A cross-sectional survey of 88 countries
BMJ Open
Ian Bates ,1,2 Sherly Meilianti ,1,2 Lina Bader,2 Rishi Gandhi,1 Rachael Leng,1 Kirsten Galbraith 2,3
22 April 2022
e-lhf
ABSTRACT
Objective
Advancing the pharmacy workforce contributes to strengthening primary healthcare and accelerating progress towards universal health coverage.
This study aimed to identify key enablers to support policy development for national pharmacy workforce advancement.
Design
A cross-sectional country-level questionnaire was distributed from July 2018 to March 2019.
Setting
National-level or country-level pharmacy workforce development policy.
Participants
Professional leadership associations and national agencies of the International Pharmaceutical Federation (FIP). The FIP global database included 129 countries.
Measures
The questionnaire was designed to collate data on the scope of advanced and specialist practice in respondent countries. Multiple correspondence analysis and subsequent cluster analysis were conducted to explore the associations and patterns of country-level attributes of systems in place for the pharmacy workforce advancement in order to develop a general transnational model for country-level advanced practice development.
Results
Eighty-eight countries (68.2% response rate) responded to the questionnaire.
Factors that enhance and contribute to advanced practice policy development include the country’s socioeconomic factors and the availability of national practice advancement concepts.
The essential advancement concepts include the availability of framework and professional recognition systems, programmes assisting advanced practice development and workforce advancement and recognition opportunities.
Cluster analysis identified three clusters of country respondents.
- First cluster included low-income and middle-income with poor pharmacy advancement implementation,
- second cluster included a higher socioeconomic status with weaker pharmacy workforce advancement implementation and
- third cluster included upper middle-income to high-income countries and high rates of pharmacy advancement implementation.
Conclusion
The key factors identified in this study can be used to support a transnational approach to pharmacy workforce advancement.
The three clusters identified highlighted that workforce advancement was not an exclusive trait of higher-income countries.
Lessons from countries that have already adopted concepts of advancement in pharmacy practice could be adopted to other countries to accelerate the progress of advanced practice globally.
Lessons from countries that have already adopted concepts of advancement in pharmacy practice could be adopted to other countries to accelerate the progress of advanced practice globally.
Introduction
WHO predicts a global shortfall of healthcare workers of around 18 million by 2030, with the biggest impact in low-income and middle-income countries (LMICs).1
Investing in building health workforce capacity is an essential (and non-contestable) factor for enhanced delivery of primary healthcare (PHC) and to achieve universal health coverage (UHC).2
WHO predicts a global shortfall of healthcare workers of around 18 million by 2030, with the biggest impact in low-income and middle-income countries (LMICs) …
Investing in building health workforce capacity is an essential (and non-contestable) factor for enhanced delivery of primary healthcare (PHC) and to achieve universal health coverage
Strategies defined by WHO for tackling this global issue include implementing PHC programmes, country-level tools for ensuring UHC and a global campaign to advocate for strengthening the global health workforce.3
Strategies defined by WHO for tackling this global issue include implementing PHC programmes, country-level tools for ensuring UHC and a global campaign to advocate for strengthening the global health workforce.3
The pharmacy workforce is the third-largest global regulated health workforce. In nearly all countries, the pharmacy workforce is the most accessible health workforce for civil society and, as such, is at the forefront of healthcare service delivery.4 5
There is a need to describe and recognise an advanced practice role for pharmacists, in conjunction with enhancements in workforce competencies.6 7
The pharmacy workforce is the third-largest global regulated health workforce.
In nearly all countries, the pharmacy workforce is the most accessible health workforce for civil society and, as such, is at the forefront of healthcare service delivery.4 5
There is a need to describe and recognise an advanced practice role for pharmacists, in conjunction with enhancements in workforce competencies.6 7
As populations worldwide are living longer, they do so with additional and often complex comorbidities, with increases in the use and complexity of medicines and therapeutic strategies, most often within more complex multidisciplinary team environments.
Trends such as pharmacist prescribing, in addition to therapeutic specialisation, are significant workforce development needs due to the increasing complexity of medicines management for long-term conditions, communicable disease and preventative healthcare.8
Trends such as pharmacist prescribing, in addition to therapeutic specialisation, are significant workforce development needs due to the increasing complexity of medicines management for long-term conditions, communicable disease and preventative healthcare.
