institute for continuous
health transformation
Joaquim Cardoso MSc
Senior Advisor for Continuous Health Transformation
and Digital Health
January 9, 2023
Key Takeaways
- Healthcare systems worldwide need transformation, which can be achieved through the adoption of value-based payment models.
- The transition to value-based payment models presents challenges, including the need to move away from volume-based payments, invest in new data and IT systems, and accept longer-term time horizons.
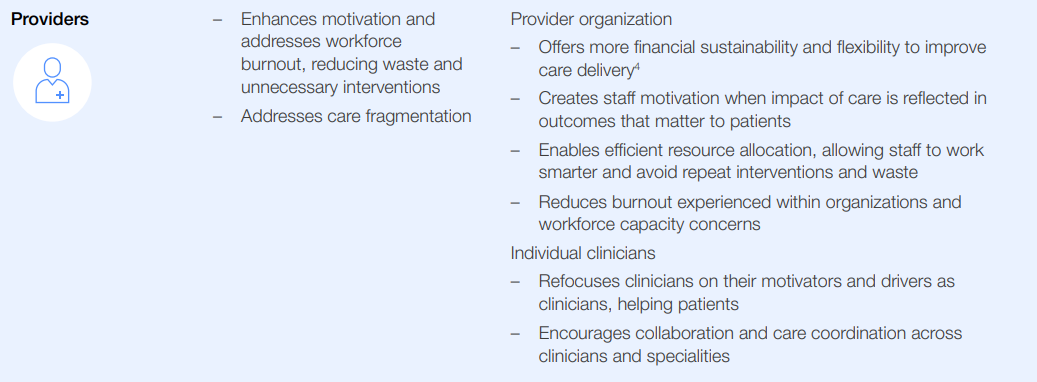
- Value-based payment models can emphasize quality of care over volume, reduce waste and unnecessary interventions, deliver integrated care, address health equity in outcomes, reduce workforce burnout, motivate high-value innovation, and create a more sustainable healthcare system.
- All levers of change, such as provider behavior and care delivery, must be addressed in order for value-based payment models to be successful.
- Barriers to the widespread adoption of value-based payment models include a lack of shared understanding, cultural and organizational resistance, and the complexity of designing and implementing such models.
- To overcome these barriers and successfully implement value-based payment models, healthcare stakeholders must commit to the pursuit of value-based healthcare, align on a common mission, design models that assess outcomes, incentivize behavior change, assess and improve the model, and scale up successful models.
Infographic
DEEP DIVE

The Moment of Truth for Healthcare Spending: How Payment Models can Transform Healthcare Systems
World Economic Forum
Yasmin Dias Guichot
Lead, Healthcare Systems Transformation
JANUARY 2023
Executive summary
Healthcare systems worldwide urgently need transformation, but this change is possible only alongside broadscale adoption of value-based payment models.
The change to value-based payment models is a vital transformation, albeit a difficult task.
There are many hurdles to overcome that require a willingness to leave behind volume-based payments, invest in new data and IT systems, develop new business models around care delivery models, and accept longer-term time horizons.
Greater efforts must be made globally to bring together shared understanding of the opportunities, challenges and solutions to make this urgent transformation possible and expedient.
Background
The World Economic Forum’s Global Coalition for Value in Healthcare launched the Global Enablers Payments Community, a multistakeholder network aimed at cultivating collaboration, exchanging experiences and accelerating healthcare transformation for this critical lever for value-based healthcare systems.
The community consisted of experts from sectors including healthcare providers, payers, pharmaceuticals, medtech, governments, consulting and academia, who met regularly to exchange case studies on value-based payment models to bring local and regional learnings to a global platform.
Additionally, non-community healthcare sector leaders were brought into the research to further understand the key issues.
This insight report is a thematic exploration by the coalition into payment models as an enabler of value-based healthcare.
The purpose is to take current perspectives using real experiences and case studies across healthcare stakeholders to provide guiding principles and concrete recommendations for implementing and deploying value-based healthcare payments across the globe.
Specifically, the report aims to:
- Raise the urgency and need to scale up the adoption of value-based payment models
- Guide healthcare leaders, including system leaders, payers, providers and policy-makers, towards a common understanding of value-based payment models
- Create greater awareness and inspiration by sharing success stories, drive increased willingness to participate in value-based payment models and motivate stakeholders to invest time, energy and resources
- Identify the critical barriers and potential solutions to progressing the focus from theory to value-based healthcare implementation.
