the health strategist
research institute for continuous transformation
— in health & care
Joaquim Cardoso MSc
Chief Researcher & Editor
March 22, 2023
This is a republication of an excerpt of the paper “Reasons for encounter in primary health care in Brazil”, with the title above.
(Chueiri PS, Gonçalves MR, Hauser L, Wollmann L, Mengue SS, Roman R, Rodrigues Agostinho Rech M, Soares MAV, Pertile J, Harzheim E. Reasons for encounter in primary health care in Brazil. Fam Pract. 2020 Oct 19;37(5):648–654. doi: 10.1093/fampra/cmaa029. PMID: 32297637)
Abstract
Background:
- Primary health care (PHC) delivery in Brazil has improved in the last decades.
- However, it remains unknown whether the Family Health Strategy teams are meeting the health needs of the population.
Objectives:
- To describe the reasons for encounter (RFEs) in PHC in Brazil and to examine variations in RFEs according to sex, age and geographic region.
Methods:
- This descriptive study is part of a national cross-sectional study conducted in 2016.
- The sample was stratified by the number of PHC physicians per geographic region.
- Physicians who had been working for at least 1 year in the same PHC unit were included.
- For every participating physician, 12 patients aged ≥18 years who had attended at least two encounters were included.
- Patients were asked about their RFEs, which were classified according to the International Classification of Primary Care.
Results:
- In 6160 encounters, a total of 8046 RFEs were coded.
- Seven reasons accounted for 50% of all RFEs.
- There was a high frequency of codes related to test results, medication renewal and preventive medicine.
- RFEs did not vary significantly by sex or geographic region, but they did by age group (P < 0.001).
- The rates of prescriptions, requests for investigations and referrals to specialized care were 71.1%, 42.8%, and 21.3%, respectively.
Conclusion:
- This novel study opened the ‘black box’ of RFEs in PHC in Brazil.
- These findings can contribute to redefining the scope of PHC services and reorienting work practices in order to improve the quality of PHC in Brazil.
Key Messages
- The comprehensiveness of care of Brazilian primary care teams is still limited.
- Reasons for encounter in Brazil do not vary by region as do morbidity data.
- Prevention is a top reason for prioritizing healthy people’s access to primary care.
- Prescription renewal and review of exams are the main reasons for encounter.
- These problems could be resolved by other technologies or health professionals.
DEEP DIVE
Reasons for encounter in primary health care in Brazil
Health Service Research
Patricia S Chueiria,*, Marcelo Rodrigues Gonçalves b, Lisiane Hauser c, Lucas Wollmann d, Sotero Serrate Mengue b,c, Rudi Romanb, c, Milena Rodrigues Agostinho Rech e, Marcelo de Araújo Vianna Soares b, Jamily Pertileb and Erno Harzheimb, f
16 April 2020
BACKGROUND
Brazil has a public national health care system that is funded by federal taxes and operated by municipal governments.
Created in 1988, the system provides comprehensive care for any citizen without copayments or patient charges.
Over the past 30 years, Brazil has developed a national policy on primary health care (PHC), the Family Health Strategy (FHS).
FHS teams consist of a family physician, a nurse and community health workers, and each team is in charge of an average of 3500 patients from a specific area.
However, it is not possible for patients to choose their FHS team.
FHS currently covers 63% of the Brazilian population, and those not enrolled in the FHS seek care mainly in emergency departments and walk-in clinics.
It is important to note that 22% of the Brazilian population have private health insurance and only occasionally use the public health system[1].
Universal health coverage has not yet been achieved owing to three major problems:
· (1) public underfunding of PHC and chronic inefficiency of the public health system;
· (2) lack of specific PHC medical training and maldistribution of PHC physicians; and
· (3) the country’s federal system that hinders the municipal management of health services[2].
In recent years, the FHS has been co-responsible for improvements in the country’s health indicators, including a decline in infant mortality rates and in hospitalizations for ambulatory care sensitive conditions[3] [4].
However, there is currently a drop in vaccination coverage, a new syphilis epidemic and a plateau in the quality of chronic disease management.
