Health Transformation Institute (HTI)
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
December 18, 2022
Executive Summary
- The urgency of climate change calls for mandatory development and adoption of transparent and standardized metrics for whole-organization greenhouse-gas accounting in health care, …
- as well as for the creation of governance and infrastructure for decarbonization-related measurement by all HCOs.
- Policy changes are needed to support all HCOs in performing greenhouse-gas measurements while providing impetus for improvement, shared learning, and development of best practices.
- Successful health care system decarbonization will require a standardized and systematic national reporting structure for performance tracking and changes to payment and accreditation procedures that take into account greenhouse-gas emissions.
- Actions proposed herein could accelerate the transition to a sustainable future.
Infographic
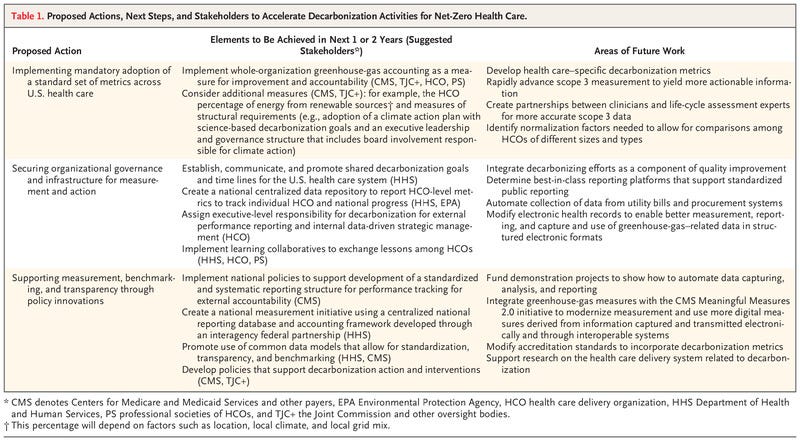
Figure 1 — recommended metrics
ORIGINAL PUBLICATION
Mandatory Reporting of Emissions to Achieve Net-Zero Health Care
NEJM
Hardeep Singh, M.D., M.P.H., Matthew Eckelman, Ph.D., Donald M. Berwick, M.D., M.P.P., and Jodi D. Sherman, M.D.
December 14, 2022
The most recent assessment by the United Nations Intergovernmental Panel on Climate Change (IPCC) states that climate change is happening faster than expected and that the window to take action is quickly closing.1
Immediate, rapid, and large-scale reductions in greenhouse-gas emissions are needed to limit warming to 1.5°C and avert the worst predicted harms. Morbidity and mortality from climate-related threats — such as food and water insecurity, changes in disease-vector ranges and seasonality, and heat, wildfire, and other weather-related events — are rising, and health care systems are at increasing risk for disruption.2,3
The health care sector is responsible for approximately 5% of global emissions and 8.5% of emissions at the national level in the United States.4,5
In 2018, greenhouse gases and toxic air emissions associated with the health care sector led to an estimated loss of 388,000 disability-adjusted life-years.4
In recognition of their shared responsibility to decarbonize, many health systems are increasing their commitments to achieve “net zero” — that is, conditions in which released greenhouse-gas emissions are counterbalanced by means to remove them from the atmosphere.6,7
The health care sector is responsible for approximately 5% of global emissions and 8.5% of emissions at the national level in the United States.4,5
In 2018, greenhouse gases and toxic air emissions associated with the health care sector led to an estimated loss of 388,000 disability-adjusted life-years.4
Recent developments herald increasing momentum for decarbonizing health care.7,8
The U.K. National Health Service (NHS) has long been a leader in tracking its own carbon emissions, …
… and following their 2020 pathbreaking “Delivering a Net Zero Health Service” strategy, more than 50 countries committed to achieving low-carbon sustainable health systems through a new World Health Organization initiative at the COP26 meeting in November 2021.