Having national professional recognition mechanisms in place has shown benefits for the enhancement of career pathways, enhancement of service development and delivery (linked to career pathway) and professional esteem.9 10
It is also imperative to have workforce development mechanisms available to directly support the realistic achievement of PHC outlined in the Astana Declaration.8
United Nations (UN) indicator target 3.c concerning a ‘substantially increase of health financing and recruitment, development training and retention of health workforce’, and pharmacists have been recognised as part of the health workforce (in addition to physicians, nursing personnel, midwifery personnel and dentists).5
United Nations (UN) indicator target 3.c concerning a ‘substantially increase of health financing and recruitment, development training and retention of health workforce’, …
… and pharmacists have been recognised as part of the health workforce (in addition to physicians, nursing personnel, midwifery personnel and dentists).5
The International Pharmaceutical Federation (FIP), the global professional leadership body, supports global health through advancing pharmaceutical practice, sciences, workforce and education.11
In 2016, the FIP started a programme of global workforce transformation to meet the evolving complex health needs of populations, with the introduction of Pharmaceutical Workforce Development Goals.5 12
This has recently been further extended to incorporate practice transformation and innovation through pharmaceutical science, with new goals for practice and science merged with existing goals for workforce and education, under the umbrella of the more comprehensive FIP Development Goals (FIP DGs).13
FIP DG 4 supports the concept of ‘advanced and specialist development’, including a recommendation in the workforce element that ‘countries/territories and professional member organisations should have education and training infrastructures in place for the recognised advancement of the pharmacy workforce as a basis for enhancing patient care and health systems deliverables’.13
FIP DG 4 supports the concept of ‘advanced and specialist development’, including a recommendation in the workforce element that ‘countries/territories and …
… professional member organisations should have education and training infrastructures in place for the recognised advancement of the pharmacy workforce as a basis for enhancing patient care and health systems deliverables’.
This goal sets out to ensure that pharmacy advancement and specialisation is recognised and supported in all sectors of pharmacy practice, including primary healthcare, where pharmacists serve as a first point of contact for many patients and local communities.
To support the achievement of this goal, the FIP has developed a validated tool, the FIP Global Advanced Development Framework, to support the professional development and recognition of the pharmacy workforce at the individual, institutional and national level.14
In 2015, FIP conducted the first global survey to identify the status of advanced practice initiatives across countries.9 10 15
Across 48 countries, this study found significant variations within terminology and definitions (scope of practice) of advanced practice and specialisation.10 15
The survey also reported variations between countries in professional recognition systems for the advancement of practice, including development, definitions and conduct.9 10
Some countries had developed competency development frameworks specific to the advancement of pharmacy practice, demonstrating they are moving towards developing structures and guidelines for advancing and recognising practice beyond the early career or foundation level.9 10 15
Despite the range of data gathered from this original survey, there remained unanswered questions regarding factors associated with the successful implementation of advanced practice pathways.
This paper presents a significant data extension with a larger and more diverse sample base of 88 countries that aims to identify key enablers to support policy development for national pharmacy workforce advancement.
Based on the key enablers or attributes identified, the authors then developed a global template for realistic and impactful workforce advancement in a translation context.
This global template is intended to be used to support countries in assessing and evaluating their countries’ needs and is particularly aimed at LMICs.
This study will aid in identifying the support needed for countries wishing to introduce local advancement pathways for the pharmaceutical health workforce.
The generation of an evidence base for successful implementation of advancement initiatives will enable an escalation of the processes for developing a global advanced health workforce to provide enhanced healthcare globally.

Methods
See the original publication
Results
Multiple correspondence analysis
The discrimination measures show correlations between clusters of variables and dimensions.
A relatively large discrimination value for a variable along a dimension indicates a greater influence along with the dimension.23
Figure 1 shows the discrimination measures plot for each variable of the proposed MCA model.
Variables marked with blue dotted lines (variables A–J) have larger discrimination coordinates along the abscissa (dimension 1).
These variables tend to be variables that are subject to policy control in terms of workforce development (ie, can be altered by policy innovation) and are related to conceptual attributes for the advancement of practice; we identified dimension 1 as ‘conceptualisation of advanced practice’.
