Health Foundation
Tim Horton, Tom Hardie, Shakira Mahadeva, Will Warburton
16 March 2021
Key points
- This long read explores the challenges of implementing health care technologies and investigates patient and staff experiences of technology during the first phase of the coronavirus (COVID-19) pandemic.
- It draws on learning from the Health Foundation’s programmes and YouGov surveys of over 4,000 UK adults and over 1,000 NHS staff conducted in October 2020.
- During the pandemic, there has been increased NHS use of both established and newer technologies to reduce face-to-face contact and manage demand.
- Around three-fifths (~60%) of UK adults who used the NHS during the early phase of the pandemic said that in doing so they used technology either in a new way or more than before.
- While technologies were rolled out with impressive speed, some aspects of implementation — such as evaluation, co-design and customisation — will necessarily have been shortcut, and will need revisiting after the emergency phase of the pandemic is over.
- Furthermore, many technologies were rolled out specifically to serve pandemic response objectives such as social distancing, so will need to be ‘reoriented’ and developed to serve wider quality and productivity objectives in future.
- Among members of the public and NHS staff who reported increased use of technology, the overwhelming majority said they had positive experiences — impressive given the severe pressure on the NHS.
- Slightly higher proportions of negative experiences were reported by those aged 55 and older, those with a carer and unemployed people, so it will be necessary to investigate what worked well, what did not and why, including from the standpoint of equity and digital inclusion.
- Around two-fifths (~40%) of the public and a third (~33%) of NHS staff surveyed said these technology-enabled approaches were ‘worse’ than traditional models of care.
- While this should not be taken as a long-term verdict — many of the same people also said their experience had made them feel more positive about using technology in future — it does highlight the need to develop and improve these approaches before ‘locking them in’.
- Through a refresh of the NHS long term plan and other national strategies, policymakers will need to support front-line teams to revisit aspects of implementation and ‘reorient’ technology-based interventions to serve longer term quality and productivity objectives.
- Central to this will be evaluating their impact on care quality and developing a vision of ‘what good looks like’.
- NHS staff surveyed highlighted the issues of ensuring adequate IT and equipment and sufficient staffing as among the top challenges for capitalising on recent technological progress.
- The forthcoming Spending Review and the next stage of national workforce strategies should explicitly address the NHS workforce, skills and infrastructure needed to exploit new and established technologies successfully beyond the pandemic.
FULL VERSION
The increased use of health care technology during the pandemic
Over the past year, the NHS has been through an extraordinary period of challenge and change. At the forefront of this has been the incredible effort and commitment shown by those in the health service in dealing with the impact of COVID-19. Also significant is the way services have had to rapidly adapt to the new reality of delivering health care in a pandemic.
Some of the most notable developments have involved greater use of technology to reduce face-to-face contact and help manage demand.
This includes increased use of established technologies and platforms:
- more phone and video consultations in primary and secondary care;
- wider use of devices and apps for remote working at home, including as part of virtual wards;
- increased use of the Electronic Prescribing Service; and
- wider use of the NHS website and
- NHS 111 online.
COVID-19 has also accelerated the uptake of newer technologies and platforms, such as
- the NHS app for appointment booking and patient record access;
- the rollout of video conferencing software to enable remote working and collaboration, including more professional-to-professional support for clinical decision-making;
- and the use of AI-driven image analysis to help diagnose and monitor the progression of COVID-19.
Though the NHS has previously attracted criticism for being slow to adopt and rollout new technologies, recent developments show it can do so at impressive pace and scale when conditions allow and staff are empowered to make change happen.
Recent Health Foundation research on the service shifts accelerated by COVID-19 highlights some key factors that enabled these developments.
- A significant reduction in services released staff from other duties to concentrate on implementing and delivering change.
- A sudden, urgent common purpose simplified decision making and made it easier to collaborate and work across organisational boundaries.
- And important moves by national bodies supported change on the ground; for example, producing information governance guidance and procuring licenses to support the rollout of virtual consultations, publishing procurement frameworks, and purchasing equipment to support home monitoring.
Sustaining technology use beyond the pandemic
While COVID-19 has driven these recent technological steps forward, it is notable that several of them — such as greater use of video consultations or devices and apps for home monitoring — have nevertheless been longstanding NHS objectives whose uptake has been accelerated by the pandemic response.
Along with health systems around the world, there are ambitions for the NHS to make greater use of technology to improve quality and efficiency. And there are high hopes, including those voiced by Secretary of State Matt Hancock in summer 2020 and in the plans set out in the white paper in England in February 2021, that recent developments will help usher in an era of more technology-enabled health care beyond COVID-19 — a potentially positive legacy from a difficult time.
This long read aims to inform this agenda by investigating patient and staff experiences of the increased use of technology during the first phase of the pandemic (defined here as March to October 2020) and by exploring some of the challenges of implementing health care technologies in practice.
Drawing on two YouGov surveys of UK adults and NHS staff conducted in October 2020, and on learning from the Health Foundation’s programmes, we also ask what will be required to embed and sustain recent developments for the long term — offering lessons for providers and policymakers.
Mapping the increased use of technology
In our survey of UK adults (total sample size 4,326), conducted 26–28 October 2020, around twofifths of respondents (39%) said that they had either ‘received NHS care for any health condition’ or that they (or their carer) had ‘communicated with the NHS about their health’ since the first lockdown began at the end of March 2020. And nearly all of this group (97%) said they had used technology in some way in doing so (defined broadly to include phone, video link, web, email, messaging, apps and medical devices).