These countries included the United States, with its newly established Department of Health and Human Services (HHS) Office of Climate Change and Health Equity helping to coordinate multiple new national efforts.9
In September 2021, the National Academy of Medicine launched a new Action Collaborative on Decarbonizing the U.S. Health Sector.10
In April 2022, the Centers for Medicare and Medicaid Services (CMS) issued a request for information on how health care providers can respond to climate risks and reduce their emissions and how HHS can support these efforts; in the same month, HHS and the White House issued a “call to action” for health care stakeholders to commit to reducing emissions across the health care sector.11,12
In June 2022, at a related White House event, 61 U.S. health care and industry signatories pledged to cut their greenhouse gases in line with the recent goal of making the federal government net zero by 2050.13
Despite these encouraging developments, voluntary pledges and initiatives will not be adequate to reach net-zero health care goals.14,15
Implementation of standardized metrics for reporting health care greenhouse gases is essential to quantify progress, identify best practices, and ensure accountability.15,16
Health systems globally are developing decarbonization policies and procedures that fit within their governance structures.
Several other countries have begun measuring, setting targets, and implementing interventions to achieve health care decarbonization goals.17,18
Health systems globally are developing decarbonization policies and procedures that fit within their governance structures.
Several other countries have begun measuring, setting targets, and implementing interventions to achieve health care decarbonization goals.17,18
Under mandate, NHS England aims to be net zero by 2045, and resources and implementation authority were embedded into U.K. legislation in 2022.19–21
The United States does not have similar legislated targets or resources.
Under mandate, NHS England aims to be net zero by 2045, and resources and implementation authority were embedded into U.K. legislation in 2022.19–21
The United States does not have similar legislated targets or resources.
The recent mandates of the U.S. government to achieve net-zero emissions from its operations by 2050 encompass federal health systems; however, with so few nonfederal health systems pledging to decarbonize, and in the absence of standardized measures, accountability, and support, we risk the U.S. health system failing to do its part to meet the IPCC goals.
Proposed Actions, Next Steps, and Stakeholders to Accelerate Decarbonization Activities for Net-Zero Health Care.
We thus recommend that greenhouse-gas–related measurement and reporting should be a requirement for all health care delivery organizations (HCOs), …
… broadly defined to include inpatient, outpatient, and residential care and their supporting services (e.g., offices, laboratories, and warehouses).
Although HCOs currently face competing priorities and are already reporting many quality measures and new greenhouse-gas–related reporting requirements are likely to feel onerous, the urgency of the climate crisis and its implications for public health and health system preparedness demand such action.22
We propose the following actions to implement greenhouse-gas–related measurement activities in HCOs to accelerate decarbonization efforts (Table 1):
implementing mandatory adoption of a standard set of reporting metrics across U.S. health care; securing organizational governance and infrastructure for measurement and action; and supporting measurement, benchmarking, and transparency through policy innovations.
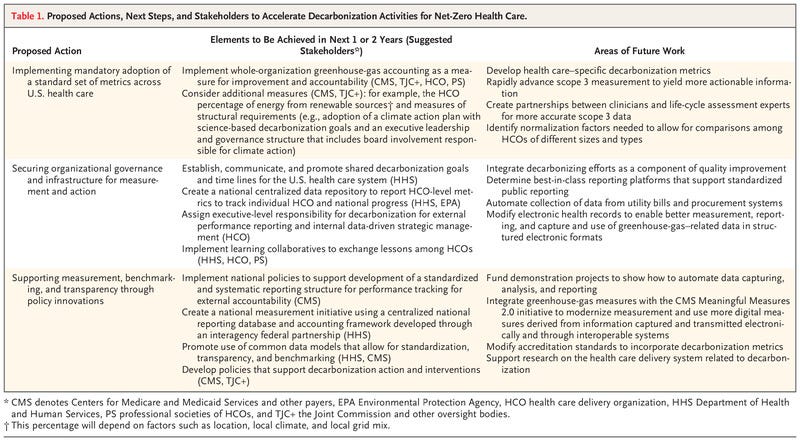
Implementing Mandatory Adoption of a Standard Set of Metrics across U.S. Health Care
Currently, HCO reporting of greenhouse-gas emissions in the United States (outside of federal systems) is voluntary.