Variables marked with red dotted lines (variables K–O) have statistical influence along the ordinate axis (dimension 2).
These variables (such as pharmacist density, World Bank class) represent the country-level socioeconomic or demographic attributes and tend to be more resistant to policy change; we identified dimension 2 as ‘socioeconomic factors’.
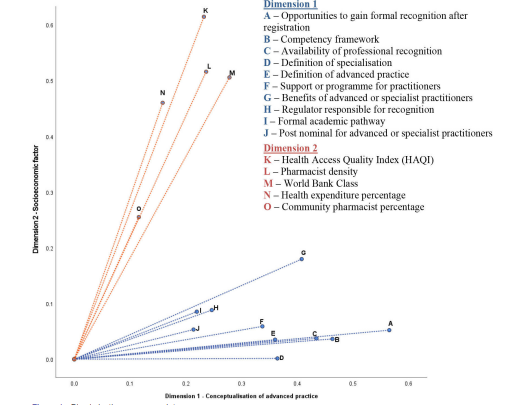
Eigenvalues for dimension 1 of the MCA result (4.637) indicate a greater weighting on this scale compared with dimension 2 (2.977).
his is also reflected in variance, with dimension 1 accounting for 30.9% while dimension 2 accounts for 19.8%; the overall model accounts for 50.8% of the total variance, indicating a reliable projection.
Figure 2 shows the joint category plot of the coded values of the model variables, showing correlations between variable values as well as their relationship to the model dimensions.
It revealed four groups of variable items that tended to cluster. A
long dimension 1 were the concepts and infrastructures for pharmacy workforce advancement, with clusters of presence/absence in sample countries divided by the abscissa (blue circled clusters in figure 2).
Where there are case values clustered together on the righthand side of dimension 1, this indicates the presence of nationally available policy and support available for structural advancement of practice, in contrast with left-hand clusters with no access to identifiable concepts and support in those case countries.
Coded values along dimension 2 were dichotomised into clusters of generally higher or lower attributes of socioeconomic and/or demographic measures (red circled clusters in figure 2).
Using the MCA model outputs, attributes of pharmacy workforce development potential can now be associatively connected with current country-level policy constructs within prevailing socioeconomic factors and access to, and implementation of, credible policy models for pharmacy workforce advancement.
Cluster analysis
Using the MCA model outcome and object scores, a hierarchical clustering analysis was conducted.24 The output suggests a three-cluster solution based on the coefficients of the agglomeration schedule and gradient inflexion of the resultant scree plot.
The three-cluster solution in the scree plot was also reflected in the clustering dendrogram; from this three-cluster solution, case membership for each proposed cluster was identified.
Figure 3 shows a scatter plot of object scores associated with each of the sample case countries identified by the MCA model.
Subsequently, overlay of the cluster analysis ‘cluster membership’ of the surveyed countries can be identified (country cases identified with the three-digit country ISO codes).25
Table 2 expand on the attributes associated with each of the identified clusters.
- Generally, countries in cluster 1 (blue) were mostly lower to upper middle-income countries;
- cluster 2 (green) were of a higher socioeconomic status and
- cluster 3 (purple) comprised mostly upper middle-income to high-income countries.
Cluster 3 countries tend to differ as these are more likely to have advanced practice scope policies in place compared with cluster 1, and these latter countries have a greater anglophone tendency.
Cluster 2 countries, although generally in higher socioeconomic categories, had mixed levels of practice advancement attributes.
These countries also tend to have much lower anglophone traditions.
Table 2 Cluster attributes
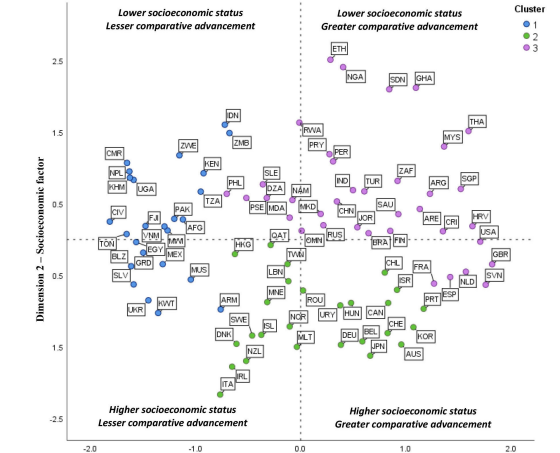
Figure 3 — Scatter plot of object scores (country ISO code used for labels).