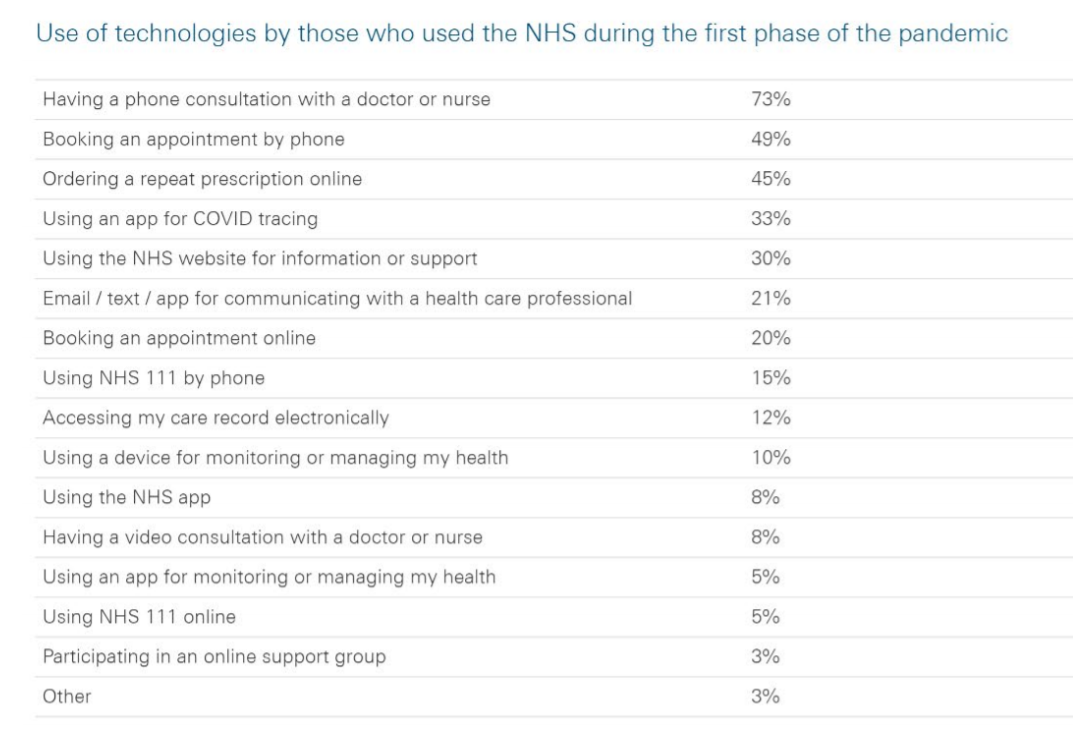
Table 1 lists the technologies that respondents used. Phone consultations dominate, followed by some well-established uses of technology, such as booking appointments by phone or using the NHS website. But some emerging or less established uses of technology, including several explicitly promoted by national bodies, are also apparent. For example, accessing care records electronically, devices for home monitoring, video consultations, and the NHS app.
Table 1
For some, the use of these technologies during the pandemic would have been nothing out of the ordinary — part of an existing pattern of interaction with the NHS. But for many others, it represented an increased use of technology — part of an explicit NHS strategy, described above, for greater use of technology to deliver services during the pandemic.
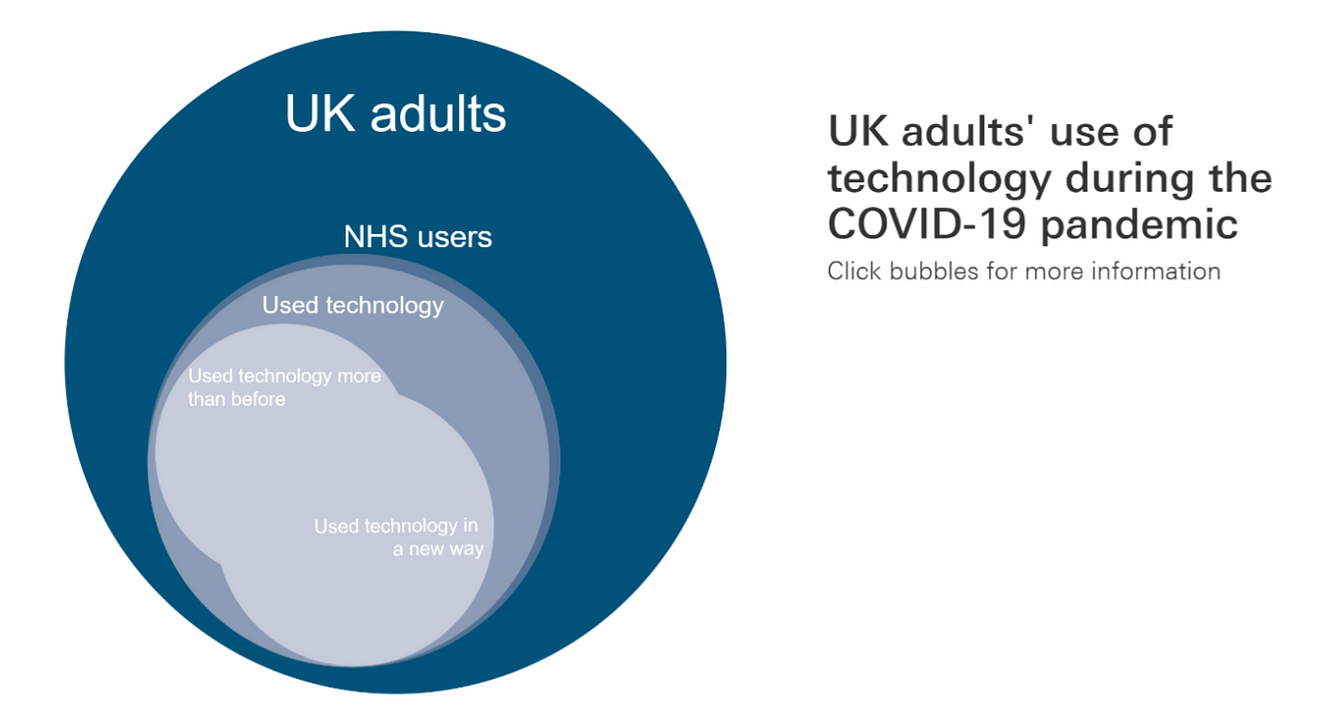
To identify the subset of people for whom this represented an increased use of technology, we asked those who had used technology for health care purposes whether they had used any of these technologies in a new way or for the first time during this phase of the pandemic; 40% said ‘yes’. We also asked whether they had used technology in interacting with the NHS more or less than before COVID-19, or about the same; 51% said ‘more’.