Health care systems have no universally accepted, standardized greenhouse-gas measures, reporting, or management systems, although reporting frameworks outside of health care have long existed.
Ideally, HCO metrics should make use of existing international measurement standards within the framework of the Greenhouse Gas Protocol (GHG Protocol), which delineates how different sources of emissions must be accounted for.15,23
The GHG Protocol is used for virtually all international carbon-reporting frameworks, across industries.
In health care quality efforts, measurement is used for both accountability and improvement purposes.
The same holds true for health care decarbonization, which can appropriately be considered an additional dimension of quality of care.16,24,25
In health care quality efforts, measurement is used for both accountability and improvement purposes.
The same holds true for health care decarbonization, which can appropriately be considered an additional dimension of quality of care.16,24,25
Because health care–induced pollutants cause harm to patients, the health care workforce, and society more broadly, decarbonizing efforts should be viewed explicitly as a component of quality improvement.
Even though these harms are indirect and external to an organization, they can and should be classified with other, more direct forms of injury to patients.
Metrics can enable performance reporting and transparency for accountability purposes for both HCOs and the entire U.S. health system.
Likewise, measurement can inform local HCO improvement efforts, help to evaluate and facilitate sharing of decarbonization initiatives, and identify best practices.
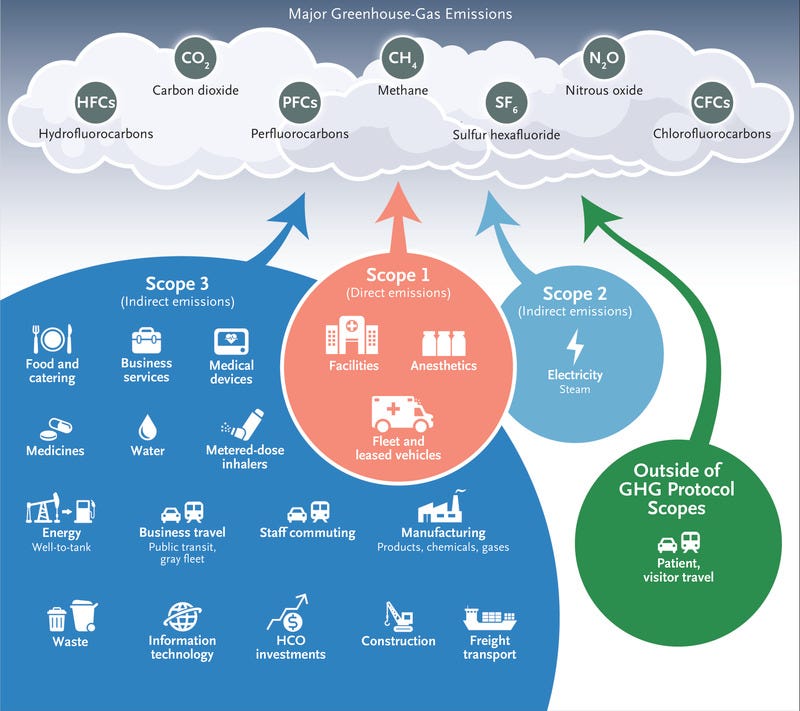
RECOMMENDED METRICS
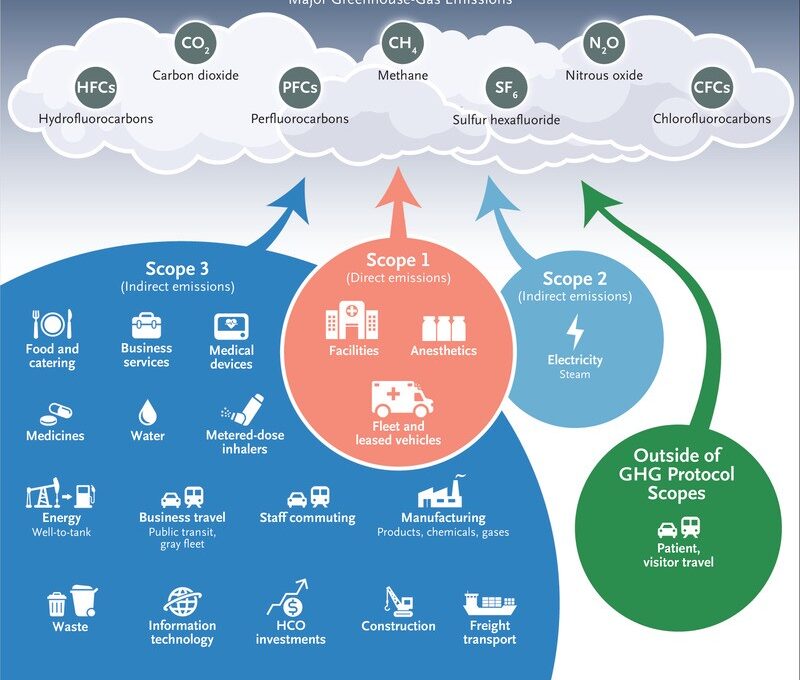
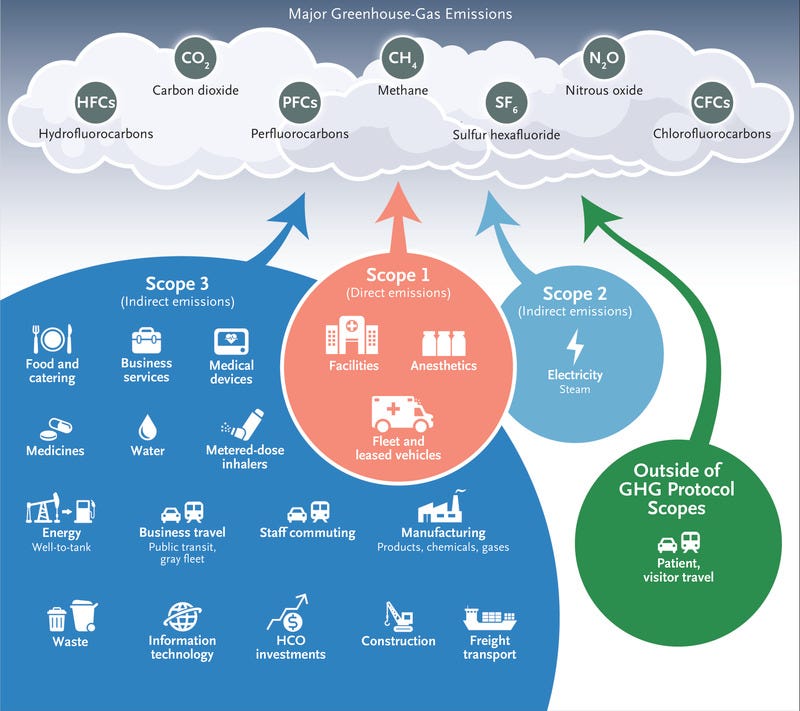
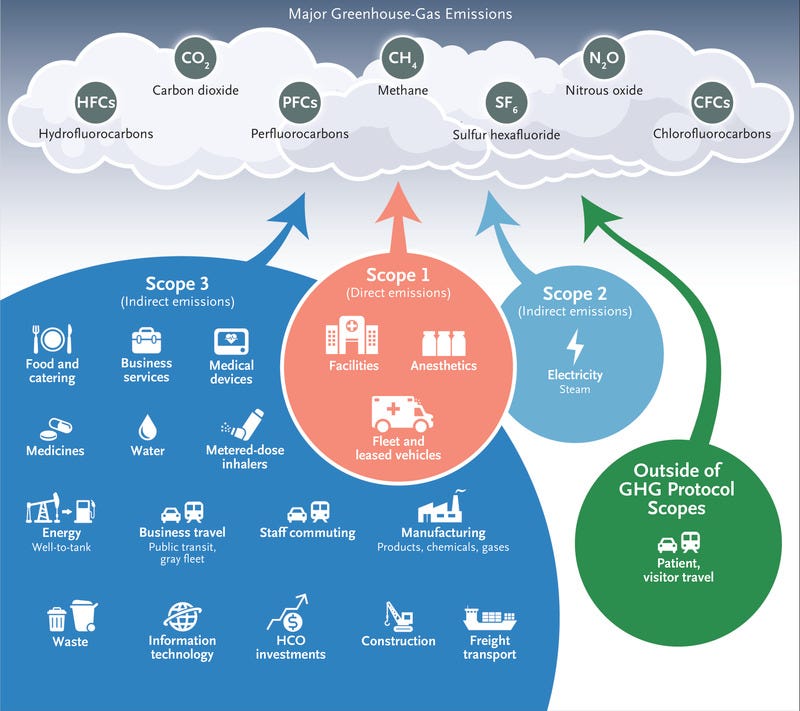
Figure 1.