PHC-based health systems undoubtedly have better health outcomes[5].
To achieve this impact, the core principles of PHC must be followed: providing patient-centered care, being responsible for the population under care and having high clinical resolution.
It is also important that PHC teams are able to recognize patients’ health problems[6], act as the communication core of the health system and advocate for patients.
Current challenges to PHC practice in Brazil include tailoring care to the health needs of the population and improving the ability of the teams to follow the core principles of PHC, with a consequent increase in clinical resolution[7].
Traditional indicators, such as morbidity and mortality rates, have long been considered limited in their capacity to describe both patients’ needs and physicians’ actions.
However, it is the collective impact of these needs and actions that determines the demand for and use of health services. In this context, the patient should be the primary unit of analysis rather than the disease[8].
In the 2013 Brazilian National Health Interview Survey, 48% of respondents reported that the municipal PHC unit is their first point of contact with the health system[9].
Therefore, the PHC team is in a unique position to assess the utilization of medical care resources and to recognize users’ health needs, which can be identified through surveys that address the reasons for encounter (RFEs).
These are the reasons for seeking care from the perspective of the patient, that is, the reasons given by the patient before any health professional makes any judgment[10].
Knowing RFEs is different from knowing the most common diagnoses or morbidities of a population; it includes a better understanding of the supply and demand of health services and maybe a better understanding of resource utilization.
RFEs reflect not only the diseases but also the symptoms, requests (for investigations, prescriptions, referrals or counseling), expectations and emotions (concerns and fears) that make people seek health care.
To date, no study has examined at a national level the RFEs in PHC in Brazil.
Therefore, it remains unknown whether FHS teams are meeting the health needs of the population and what PHC services are being delivered.
The aim of the present study was to describe the RFEs in PHC in Brazil and to examine variations in these reasons according to sex, age and geographic region.
METHODS & RESULTS
See the original publication (this is an abstract version only)

DISCUSSION
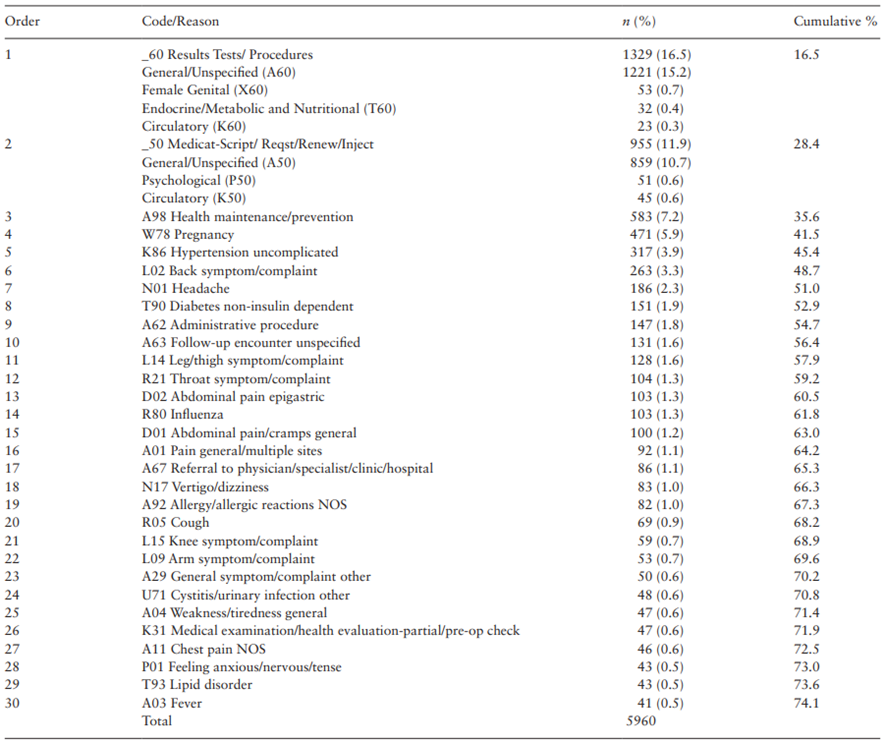
The main finding of this study was that only 7 reasons accounted for 50% of all RFEs in PHC in Brazil when administrative RFEs (_60, _50, and A62 codes) were included.
