Forbes
Madhukar Pai
Oct 6, 2021
Image: Digital technologies & point-of-care tools have great promise to reduce the global diagnostic gap. Dr Peter MacPherson, Malawi-Liverpool-Wellcome Trust Clinical Research Programme
Key messages of the Lancet Paper (Edited by the author of the blog):
- 47% of the global population has little to no access to diagnostics.
- Diagnostics are central and fundamental to quality health care. This notion is underrecognised, leading to underfunding and inadequate resources at all levels.
- The level of primary health care is the diagnostic so-called last mile and particularly affects poor, rural, and marginalised communities globally; appropriate access is essential for equity and social justice.
- The COVID-19 pandemic has emphasised the crucial role of diagnostics in health care and that without access to diagnostics, delivery of universal health coverage, antimicrobial resistance mitigation, and pandemic preparedness cannot be achieved.
- Innovations within the past 15 years in many areas (eg, in financing, technology, and workforce) can reduce the diagnostic gap, improve access, and democratise diagnostics to empower patients.
- As an example of the potential impact, 1·1 million premature deaths in low-income and middle-income countries (LMICs) could be avoided annually by reducing the diagnostic gap for six priority conditions:
diabetes, hypertension, HIV, and tuberculosis in the overall population, and hepatitis B virus infection and syphilis for pregnant women. - The economic case for such investment is strong.
The median benefit–cost 1·1 million premature deaths in low-income and middle-income countries (LMICs) could be avoided annually by reducing the diagnostic gap for six priority conditions and exceeds one for four of the six priority conditions in low-income countries, with a range of 1·4:1 to 24:1.
Given the depth and breadth of the problems, sustained access to quality, affordable diagnostics will require multi-decade prioritisation, commitment, and investment. Incorporating diagnostics into universal health coverage packages will begin this process.
Every day, millions of Covid-19 tests are performed around the world. Because of the pandemic, everyone is aware of the importance of diagnostic testing.
But, as I pointed out earlier, diagnostic tests are necessary for a wide range of conditions that affect all of us, not just pandemic threats.
Good clinical care begins with the first step of diagnosis. But easy access to diagnostics is far from guaranteed.
In fact, a report published today, The Lancet Commission on Diagnostics, estimates that nearly half of the global population lack access to basic diagnostics for many common diseases.
The Commission brought together 25 experts from 16 countries. I was one of the commissioners. The Commission highlights (explainer video below) the centrality of diagnostics for any functioning health care system and calls on policy makers to close the diagnostic gap, improve access, and expand the development of diagnostics beyond high income countries.https://joaquimcardoso.blog/media/eac16099f1051b7a509e33adb882518e
“It is unacceptable that almost half of the global population has little to no access to diagnostics,” said Sue Horton, Deputy co-Chair of the Commission, and a professor at the University of Waterloo. “The consequences are worse health outcomes and a greater risk of catastrophic health expenditures,” she added.
“To ensure success in the provision of universal health coverage (UHC), the conquest of antimicrobial resistance, and the prevention of pandemics, policy makers and funders must recognize the centrality of diagnostics,” said Kenneth Fleming, Chair of the Commission, and a professor at the University of Oxford.
Diagnosis — the weakest link
The Commission used six tracer or priority conditions (diabetes, hypertension, HIV, tuberculosis, hepatitis B virus infection and syphilis) and showed that the diagnostic gap is the single largest gap in the continuum or cascade of care (figure below). In other words, across diseases and countries, most health systems are failing to detect conditions. Once a condition is detected, most health systems are able to offer some treatment.