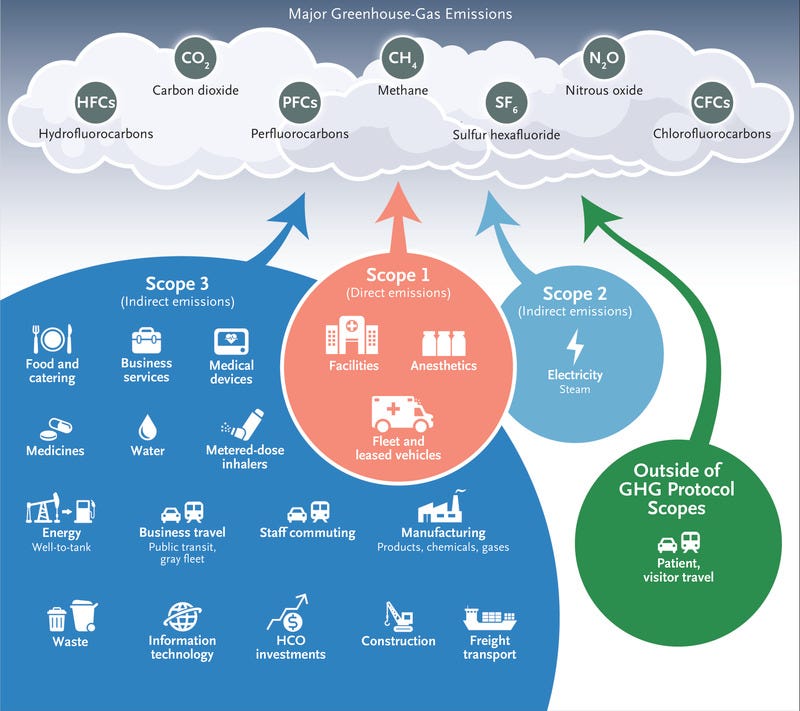
GHG Protocol Scopes for U.S. Health Care.
Calculating total organization greenhouse-gas emissions is essential to guide strategic management.
Such an effort requires accounting for greenhouse gases emitted directly from health care facilities, such as those from on-site boilers and medical gases (referred to as scope 1 under the GHG Protocol), those emitted indirectly through purchased energy (scope 2), and all other indirect emissions (scope 3).
Scope 3 covers 15 categories, including emissions from purchased goods and services, employee commuting, and waste management (Figure 1).
Several HCOs, including the Veterans Affairs health system, already measure scopes 1 and 2, but accounting of emissions from scope 3 is still evolving.
Each scope 3 category has its own measurement guidance published within the GHG Protocol standards; the recommended approach depends on the data available.
For example, for purchased goods and services, most studies to date have relied on expenditure-based modeling, which provides national mean carbon intensities for each category of purchase but not for specific products themselves.4,5
As manufacturers and researchers publish more product-level carbon-footprint data, it will be possible to perform accounting that is more detailed, actionable, and HCO-specific than is currently possible.
Few organizations in any sector currently account for all scope 3 categories; most report only on those that are most relevant or convenient.
However, because approximately 80% of U.S. health care emissions stem from scope 3, measuring relevant categories that occur upstream or downstream from health care delivery will be critical for guiding decarbonization efforts.4
On the basis of existing literature and experience, as well as input from National Academy of Medicine Climate Collaborative member organizations representing private and public health entities (see the Supplementary Appendix, available with the full text of this article at NEJM.org), …
… we recommend HCO absolute greenhouse-gas emissions as the best single measure to implement first.4,18,26
… we recommend HCO absolute greenhouse-gas emissions as the best single measure to implement first.