As shown in the diagram below, there was substantial overlap between those using technology in a new way and those using it more than before, meaning that in total 60% of those who used technology for health care during this phase of the pandemic either used it in a new way or more than before. It was this group — amounting to around a fifth (22%) of the population as a whole — that we consider here to have been part of the increased use of technology during the first phase of the pandemic and whose experiences we set out to investigate further.
Figure 1
Increased use of technology by NHS staff
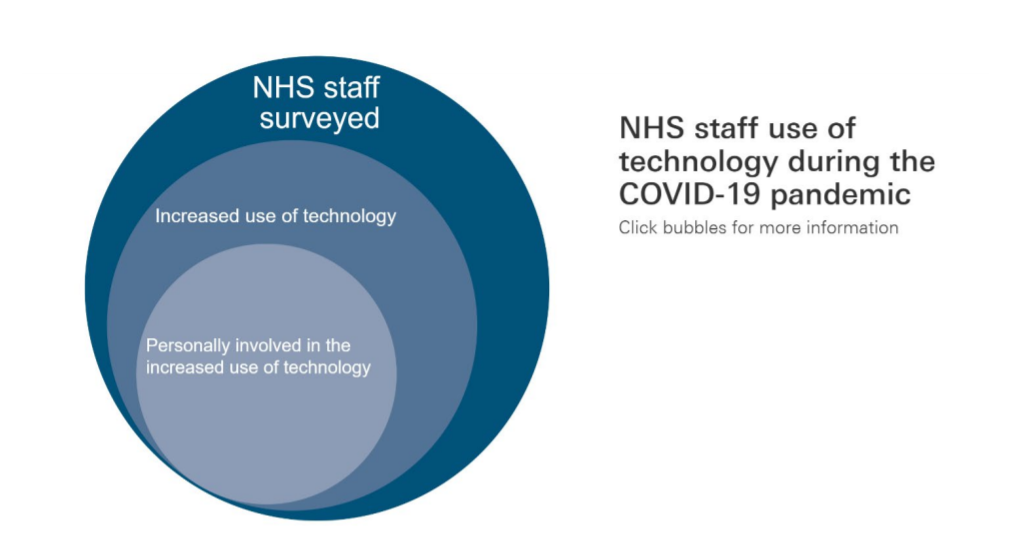
In our survey of NHS staff (total sample size 1,413), conducted between 23 October and 1 November 2020, just over four-fifths of respondents (82%) said their organisation had increased its use of technology to some extent during this period. And half of this group (51%) said they had been personally involved in this increased use of technology, amounting to just over two-fifths (42%) of NHS staff surveyed.
Figure 2
In the next part of our survey, we set out to explore the experiences of those reporting increased use of technology for health care during this first phase of the pandemic. Before describing this, however, we first explore some challenges that may have been created by the rapid implementation of technology during the pandemic.
Challenges created by the rapid implementation of technology during the pandemic
While the speed at which technologies have been rolled out during the pandemic has been impressive, the context and pace of these changes also pose challenges.
First, it is likely that having to implement changes rapidly and under the constraints of a national health emergency means that some aspects of implementation will, understandably and necessarily, have been rushed or shortcut.
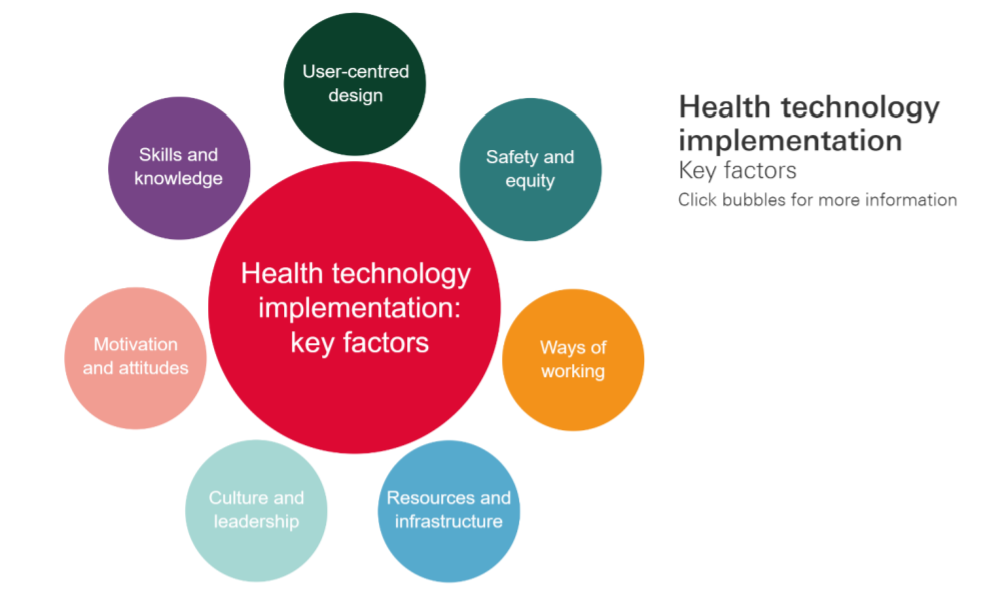
Implementing health care technology well can be a challenge at the best of times. Though people often focus on the technology in isolation, it is making it work in a real-world setting that enables the NHS and patients to derive the benefits. Doing this effectively depends on several factors, summarised in Figure 3. These include skills and knowledge; motivation and attitudes; user-centred design; ways of working; safety and equity; resources and infrastructure; and culture and leadership. It is not difficult to see how rolling out changes during a pandemic may have created challenges in each of these areas.
Figure 3
One particularly pressing challenge is the limited evaluation of the changes seen in recent months. The learning so far has revealed some of the complexities. For example, the Q Community’s work with teams implementing video consultations during the pandemic surfaced both pride about the progress made, but also concerns about accessibility and digital exclusion. Before decisions can be made about the shape of future provision, more work will be needed to understand the impact changes are having for different groups of patients.
Furthermore, the pace of change and the imperatives of managing the pandemic have meant that many changes happened without much engagement with patients, even though emerging evidence suggests that the views of patients and professionals on remote care, for example, may not be the same.