This result suggests that PHC in Brazil is currently providing a narrow range of health services, focused on clinical-administrative or follow-up reasons, which limits the comprehensiveness of care, with a negative impact on the delivery of PHC for common problems faced by the Brazilian population.
Also, this result differs from those reported in the national literature, where regional surveys (Florianópolis/SC, Porto Alegre/RS, Betim/MG, and Fortaleza/CE) have found that a mean of 30 reasons account for 50% of all RFEs in PHC[11] [12] [13], including clinical-administrative reasons.
The RFE related to the analysis of additional tests (ICPC-2 code _60 Results Tests/Procedures) was the most commonly recorded code in the present study, as well as in all Brazilian studies[14] [15] [16] [17] [18].
It is also found in the list of RFEs of international studies but at a lower rate[19] [20] [21] [22].
Regarding ‘medication-script/request/renewal/injection’ (ICPC-2 code _50), this code is among the top 3 RFEs listed in all national surveys[23] [24] [25] [26] [27] — in contrast to the international literature, where only six studies have reported this code, always at a lower rate[28] [29] [30] [31] [32] [33].
This finding may be associated with Brazilian standards on prescription validity, which are defined regionally; in some regions, prescriptions are only valid for a short length of time.
This creates excessive demand for appointments with a physician for reasons (such as prescription renewal) that could be handled by another health professional or by other means, such as email, telemedicine or even telephone, potentially limiting access for those who really need to see a physician.
However, these rates may be overestimated because all patients in the present study were at least on their second visit.
Table 2. Top 30 reasons for encounter in primary health care as coded by the International Classification of Primary Care, Second Edition (Brazil, July–December 2016)
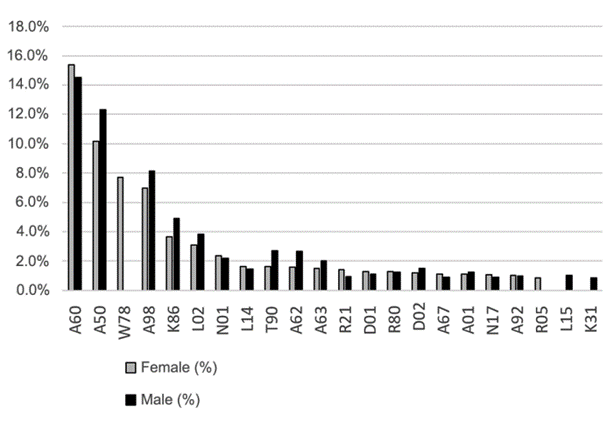
Women accounted for the majority of PHC service users, a result that is consistent with the literature[34] [35] [36] [37] [38] [39] [40] [41] [42] [43] [44] and could be suggestive, among other reasons, of limited access to services by men.