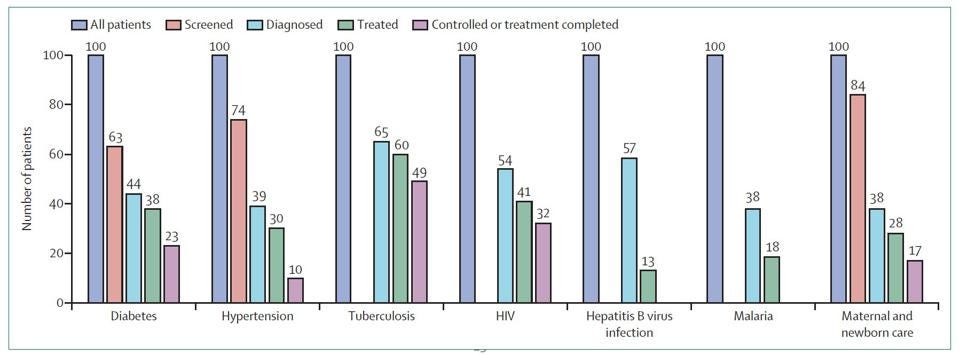
Cascade of care for different health conditions. Figure shows that the diagnostic gap is the largest … [+]. THE LANCET COMMISSION ON DIAGNOSTICS
The estimate that 35–62% of the population does not have access to essential diagnostics is an appalling finding,” said Pascale Ondoa, Director of Science and New initiatives at the African Society of Laboratory Medicine.
- The consistency of diagnosis as a key gap across communicable and non-communicable diseases is quite striking and begs the question: how can any country deliver UHC or fight pandemics, with so many people failing to get diagnosed?
- The diagnostic gap is greatest in primary care, where the report estimates that only about 19% of populations in low and lower-middle income countries have access to the simplest diagnostic tests (other than for HIV or malaria).
The Lancet report estimated that narrowing the diagnostic gap for just six conditions (listed earlier) from 35–62% to 10% would reduce the annual number of premature deaths in low-income and middle-income countries (LMICs) by 1.1 million.
As I wrote in a previous Forbes post, tremendous effort and innovation has gone into Covid-19 testing. We now have rapid tests as well as home-based, self-tests for Covid-19, and have come up with easier and simpler ways of taking testing closer to people’s homes and schools. Mobile testing sites, drive-through testing, and sample collection via community health workers, neighborhood pharmacies, schools and workplaces are all happening.
We need to do the same for many other areas in global health and ‘democratize’ access to testing.
The Covid-19 pandemic also shows the incredible value of digital health technologies (e.g. mobile apps, ultraportable digital x-rays, dashboards, chatbots), tele-health, and artificial intelligence (AI) based tools.
In addition, every country today has substantially higher capacity to conduct molecular testing.
All of these innovations and investments must be leveraged to address the global diagnostics gap.
The Lancet Commission report provides useful information on what diagnostics capabilities are required at each tier of the healthcare delivery system (image below).
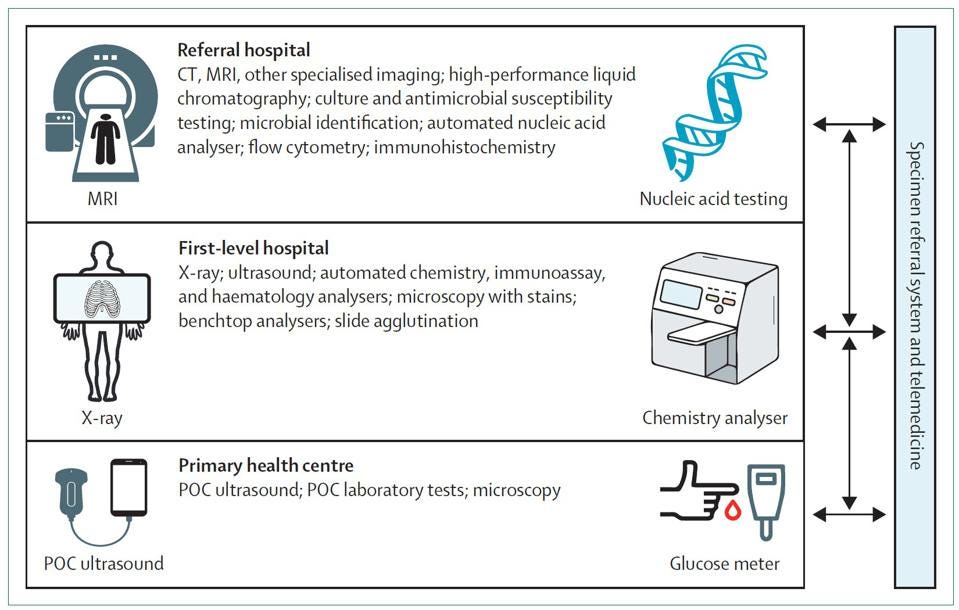
Diagnostics capabilities required at each tier of the healthcare system. The Lancet Commission on Diagnostics
No UHC without diagnosis
As part of the Sustainable Development Goals (SDG), all countries have pledged to ensure Universal Health Coverage (UHC) by 2030.