See the original publication

Discussion
Advancing the global health workforce is one of the strategies to strengthen primary healthcare.
The 2018 Astana Declaration further emphasised the pivotal role of the health workforce, including the pharmaceutical workforce, in primary healthcare access and delivery to achieve universal health coverage by 2030.4 26
This paper presented evidence on the attributes of national workforce development infrastructures in place for advancing pharmaceutical workforce in the country.
From the findings, we identified factors that enhance and contribute to advanced practice policy development, namely the country’s socioeconomic factors and the availability of practice advancement concepts in the country.
In terms of MCA model dimension 1 — conceptualisation of advanced practice — we found that ‘opportunities to gain formal recognition after registration’, ‘competency development framework availability’, ‘professional recognition systems’, ‘definition of advanced practice or specialisation (scope of practice)’ and ‘support or programmes for practitioners to develop advanced practice and specialisation’, respectively have the highest associative value (figure 1).
This result shows that these concepts are essential in advancing pharmacy workforce in the country respondents.
From our findings, we proposed a global development roadmap for advanced and specialist practice to support country workforce self-assessment and self-diagnosed needs-assessments for progress towards achieving the FIP DG 4 — advanced and specialist development (online supplemental figure).
This roadmap can be used as an evidenced-based transnational tool for health workforce transformation policy programmes.
This study identified variation from a sample of 88 countries on workforce development attributes related to advancement in pharmacy scope of practice; lessons can be learnt from a systematic classification, and a transnational roadmap can be designed and adapted particularly for LMICs.
It has been suggested that a change in pharmacy education and a restructuring in legislation clarifying and protecting the roles of pharmacists may assist with narrowing the gap between the country clusters.27
It has been suggested that a change in pharmacy education and a restructuring in legislation clarifying and protecting the roles of pharmacists may assist with narrowing the gap between the country clusters
In addition to various regulatory bodies, country-level national pharmaceutical professional leadership associations are central in developing their respective workforces, supporting areas such as continuous professional development, legislation and guidelines and the implementation of tools to support pharmacists.10 15
It is important that these actions are made in conjunction with national frameworks for healthcare as well as the professional needs of individual pharmacists.
In this study, there has been some progress made from a smaller pilot sample of previous country responses9 10 with the early development of infrastructures for practice advancement, such as competency development frameworks, and by adopting and adapting ideas and resources of the frameworks from other countries.
This shows the benefit of looking for a global template to support and share ideas across nations.
An important finding from this study is that there is a key group of attributes that can describe workforce advancement in the country respondents and be used as a collective measure of progress (figure 2, blue circle).
The MCA and cluster analysis indicated this variable group was not fully associated with country-level socioeconomic status (eg, figure 2, red circle), indicating that the concepts of the scope of practice advancement do not need to be limited by socioeconomic status.
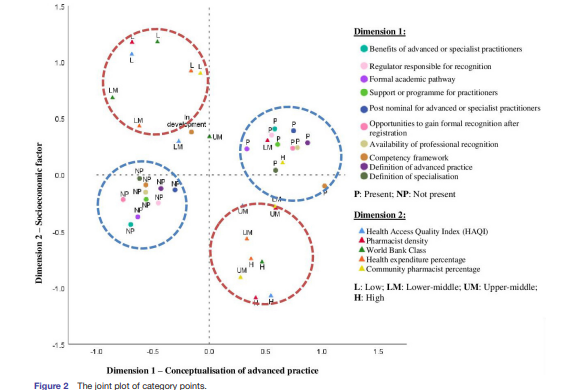
This suggests that we will be able to facilitate mechanisms for shifting workforce advancement attributes from ‘do not have an advancement concept’ to ‘having an advancement concept’ as a low-cost way of advancing the pharmacy workforce in a country and hence accelerate workforce development to meet the complex medicines-related challenges of primary healthcare across nations.
We envision accelerated workforce development progress as a ‘global advancement escalator’, with a resource focus on countries on the far left of figure 2 to shift towards the righthand scale of dimension 1.