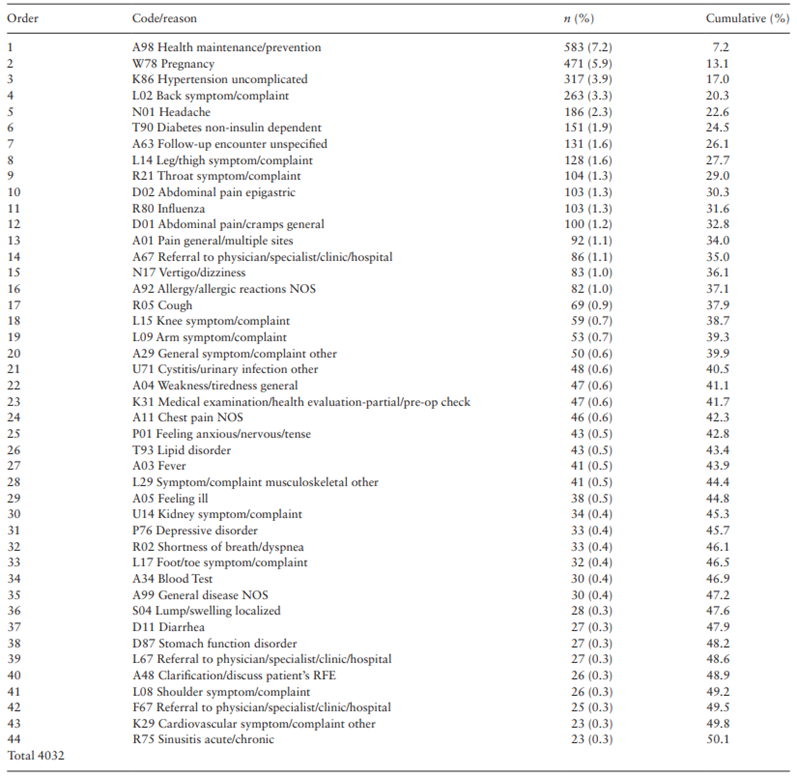
Another important finding was that ‘health maintenance/prevention’ (ICPC-2 code A98) was among the most common RFEs, and the following are examples of answers given by the patients: ‘I am coming for a routine appointment’; ‘I want to have a checkup’; ‘I am coming for general investigations’.
This is in agreement with the national literature[45] [46] but is in contrast to the international literature, where only a Greek study recorded this code[47].
This finding indicates that healthy people have greater access to health services than sick people (vulnerable), supporting the inverse care law[48].
This practice raises concerns because it may lead to further reduction of the already scarce resources for those most in need, thus increasing the inequities in access to health care in the Brazilian public health system[49].
When comparing the data from the present study with morbidity and mortality data from the Global Burden of Disease Study — Brazil[50], in which depression and anxiety were the fifth and sixth leading causes of morbidity, an unexpected finding was the low rate of RFEs related to ICPC-2 chapter P (psychological problems).
However, low back pain, headache and diabetes, reported as leading causes of morbidity, were also present in our study as the most common RFEs[51].
In addition, the almost non-existence of RFEs related to ICPC-2 chapter Z (social problems), which includes economic problems, food access problems and social security problems, does not reflect the social reality of the country as all of them are common problems in Brazil.
Table 3. Reasons accounting for 50% of all reasons for encounter in primary health care, excluding administrative reasons, as coded by the International Classification of Primary Care, Second Edition (Brazil, July–December 2016)
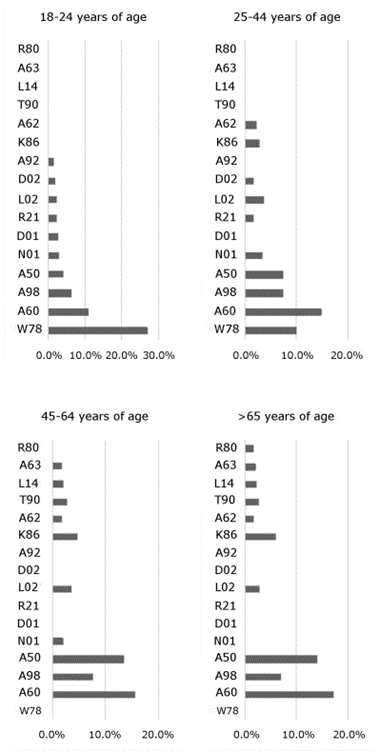
Regarding the frequency distribution of ICPC-2 codes according to age, sex and geographic region, there were differences and similarities that deserve a case-by-case analysis.
We draw attention to the little difference in RFEs between the five geographic regions of Brazil, given the known regional heterogeneity in morbidity.
More RFEs related to infectious diseases were expected in the north and north-east, while more RFEs related to non-communicable diseases were expected in the south and south-east.
This suggests that PHC units follow a national standard of care regardless of the local disease profile.
It is worth noting that our study described RFEs within the FHS rather than RFEs of the general Brazilian population.