As the Lancet Diagnostics Commission argues, countries simply cannot achieve UHC if they are missing large numbers of people with treatable conditions.
“It is a fact that to achieve UHC and health security, diagnostics play a key role, especially at the primary health care level,” said Soumya Swaminathan, Chief Scientist, World Health Organization.
“As countries think about strengthening their health systems in the wake of the pandemic, it is key that they invest in diagnostics at least for the high burden diseases, develop national essential diagnostics lists, train the needed workforce, and set up regulatory mechanisms to evaluate and approve quality diagnostic tests, including those based on AI (artificial intelligence) algorithms,” she expanded.
She emphasized that WHO has an essential diagnostics list, prequalified priority diagnostics that meet quality and safety standards, and is also working to develop governance and regulatory frameworks for AI-based technologies.
India is among the countries that has successfully developed its own National Essential Diagnostics List (NEDL).
Kamini Walia at the Indian Council of Medical Research played a key role in this, as well as serving as a Lancet Diagnostics Commissioner.
“The Lancet Commission not only analyses in detail what’s ailing the diagnostics sector but also offers tangible solutions which countries could use to improve diagnostic availability in their countries,” Walia said.

TOPSHOT — A man reacts while a health worker wearing personal protective equipment (PPE) uses a … [+]. AFP VIA GETTY IMAGES
“In Africa, the Covid-19 pandemic has been a time of reckoning for the persistent, systemic, neglect that has undermined access to diagnostics,” said Marguerite Loembe, Senior Laboratory Advisor at Africa CDC.
“Innovative approaches have enabled African countries to setup Covid-19 testing capacity where there was none earlier,” she said.
“It will be key to ensure this momentum is seized such that lessons learnt and commitments made contribute to expanding access to diagnostics on the continent beyond Covid-19, to ultimately achieve UHC,” she elaborated.
The path forward
To build on the findings of this Commission, key recommendations listed in the report include
- the initiation of national and international advocacy programs,
- the creation of an international Diagnostics Alliance as an advocate, and
- the adoption of a World Health Assembly resolution on the need for diagnostics to be an integral part of any UHC program.
It is noteworthy that the recent Declaration of the G20 Health Ministers identified “accessible vaccines, therapeutics and diagnostics “ as one of the four priority areas for action.
“The devil is in the implementation,” said Patricia Garcia, a professor at the Universidad Cayetano Heredia in Peru, former Health Minister, and a Lancet Diagnostics Commissioner.
“To implement the Commission’s recommendations, there are responsibilities at national and global levels that need to be undertaken. Having partnerships and critical views of what can go wrong and how to make things right could help,” she elaborated.
Pascale Ondoa would like to see organizations in low and middle-income countries take the lead in implementing the Commission recommendations.
“LMICs must be at the core of the process through inclusive partnerships that recognizes local technical expertise, equity-minded decision-making, and increased utilization of locally-relevant epidemiological data for the prioritization of diagnostic technologies and strategies,” she said.