So as we move beyond the emergency phase of the pandemic there will be a need to revisit aspects of implementation in order to evaluate these technology-enabled approaches and develop them further. Particularly important will be recognising that adopting new innovations effectively requires more than simply putting them in place — ongoing work may be required to adapt and tailor them to local context and generate optimum outcomes. In many cases, the necessity during the pandemic might have been to get ‘good enough’ versions of new approaches working, but few teams will have had extensive opportunities for testing, iterating and refining them.
Adapting approaches to serve broader objectives in future
It is also important to recognise that the reason COVID-19 turbo-charged the rollout of some longstanding NHS technology ambitions is that they were able to support pandemic response objectives, such as social distancing or demand management. But in future we will want these technologies to serve the broader quality and productivity objectives for which they were originally conceived, as well as new objectives as they emerge.
Take video consultations. Before COVID-19, video consultations were seen as a way to improve patient access and convenience, clinical productivity and use of the NHS estate. During the pandemic, by contrast, they have been put in place primarily to achieve social distancing (which they automatically do). But just because providers have implemented video consultations to achieve social distancing, it does not necessarily mean that they have yet achieved the wider quality objectives video consultations will need to serve over the long term.
This matters because the objectives of an innovation are central to how it is implemented and used. If a technology implemented to serve one objective is subsequently repurposed to serve another, this may have implications for how it is deployed. For example, the processes and workflows required to derive the intended benefits from it, the case made for the technology and the consensus around it, defining considerations of safety, and so on. Good implementation for one objective does not necessarily imply good implementation for another, and so work may be required to ‘reorient’ the innovation towards serving its new objectives. This, in turn, will require clarity on ‘what good looks like’ from the perspective of the various stakeholders involved.
In summary, rapid implementation of technology interventions during the pandemic may have created a range of issues that will need addressing in order to modify, improve, embed and sustain them for the long term.
Patient and staff experiences of using technology
In our surveys, we asked those members of the public and NHS staff who had reported increased use of technology for health care during the COVID-19 pandemic some questions about their experiences.
- Were patient and staff experiences of using technology positive or negative?
- How did these technology-enabled approaches compare with more traditional ways of delivering care?
- How did patient and staff experiences of technology make them feel about using these approaches in future?
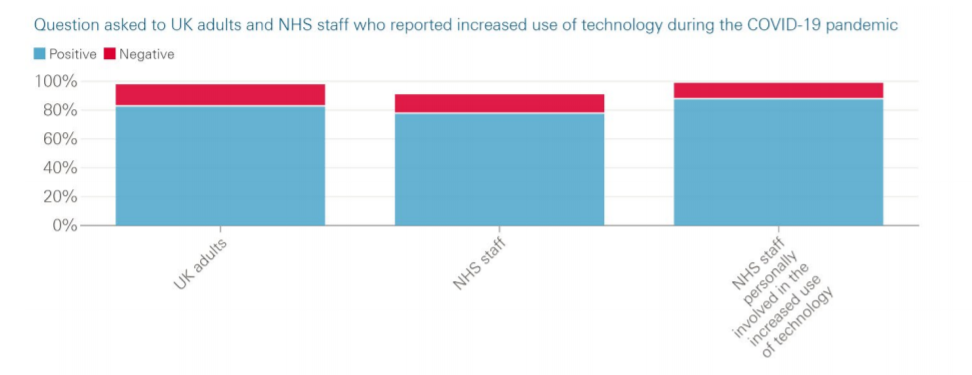
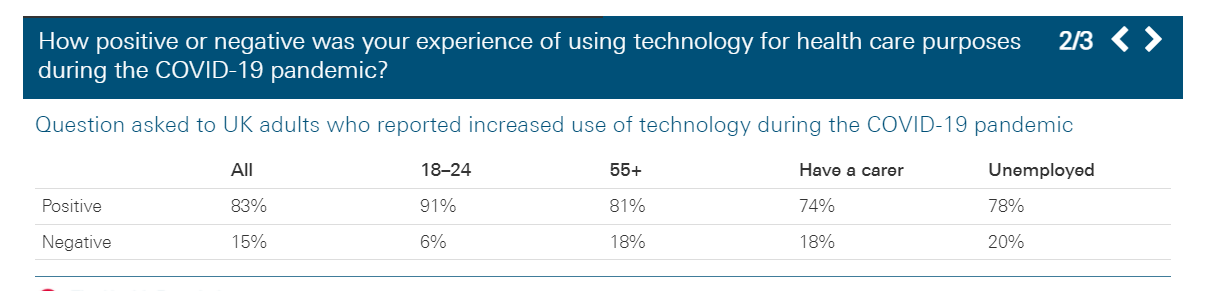
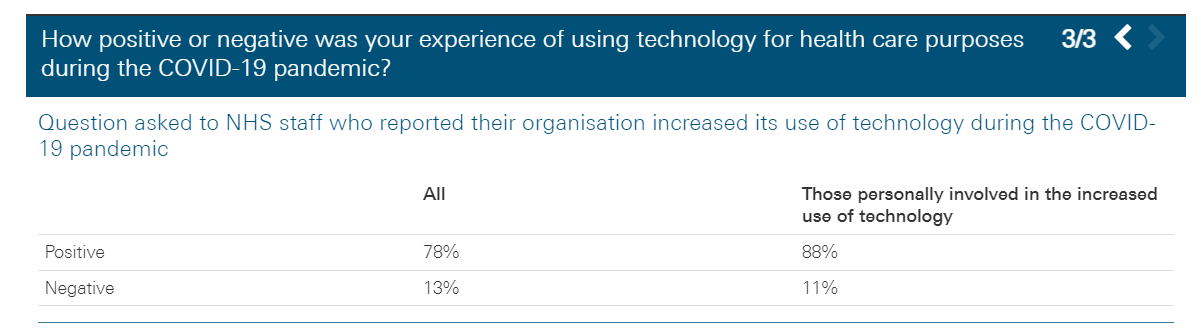
1.Were patient and staff experiences of using technology positive or negative?