We recognize that reporting of some scope 3 categories may need to be phased in over time, given the underdeveloped state of manufacturer data and HCO data-collection infrastructure for certain categories and the complexity of the health care supply chain as compared with sectors that have relatively fewer and simpler inputs (e.g., steel production). Table 1 shows additional priority measures.
Mandatory reporting of emissions is only an enabling first step in implementing decarbonization.
Additional health care–specific metrics are needed to define and set benchmarks of progress and to serve as key decarbonization performance indicators.
Normalization factors that reflect clinical activity must also be considered.
At the highest level, this can include factors such as occupied bed-days for a hospital and patient encounters for outpatient clinics or specific types of clinical services provided.26
Combining these measures with existing measures of health system performance (e.g., quality and efficiency of care, costs, equity, and care outcomes) can help to ensure that decarbonization outcomes are patient-centered.16
Some structural indicators are also important to evaluate, such as the adoption of a climate action plan by HCOs; the appointment of executive leadership responsible for climate change accounting, mitigation, and adaptation performance; and HCO governance that includes board-level oversight, reporting, and stewardship accountability.
Securing Organizational Governance and Infrastructure for Measurement and Action
Governance and infrastructure are needed for implementation of greenhouse-gas accounting, external performance reporting, and internal data-driven strategic management.
We recommend that HCOs designate a leader or unit responsible for decarbonization who is committed to implementing measurement activities (e.g., data capture, auditing, and reporting) and improving health care infrastructure, the supply chain, and delivery processes to reduce pollution while maintaining or improving care quality.
Systematic collection of actionable performance data, analysis of variation, identification of low-value care (inclusive of clinical outcomes, costs, resource consumption, and environmental performance) within the system, and continuous feedback are integral to guiding evidence-based improvement and for developing a decarbonization-focused learning health system approach.6,16,27
Data analytics and data platforms are also needed for transparent public reporting of decarbonization measures and for knowledge sharing.
An additional step is the development of better information-management systems to enable data capture, storage, and information display, which will support the setting of benchmarks for decarbonization indicators and public reporting.
For instance, a national centralized data repository could be developed to report HCO-level metrics to track individual HCO and national progress, illuminating best practices for low-carbon, patient-centered, equitable health systems.
The Environmental Protection Agency (EPA) has extensive experience with hosting and managing facility-level emissions reporting, including reporting for HCOs, through their ENERGY STAR Portfolio Manager program.
More than 3500 U.S. hospitals already use the ENERGY STAR Portfolio Manager to assess their energy performance relative to that of their peers,28 but the program is not currently configured for whole-organization carbon accounting.28
However, this tool and other current and forthcoming front-end reporting tools can be modified to capture standardized variables for scopes 1, 2, and 3.
A partnership between HHS and the EPA could build on the existing EPA program and implement a centralized national reporting database.
A whole HCO accounting framework could feasibly be developed within the next year through the integration of existing supply-chain accounting tools and through knowledge sharing with the NHS and other health systems.29,30
The increasing amount of electronically available data supports rigorous measurement and reporting of decarbonization.
Automation of data collection from utility bills and procurement records would limit burdensome data gathering by HCOs.
Comprehensive data-management systems are needed to ensure reliable and automated data capture and integration.
Systematic national efforts to modify electronic health records to enable capture and use of structured data related to emissions could facilitate the measurement, display, integration, and monitoring of information on embodied greenhouse-gas emissions embedded in the supplies, medications, diagnostics, and treatment pathways used in care delivery, as well as the identification of best practices.16
Whereas top-down accounting can illuminate which types of clinical products or processes are most carbon intensive, detailed life-cycle analyses will be necessary to differentiate among clinical options.