For example, transnational templates for competency development frameworks and professional recognition systems can be designed using existing evidence-based mechanisms and shared using an ‘adopt and adapt’ needs-based approach for workforce development policy implementation.
The concept of a global Workforce Transformation Programme to support countries in leading the advancement of their national workforce becomes a closer reality.28
We envision accelerated workforce development progress as a ‘global advancement escalator’, with a resource focus on countries on the far left of figure 2 to shift towards the righthand scale of dimension 1
This study revealed three broad clusters of countries with similar characteristics for advanced workforce development.
Generally, cluster 1 countries mainly consisted of low-income to middle-income countries.
They consistently showed less traction with workforce advancement indicators included in the analysis.
Cluster 2 comprised upper middle-income countries with high rates of pharmacy advancement implementation.
Cluster 3 comprised high-income countries but did not necessarily have high traction with all of pharmacy advancement indicators.
Despite some countries in cluster 2 having a lower socioeconomic status than those in cluster 3, they had still adopted many concepts of advanced workforce practice.
This tends to indicate that the advancement of the pharmaceutical workforce is not an exclusive trait of higher-income countries.
As pharmacists play a crucial role in the provision of healthcare, particularly in primary care settings, this study may open up the possibilities of accelerated pharmacy advancement to countries regardless of income level.
Moreover, as pharmacists are increasingly working more closely with other healthcare professionals, improved expert team working with pharmacists at the advanced level would be beneficial as there would be an expectation that advanced pharmacists are competent in direct patient care and in developing new patient care services related to medicines management.29

Conclusion
This study identified key factors to support a transnational approach to pharmacy workforce advancement for strengthening PHC programmes in order to achieve UHC.
The three clusters identified showed that workforce advancement was not an exclusive trait of higher-income countries.
Lessons from nations that have previously implemented concepts of advancement in pharmacy practice may support other countries to accelerate the progress of advanced practice globally.
Lessons from nations that have previously implemented concepts of advancement in pharmacy practice may support other countries to accelerate the progress of advanced practice globally.
This study further opens up other research opportunities.
Variables in the survey only elicited responses that reflected how much support is available for pharmacy workforce advancement in each country.
As the research variables focused on nationally aggregated data and the presence or absence of key workforce indicators, levels of pharmacy advancement may not hold true for all areas within a country (eg, in federated countries) or have direct traction with the individual registered pharmacists themselves.
There is an opportunity to investigate the proportions of advanced and specialist practitioners available for the healthcare workforce in a country and the fields of advancement in which they are involved related to impact on patient care.
Further work in building this policy model for the advancement of practice development is also required to accelerate the progress of advanced practice globally to better meet national primary healthcare challenges.
Strengths and limitations
- This study is the most comprehensive to date analysing stages of pharmacy advancement across 88 countries.
- The survey nature is self-reported by participants, which may affect the validity of the findings; however, the triangulation process through respondent validation enhances the validity of the findings.
- The findings may be somewhat limited by the language and syntactical barriers for some countries in completing the survey and providing relevant data.
To the best of the authors’ knowledge, this study is the most comprehensive to date analysing stages of pharmacy advancement between countries. This study has also provided information on associations with country-level socioeconomic status and the stages of pharmacy workforce advancement. These findings may be somewhat limited by the language and syntactical barriers for some countries in completing the survey and providing relevant data. In addition, considering the survey nature is self-reported by participants, this may affect the validity of the results. However, the triangulation process through respondent validation enhances the validity of the results.
References and additional information
See the original publication
About the authors & affiliations
Ian Bates ,1,2 Sherly Meilianti ,1,2 Lina Bader,2 Rishi Gandhi,1 Rachael Leng,1 Kirsten Galbraith 2,3
1 Department of Practice and Policy, Faculty of Life Sciences,
UCL School of Pharmacy, London, UK
2 International Pharmaceutical Federation, The Hague, The Netherlands
3Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, Parkville, Melbourne, Australia
Acknowledgments
This work was supported and resourced by International Pharmaceutical Federation (FIP). We would like to acknowledge Dr Renly Lim and Whitley Yi for reviewing the article. We also would like to acknowledge Dr Catherine Duggan, FIP Chief Executive Officer, for reviewing the article.
Originally published at https://bmjopen.bmj.com