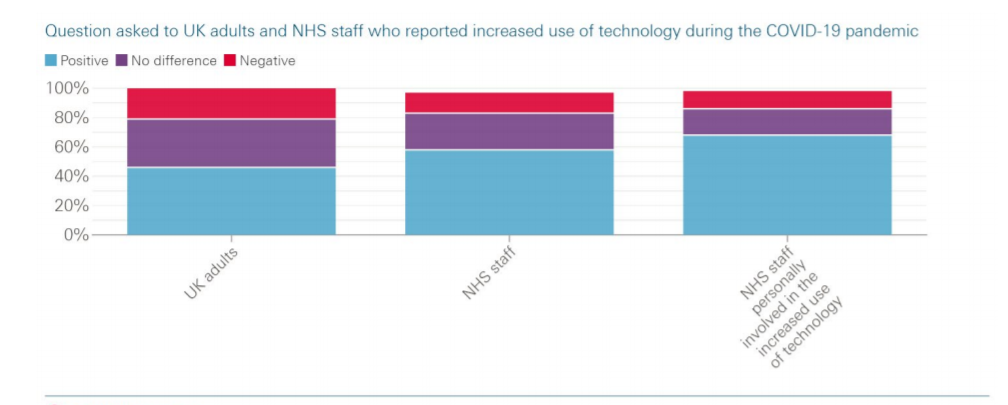
As shown in the table below, the vast majority of both public and NHS staff respondents reported positive experiences of the increased use of technology (and net positivity was even higher among NHS staff who had been personally involved in their organisation’s increased use of technology). This is an encouraging finding given the NHS has been under severe pressure during this period and it will be important to understand what went well and why to inform future technology deployment.
Age is sometimes cited as a factor affecting attitudes to technology and this was evident in our public survey, with a slightly larger proportion of younger people reporting positive experiences than the population as a whole and a slightly larger proportion of those age 55 and older reporting negative experiences. Furthermore, slightly larger proportions of people with a carer and unemployed people reported negative experiences (albeit within the context of large majorities of all these groups reporting positive experiences). It will be important to investigate the reasons for these differences, particularly from the standpoint of equity and digital inclusion, and how they can be addressed.
Figure 4
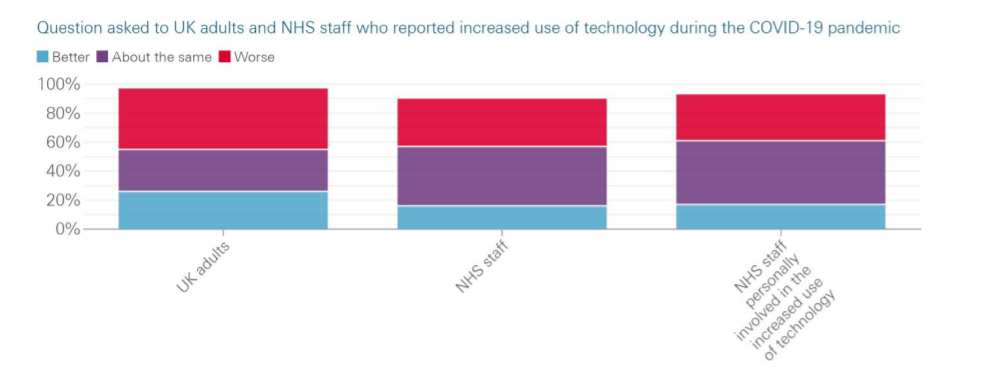
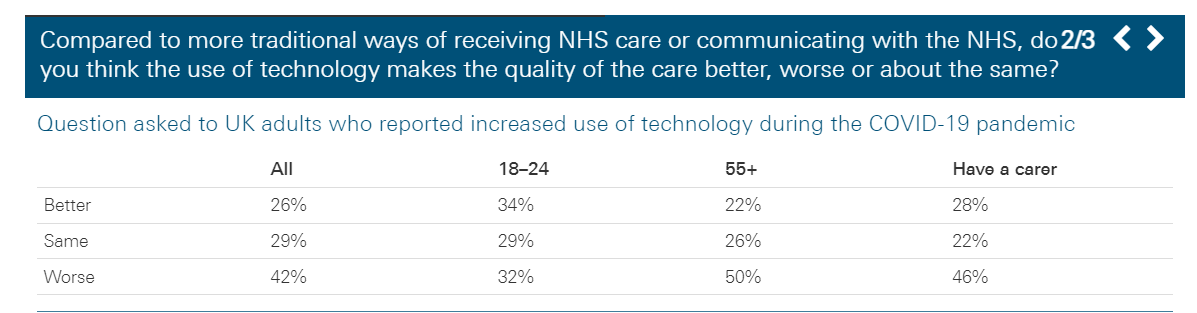
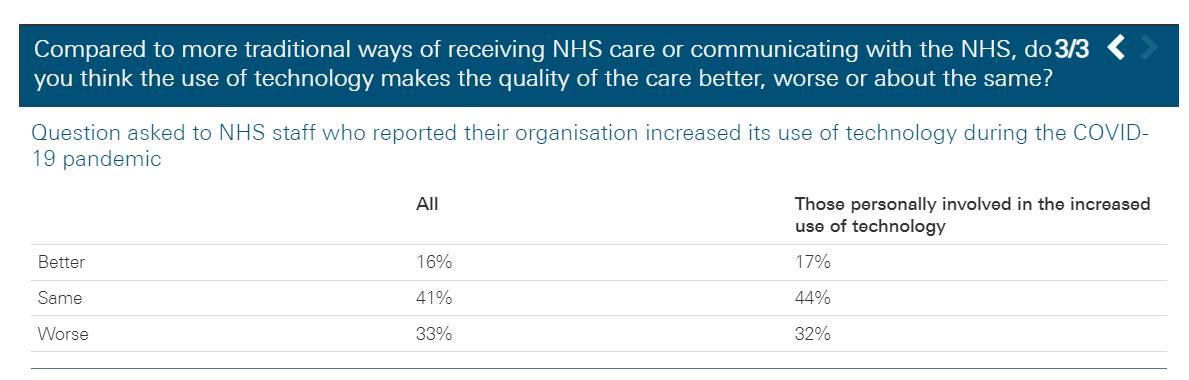
2. How did these technology-enabled approaches compare with more traditional ways of delivering care?
Here, the results present a more mixed picture. Reflecting on their experience during the COVID-19 pandemic, just over two-fifths (42%) of the public and a third (33%) of NHS staff surveyed said these technology-enabled approaches were worse than traditional ways of delivering care. But caution is required in interpreting this. Many of these approaches will have been rolled out in the first instance not to improve services but to maintain them during a public health emergency. As discussed, making technology-enabled approaches serve longer term quality ambitions may require further development.