Key findings include:
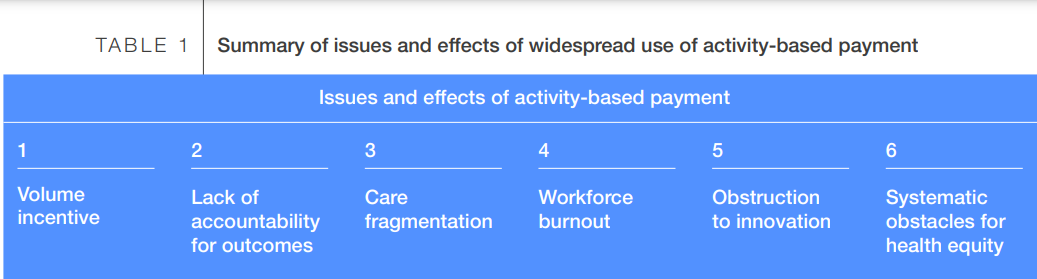
- Payment models based on fee-for-service (FFS) and diagnosis-related groups (DRG) contribute to the unsustainable development of today’s healthcare systems.
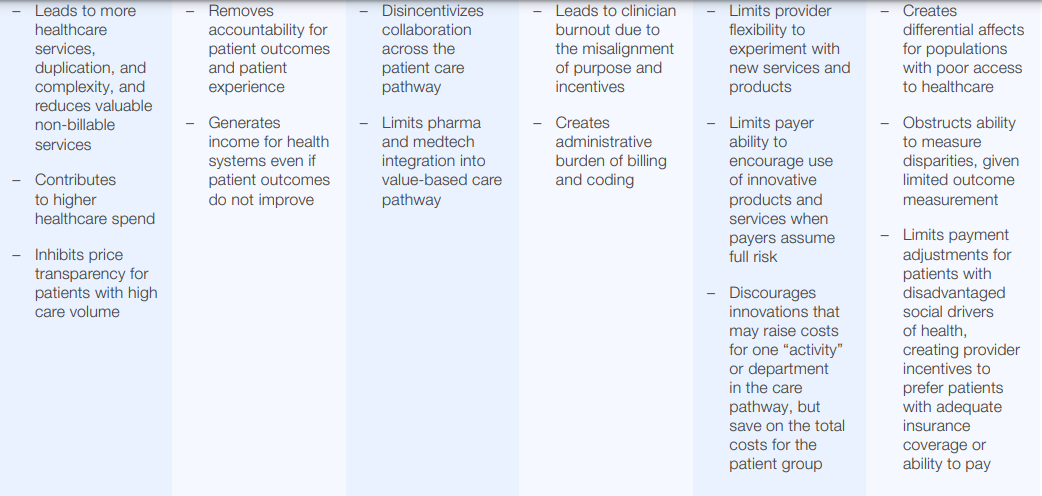
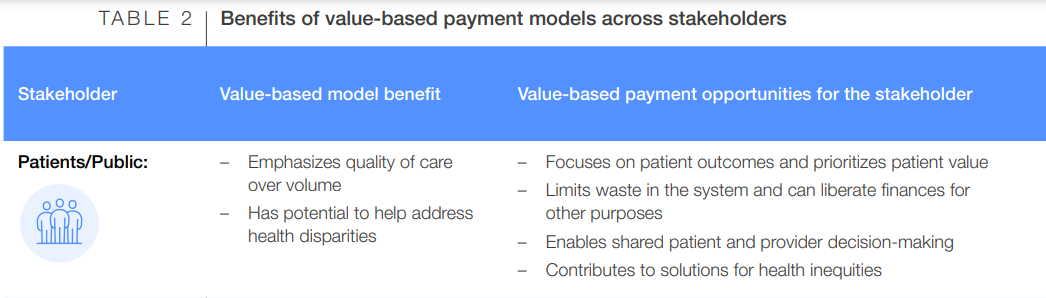
- Several key opportunities can be fulfilled through value-based payments models:
o Emphasize quality of care over volume
o Reduce waste and unnecessary interventions
o Deliver integrated care
o Address health equity in outcomes
o Reduce workforce burnout
o Motivate high-value innovation
o Create a more sustainable healthcare system
- Changes in payment models alone are not enough; all levers of change must be addressed.