With respect to the mean of 1.3 RFEs per patient, this is consistent with the results from national and international studies, which report a mean of 1–2 RFEs per patient[52] [53] [54] [55] [56] [57] [58] [59] [60] [61] [62] [63] [64] [65].
The rate of referrals (21.3%), however, was much higher than the rates reported in the national and international literature, ranging from 4% to 12%[66] [67] [68] [69] [70] [71] [72] [73] [74] [75].
Only one study conducted in India found a similarly high rate[76].
Our high rate of referrals may be related to some barriers faced by FHS teams, such as the impossibility of ordering some types of tests (e.g. echocardiogram) and poor infrastructure in PHC units, thus making FHS teams refer these patients elsewhere.
As for the rates of prescriptions and requests for investigations, there is a wide variation in their reporting and calculation methods in the literature, thereby hindering a proper comparison with the results obtained in the present study.
These results can be used as a reference for future research.
Figure 1.
Top 20 reasons for encounter in primary care according to sex as coded by the International Classification of Primary Care, Second Edition (Brazil, July–December 2016).
The main limitations of this study are its cross-sectional design and the period of only 2–3 days for interviews in each PHC unit, which hinders the analysis of seasonal variation in RFEs.
Also, the method of data collection may have led to measurement bias for three reasons:
(i) users were interviewed by an unknown person rather than by their primary care provider and, because of that, they may have not reported all their reasons (e.g. psychosocial problems);
(ii) the interview was performed shortly after the medical visit, and the reported reasons may have been influenced by the diagnosis made and
(iii) users were second-visit patients, which may have resulted in more reasons related to follow-up. Lastly, the results cannot be generalized to the Brazilian general population because only people enrolled in the FHS were interviewed.
A strength of this study is the random sample selection of physicians at the level of the PHC unit; only after that was the sample of patients selected consecutively.
The major strength, however, is its novelty as it is the first study to examine, at a national level, the RFEs in PHC in Brazil. Also, to the best of our knowledge, this is the first study of such magnitude to be conducted in Latin America.

Conclusion
This study opened the ‘black box’ of RFEs in PHC in Brazil.
Its main finding of only a few ICPC-2 codes accounting for half of the RFEs, as well as the high rate of referrals and of clinical-administrative and preventive codes highlight the inequities and limited comprehensiveness of PHC in Brazil.
Moreover, the homogeneity of the health needs observed here does not reflect the regional and socio-economic diversity of the country.
These results may serve as a basis for changes in the national PHC policy as they can foster discussions about the work practices of FHS teams and the urgent need to redefine the scope of PHC services in addition to contributing to the current debate on the quality of medical training necessary to provide this level of care.
It is essential to expand coverage and improve the clinical performance of Brazilian PHC teams.
Further research is warranted to clarify the similarity of RFEs across the different regions of the country and to address the reasons why healthy Brazilians are seeking medical care.
Transforming these findings into responses that can effectively reduce inequities, through public policies, will be the mission of national managers.
Figure 2. Top 10 reasons for encounter in primary care according to age group as coded by the International Classification of Primary Care, Second Edition (Brazil, July–December 2016).
References
See the original publication
About the authors & affiliations
Patricia S Chueiria,*, Marcelo Rodrigues Gonçalves b, Lisiane Hauser c, Lucas Wollmann d, Sotero Serrate Mengue b,c, Rudi Romanb, c, Milena Rodrigues Agostinho Rech e, Marcelo de Araújo Vianna Soares b, Jamily Pertileb and Erno Harzheimb, f
a School of Medicine,
Faculdade Israelita de Ciências da Saúde Albert Einstein, São Paulo,
b School of Medicine,
Universidade Federal do Rio Grande do Sul, Porto Alegre,
c Postgraduate Program in Epidemiology, TelessaudeRS, School of Medicine, Universidade Federal do Rio Grande do Sul, Porto Alegre,
d Community Health Services,
Grupo Hospitalar Conceição, Porto Alegre,
e School of Medicine,
Universidade de Caxias do Sul, Caxias do Sul and
f Secretary of Primary Health Care,
Ministry of Health, Brasília, Brazil.