Furthermore, for some kinds of technology interventions, such as virtual consultations, maintaining quality while realising the benefits of remote care could itself be seen as a legitimate objective. From this perspective, a majority of the public saying their experience was either the same or better would be encouraging.
What these findings do suggest, however, is that once the NHS moves beyond the emergency phase of the pandemic, there will be further work to do on assessing and improving some of these technology-enabled approaches. Notably, half of those aged 55 and older and nearly half of those with a carer — groups that may have higher need for health care — thought technology-enabled approaches, as they experienced them during the first phase of the pandemic, were worse compared with traditional ways of delivering care.
Figure 5
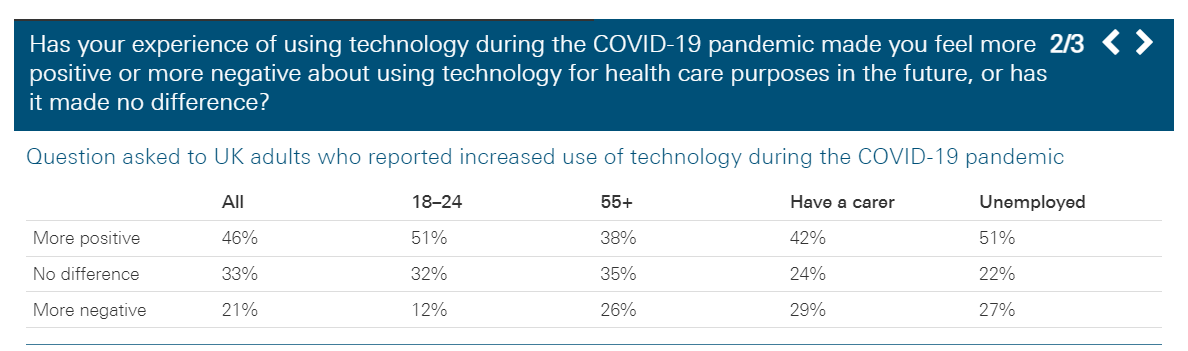
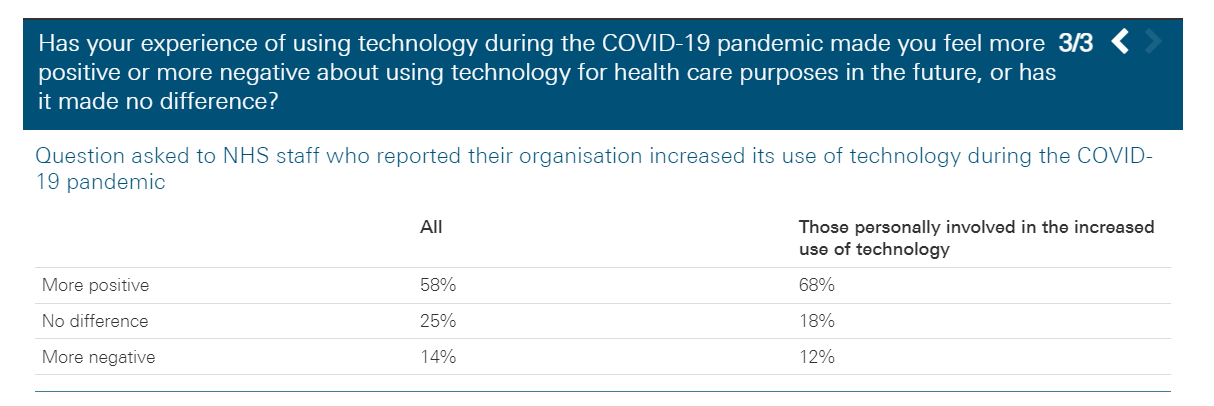
3. How did patient and staff experiences of technology make them feel about using these approaches in future?
Among both the public and NHS staff surveyed, those who said their experiences had made them feel more positive about using these technology-enabled approaches in future significantly outweighed those who said it had made them feel more negative. This suggests that the mixed pattern of responses to the previous question does not amount to a rejection of using these approaches in future. For example, while half of those aged 55 and older thought technology-enabled approaches during the COVID-19 pandemic were worse than traditional models of care, only a quarter said their experience had made them feel more negative about using these in future. Nevertheless, a significant minority did say their experiences had made them feel more negative about using technology in future (21% of all those who reported increased use of technology during the COVID-19 pandemic, rising to 29% for those with a carer), so it will be important to investigate and learn from what has happened in these cases.
Figure 6
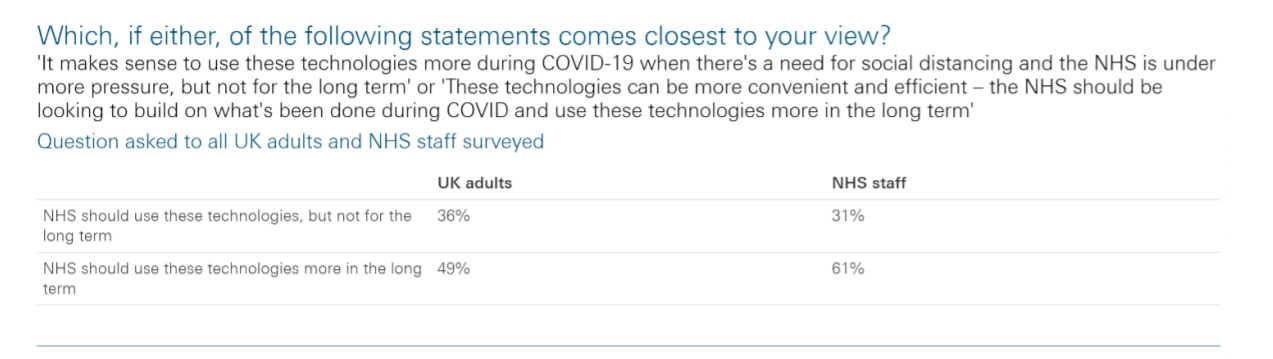
Beyond exploring the views of those who had used technology more during the COVID-19 pandemic, we also wanted to investigate wider public and NHS staff attitudes to using these kinds of technology-enabled approaches in future. When asked to choose between two competing statements, 49% of the public and 61% of NHS staff surveyed agreed that the NHS should be looking to build on developments during the COVID-19 pandemic and use technology more in the long term. By contrast, 36% of the public and 31% of NHS staff surveyed thought that greater use of technology made sense during the pandemic but was not something for the long term.
