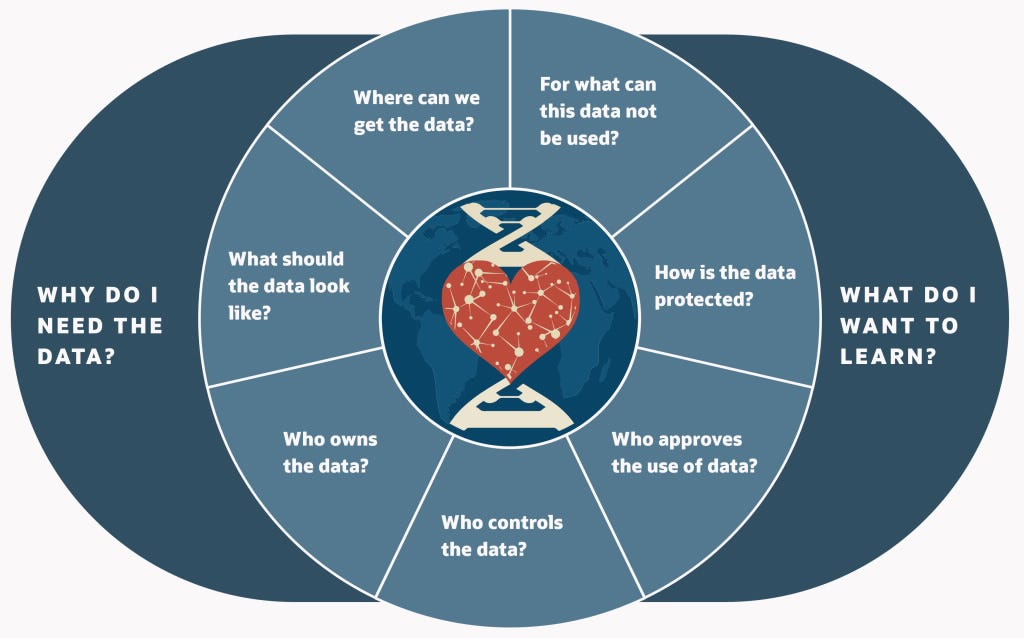
Data-driven healthcare stakeholders need to develop an outside-in approach — What do we want to learn and achieve, and what’s our part in that? — then work backward to the data requirements.
They also need to reevaluate how they treat and leverage data and develop an understanding of education, policies, and perceptions about the role of data in our society.

We must unify global data through innovation, and that starts with the right intentions — consent to share and the motivation to innovate beyond the four walls.
We would be better prepared for future emergencies with clarity, transparency, and a comprehensive data-driven strategy across all healthcare organizations.
About the authors
Stephanie Trunzo
Senior Vice President and GM, Oracle Health

Originally published at https://blogs.oracle.com.
Names mentioned
DJ Patil, former Chief Data Scientist of the United States Office of Science and Technology Policy