“Massive inequities in access to testing did not begin with Covid-19, nor will they end when the pandemic finally eases,” said Bill Rodriguez, CEO of FIND, Geneva, a non-profit global alliance for diagnostics.
“The Commission rightly calls for the pandemic to be a “turning point” for testing; we must address the lack of attention, lack of funding, lack of investment in laboratories and a trained workforce, lack of integrated data management systems, and lack of linkages between testing and healthcare services.
This report provides an essential blueprint for addressing these challenges and improving health for all. We cannot and must not let this moment pass if we are serious about reaching global targets and achieving UHC,” he added.
In Summary
In summary, we cannot fight pandemics or achieve UHC if we are flying with blindfolds.
- Diagnostics help remove our blindfolds, and give us visibility and clarity on what problems need to be addressed.
- Implementing the Lancet Diagnostics Commission recommendations must be a key priority for all policy makers, to not only recover from the pandemic, but also to achieve any health-related sustainable development goal.
About the author
I am a Canada Research Chair of Epidemiology & Global Health at McGill University, Montreal, where I serve as Associate Director of the McGill International Tuberculosis Centre. I did my medical training in India and public health training in Berkeley. My research is mainly focused on improving the diagnosis and treatment of tuberculosis in low and middle income countries. I like to write about global health, technologies of relevance to global health, healthcare delivery challenges in low income countries, and inequities in healthcare. I serve as an adviser to non-profits such as WHO, Stop TB Partnership, FIND, and TB Alliance. I have written for HuffPost, The Conversation, STAT, Devex, Scientific American, Nature blogs, among others.
Disclosures:
I have no financial interests in any diagnostic product or company. I have no industry ties, industry funding or consultancies.
I was a member of the WHO Strategic Advisory Group of Experts on In Vitro Diagnostics Group that developed the Essential Diagnostics List.
I serve on the scientific advisory committee of the Foundation for Innovative New Diagnostics (FIND), a non-profit based in Geneva, and hold grants on tuberculosis from the Bill & Melinda Gates Foundation.
I served as a Commissioner on the Lancet Diagnostics Commission.
Originally published at https://www.forbes.com.
Names Cited & Organizations:
Dr Peter MacPherson, Malawi-Liverpool-Wellcome Trust Clinical Research Programme;
Kenneth Fleming, Chair of the Commission, and a professor at the University of Oxford.
Sue Horton, Deputy co-Chair of the Commission, and a professor at the University of Waterloo;
Pascale Ondoa, Director of Science and New initiatives at the African Society of Laboratory Medicine;
Soumya Swaminathan, Chief Scientist, World Health Organization;
Kamini Walia, at the Indian Council of Medical Research;
Marguerite Loembe, Senior Laboratory Advisor at Africa CDC;
Patricia Garcia, a professor at the Universidad Cayetano Heredia in Peru, former Health Minister, and a Lancet Diagnostics Commissioner;
Bill Rodriguez, CEO of FIND, Geneva, a non-profit global alliance for diagnostics;
APPENDIX
PDF version of the original The Lancet paper

The Lancet Commission Members
Kenneth A Fleming, Susan Horton, Michael L Wilson, Rifat Atun, Kristen DeStigter, John Flanigan, Shahin Sayed, Pierrick Adam, Bertha Aguilar, Savvas Andronikou, Catharina Boehme, William Cherniak, Annie NY Cheung, Bernice Dahn, Lluis Donoso-Bach, Tania Douglas, Patricia Garcia, Sarwat Hussain, Hari S Iyer, Mikashmi Kohli, Alain B Labrique, Lai-Meng Looi, John G Meara, John Nkengasong, Madhukar Pai, Kara-Lee Pool, Kaushik Ramaiya, Lee Schroeder, Devanshi Shah, Richard Sullivan, Bien-Soo Tan, Kamini Walia