So the balance of opinion is tentatively encouraging for proponents of greater use of health technology. However, it is clear that a significant minority of those surveyed were unconvinced about the long-term use of these technology-enabled approaches. This highlights the need for NHS leaders to engage with the public and NHS staff to understand these differing views, make the case for future changes, and help build awareness and confidence about technology-enabled care.
Table 2
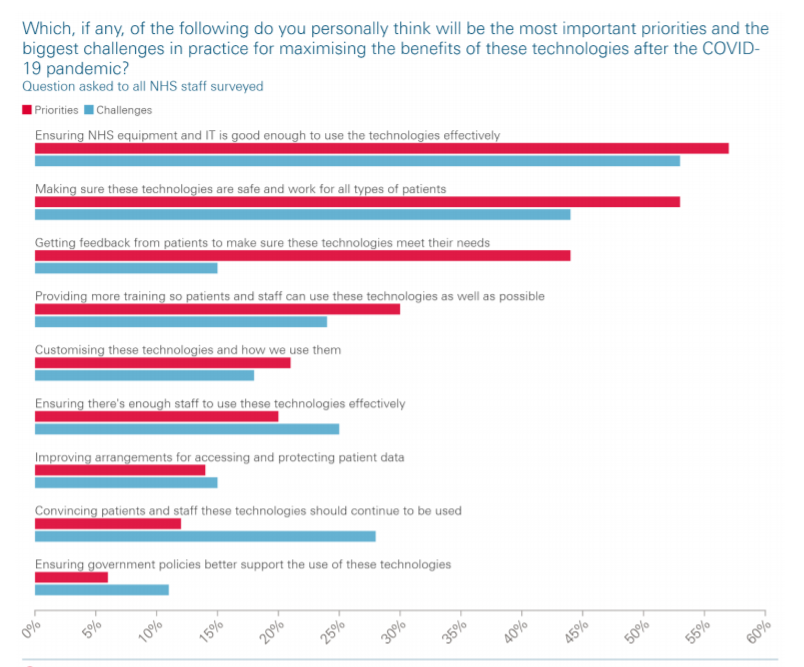
Finally, we explored NHS staff views on both the most important priorities and the biggest practical challenges for building on and embedding recent technological developments after the pandemic. When presented with a list of issues, the same two ranked highest as both priorities and practical challenges: ensuring that NHS equipment and IT is good enough to use technologies effectively, and making sure technologies are safe and work for all types of patients. This provides a strong signal for policymakers and organisational leaders to consider how they can best support this agenda. The next highest ranked priority was getting feedback from patients to make sure these technologies meet their needs, while the next highest ranked challenge was convincing patients and staff that these technologies should continue to be used.
Figure 7
Lessons for deploying health care technology after the pandemic
What is going to be required to learn from, build on and embed some of the positive technology enabled developments we have seen during the COVID-19 pandemic? And how can the benefits be maximised?
In some quarters, the progress seen has led to talk of ‘locking in’ recent changes — based on the view that COVID-19 has sped up the rollout of some major innovations and with the job now done they can be preserved for the long term. The recent white paper in England, for example, sets out the aim to ‘make permanent the innovations that COVID-19 has accelerated’. But the issues highlighted here and in our survey suggest that the job is not yet fully done and further work is needed to evaluate and build on recent progress.
Priorities for NHS provider organisations
- Revisit aspects of development and implementation
- Think about longer term objectives
- Create the right environment for adopting and using technology
1.Revisit aspects of development and implementation
Front-line teams will need to revisit aspects of development and implementation that may have been shortcut during the COVID-19 pandemic.
This could include rapid steps to put in place more local evaluation, to ensure new approaches are safe and work for all groups of patients. Identifying issues around digital exclusion and putting in place mitigating actions or alternatives to ensure technologies are not creating or widening health inequalities will be particularly important.
It might also include more consultation and co-design with patients and staff to ensure new approaches are user-centred. Indeed, there may still be a need to develop and secure consensus about the future role of some technology-enabled approaches that were perhaps taken as a given during the pandemic.
Other implementation issues may need revisiting too, such as training needs or activities like customising technologies and optimising ways of working, which begin at implementation but subsequently become part of the iterative work of continuous improvement.
In short, though the speed at which technologies have been rolled out during the pandemic has rightly been praised, more work is going to be required to get the best out of them for the long term.
2. Think about longer term objectives
Technology-enabled approaches will need to be re-oriented towards serving longer term quality and productivity objectives beyond the pandemic.
For example, how can the recent deployment of devices for home monitoring develop from a useful way of monitoring health during a time of social distancing into a way of better supporting patients to manage their own health? How can the increased use of video consultations develop from a way of delivering health care at a time of reduced social contact into the vision for improving patient access, clinical productivity and use of the NHS estate outlined in the NHS long term plan? And how can we go beyond simply ensuring new technology-enabled approaches do not widen health inequalities towards the much more ambitious goal of harnessing the power of technology to ‘level up’ on health and make a particular difference for those who experience poorer outcomes? Changes such as these may require evolution of the interventions in question to focus on these longer term objectives.
3. Create the right environment for adopting and using technology
Leaders of organisations and systems providing NHS care have a crucial role to play in creating a conducive environment for adopting and sustaining innovation and technology. This includes engaging with their workforce to build a shared vision around technology-enabled care, and setting out how new uses of technology align with wider organisational strategy and values.