Better electronic capture of resource-consumption data and real-time metrics display can influence clinical, procurement, and supply-chain management decisions and nudge decision-makers toward carbon-friendly choices (e.g., selection of inhaled anesthetics with low greenhouse-gas emissions.)16,25,31,32
Supporting Measurement, Benchmarking, and Transparency through Policy Innovations
HCOs currently face many competing priorities and challenges and spend substantial resources to comply with reporting requirements of numerous performance measures.
To facilitate rapid adoption of greenhouse-gas accounting, HCOs will need support and guidance, including guidance as to what data sources to use for generating reports.
Because all HCOs are resource-constrained, they will direct their attention first to measures required explicitly by accrediting agencies and payers; policy changes related to payment and accreditation are needed to support greenhouse-gas measurement and accounting.4
RECOMMENDATIONS TO ENABLE STANDARDIZED AND SYSTEMATIC MANDATORY REPORTING NATIONALLY
Policy innovations should support the development of a standardized and systematic reporting structure for performance tracking and external accountability.33
Creation of a national measurement system that uses a centralized national reporting database and accounting framework is now essential.
This system could be developed through an interagency federal partnership under the auspices of HHS and funded by Congress.
Payment mechanisms through value-based purchasing, quality-measure reporting programs, and Conditions of Participation (standards that HCOs should meet to participate in CMS programs) should create incentives for HCOs to report their scope 1 and 2 emissions through this common platform.
Incentives for reporting of scope 3 emissions could be added subsequently.4
Decarbonization efforts should be integrated with existing public reporting initiatives on accountability for quality, such as the CMS Hospital Care Compare program.4,16,34
Because measurement alone is insufficient, additional policy changes and funding mechanisms must support decarbonization action and interventions.
Unintended consequences of performance measurement — for example, the burden of reporting, as well as insufficient attention to improvement efforts and subsequent gaming of measures — may emerge and undermine efforts.
The use of electronic data and automated measures can reduce measurement burden, and standardized methods can help to avert “greenwashing” (i.e., making misleading claims to appear environment-friendly).35
New policies could provide funding for demonstration projects to show how data capture, analysis, and reporting can be automated.
Unintended consequences of performance measurement — for example, the burden of reporting, as well as insufficient attention to improvement efforts and subsequent gaming of measures — may emerge and undermine efforts.
New policies could provide funding for demonstration projects to show how data capture, analysis, and reporting can be automated.
NEXT STEPS FOR CREATING A MEASUREMENT ECOSYSTEM
Engaging stakeholders involved in quality measurement, such as the National Quality Forum and National Committee on Quality Assurance, is important.
We recommend that the Joint Commission and other oversight bodies modify accreditation surveys and standards to incorporate decarbonization metrics while simultaneously reducing regulatory burdens.4,16
True transparency requires verifiable (accountant-assured) disclosures, and therefore random audits by payers and accreditation bodies will be needed.
Case studies and best practices from the HCOs showing the fastest progress toward decarbonization, verified through reporting, should be disseminated.
Given the present dearth of funding at the intersection of health services research and climate change, support for health care delivery system science and discovery pertaining to decarbonization is needed from organizations such as the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Centers for Disease Control and Prevention.4,16
Conclusion
The urgency of climate change calls for mandatory development and adoption of transparent and standardized metrics for whole-organization greenhouse-gas accounting in health care, as well as for the creation of governance and infrastructure for decarbonization-related measurement by all HCOs. Policy changes are needed to support all HCOs in performing greenhouse-gas measurements while providing impetus for improvement, shared learning, and development of best practices. Successful health care system decarbonization will require a standardized and systematic national reporting structure for performance tracking and changes to payment and accreditation procedures that take into account greenhouse-gas emissions. Actions proposed herein could accelerate the transition to a sustainable future.
About the authors & authors affiliations
From the Center for Innovations in Quality, Effectiveness, and Safety, Michael E. DeBakey
Veterans Affairs Medical Center and Baylor College of Medicine — both in Houston (H.S.);
Northeastern University (M.E.) and the
Institute for Healthcare Improvement (D.M.B.) — both in Boston; and
Yale University, New Haven, CT (J.D.S.).
Originally published at https://www.nejm.org.