More specifically, organisational leaders will need to support their workforce in reorienting and embedding new technologies rolled out during the pandemic by empowering them to design and test changes and allowing them the time and space to do so. This will happen most effectively if there is a learning culture within the organisation or system with a commitment to continuous improvement. Our poll also highlights the need to ensure the right digital infrastructure and staffing are in place.
Priorities for policymakers and national leaders
- Engage and consult the public and NHS staff
- Evaluate impacts before ‘locking in’ new approaches
- Help providers to focus on longer term objectives
- Address the NHS’s workforce, skills and infrastructure needs in relation to technology
1.Engage and consult the public and NHS staff
NHS leaders in the four UK nations should support public engagement exercises and consultation on the future of technology in health care, ensuring representation from underserved groups and patients with complex needs.
There were many positive findings from our surveys, but it is also clear that not everyone had a good experience of using technology during this period. Research is needed to understand why a minority of the public and staff reported negative experiences and why some — particularly older people and those with a carer — rated technology-enabled approaches as ‘worse’ than traditional ways of delivering care, along with evidence-based actions to address problems and concerns.
It is also clear that the NHS has not yet ‘sealed the deal’ with the public as a whole on technology-enabled health care, with a significant minority appearing sceptical about its use beyond COVID-19. So there needs to be a meaningful conversation with the public and NHS staff to understand and address concerns, as well as to raise awareness and build confidence in these approaches. This will be particularly important for public-facing technologies, such as online appointment booking or mobile health apps, which potentially affect all users of the NHS.
2. Evaluate impacts before ‘locking in’ new approaches
Rather than rushing to lock in recent technological developments, policymakers should first ensure proper evaluation of their impact on the quality of care, including on health outcomes and patient and staff experience, and whether there have been any unintended consequences.
While the overwhelming majority of respondents to our poll found their experience of using technology during the first phase of COVID-19 positive, our poll also raised questions about the impact and quality of these approaches that requires further evaluation. In particular, there is a need to better understand what and who these technologies do and do not work for, rather than thinking of blanket, one-size-fits-all applications of technology. This means having a strong priority within NIHR programmes for such evaluations, including through approaches that can produce rapid results, such as the work currently underway by the BRACE and RSET teams to evaluate COVID-19 virtual ward models.
3. Help providers to focus on longer term objectives
Through a refresh of the NHS long term plan, and equivalent strategies in the devolved nations, policymakers should put in place a strategy of ‘reorientation’ — helping providers to develop and optimise the use of recent technological innovations to meet longer term quality and productivity goals.
This involves assessing which approaches are capable of serving longer term quality and productivity objectives — as has been happening through the Beneficial Changes Network in England, including work commissioned from the AHSNs and ARCs to evaluate and prioritise promising changes at a regional level — and then supporting providers to develop these approaches to achieve this. There is also growing awareness that critical to doing this will be understanding ‘what good looks like’ when it comes to technology-enabled health care.
At a national level, this work will benefit from greater alignment of thinking on technology and quality improvement, as well as ensuring that centrally-led programmes do more to bring technology and improvement communities together in practice.
4. Address the NHS’s workforce, skills and infrastructure needs in relation to technology
The forthcoming multi-year Spending Review and the next stage of national workforce strategies should explicitly address the workforce, skills and infrastructure needs of the NHS in order to exploit new and established technologies successfully over the long term.
Ensuring the NHS has adequate IT and equipment to make the most of new technologies was the top priority in our survey of NHS staff. Yet we know that capital spending in health care was significantly lower than the OECD average throughout the 2010s, resulting in a growing maintenance backlog. So recent increases in capital spending, only partly a consequence of COVID-19, will need to be maintained if the NHS is to keep pace with developments.
In addition, the staffing shortfall will need to be addressed if the NHS is to make the most of the opportunities technology presents.
Furthermore, while much support has been provided to more technologically advanced NHS providers in recent years, there is a need to focus on building the capability of less advanced providers as well. It is therefore important that funding recently committed in England and Wales, as well as future funding allocations, can be used to assist these organisations.
Looking ahead
Over the coming months, the Health Foundation will be playing its part in supporting this agenda.
Our Q Exchange programme is funding 30 front-line teams to embed and sustain positive changes that have happened during the pandemic, including several projects focused on virtual care.
Our Adopting Innovation programme will be supporting NHS providers and local health systems to create the conditions for more effective take-up of innovations and technologies.
And we are supporting research projects to learn from the roll out of remote and asynchronous consultations before, during and after the pandemic, including studies led by the University of Oxford and Aberdeen University.
Alongside this, the Improvement Analytics Unit, a partnership between the Health Foundation and NHS England and NHS Improvement, is evaluating COVID-19 oximetry (the use of small devices for measuring blood oxygen level) at home.
And THIS Institute is undertaking a variety of projects to develop clarity on ‘what good looks like’ for remote care in areas such as antenatal services, mental health, heart failure and COPD.
As we emerge from the shadow of the pandemic, the NHS faces an important moment, where the choices made will determine not only the success or failure of recent technological steps forward, but also how fast and effectively the NHS will be able to grasp technological opportunities in future.
Getting it right will mean seizing the moment to take stock and understand how these technology-enabled approaches can work to improve care for everyone, and then setting them on the right path to get there.
Despite the challenges, with coordinated action at all levels of the health service, there is a real opportunity to build on recent progress during the pandemic and shape a positive technology legacy for the future.
Contents
- Key points
- The increased use of health care technology during the pandemic
- Mapping the increased use of technology
- Challenges created by the rapid implementation of technology during the pandemic Patient and staff experiences of using technology
- Lessons for deploying health care technology after the pandemic
- Supporting information
About the authors
- Tim Horton (@timjhorton) is Assistant Director (Insight & Analysis) at the Health Foundation
- Tom Hardie is Improvement Fellow at the Health Foundation
- Shakira Mahadeva is Improvement Intern at the Health Foundation
- Will Warburton is Director of Improvement at the Health Foundation
This long read was published originally on 16 March 2021 at the following address: www.health.org.uk/publications/long-reads/securing-a-positive-health-care-technology-legacyfrom-covid-19