For example, value-based payment models can drive faster change when they help enable a shift in provider behaviour and care delivery. - Though value-based payment models have not yet been widely scaled, healthcare stakeholders worldwide are eager to create a reality where the healthcare system focuses on the outcomes that matter to patients.
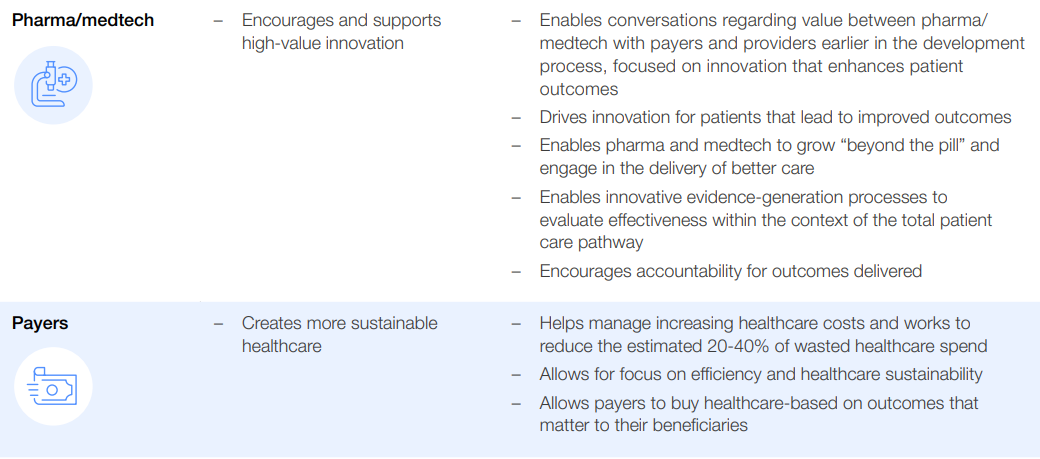
- The pathway for payment change requires stakeholders to decide at the leadership level to pursue value-based healthcare, align with partners on a common mission, design a payment model that will assess outcomes, implement the model to incentivize behaviour change, assess and improve the model and scale-up models across geographies and patient groups
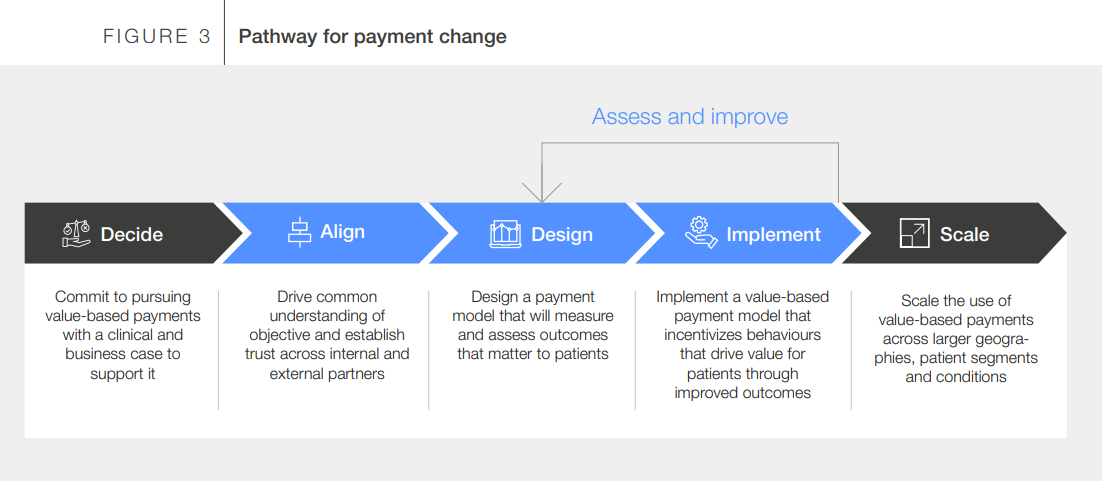
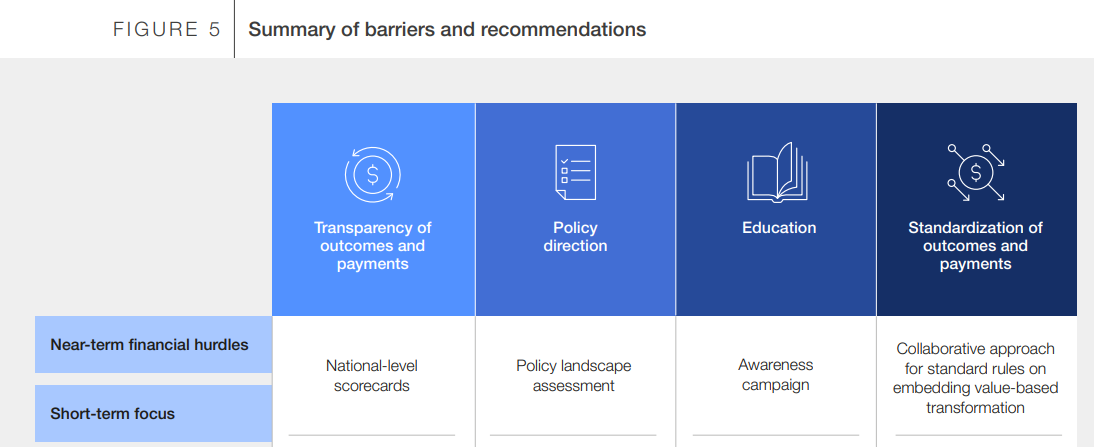
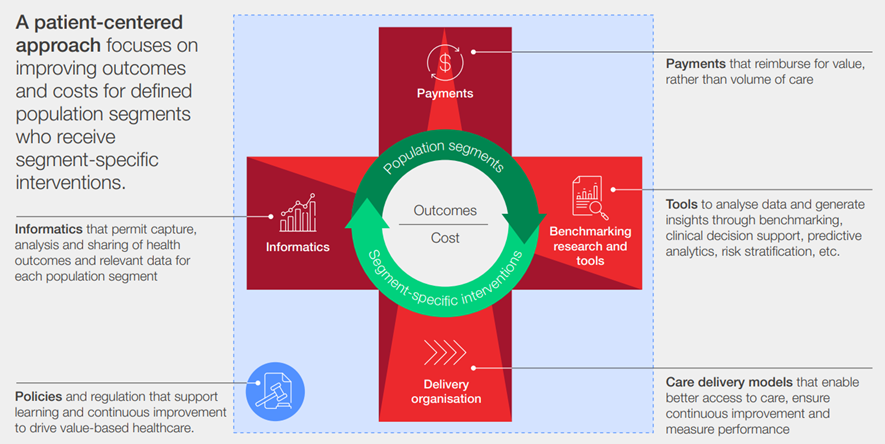
- The major barriers to systemwide adoption and scale-up of value-based payment models are the investment hurdles (near-term financial constraints, short-term focus and resistance to change) and the limited use of levers that tie stakeholders to the current system (policy, care delivery, tools and informatics levers). Solutions to barriers will include increasing transparency, policy direction, education and standardization.
- The importance of establishing consensus across stakeholders: value is about outcomes that matter most to patients.
The major barriers to systemwide adoption and scale-up of value-based payment models are: (1) the investment hurdles (near-term financial constraints, short-term focus and resistance to change) and (2) the limited use of levers that tie stakeholders to the current system (policy, care delivery, tools and informatics levers).
Solutions to barriers will include increasing transparency, policy direction, education and standardization.
Scale will require collaboration and partnerships — opportunities lie in systems that are willing to take a multistakeholder approach to ensure that all facets of the complicated healthcare system can come together simultaneously.
Together stakeholders can agree on a set of steps and move forward to implement value-creating systems.

Introduction: Value in healthcare — then and now
Healthcare delivery needs to transform and re-focus on healthcare that creates value.
The healthcare sector is facing three major crises — value, evidence and purpose. Across the world, pioneers have shown that value-based healthcare can address all three.
Stefan Larsson, Distinguished Fellow, World Economic Forum; Chairman and Co-Founder, International Consortium for Health Outcomes Measurement (ICHOM) in The Patient Priority
The global healthcare affordability crisis is not a new topic.
Individuals and healthcare systems are reaching the limits of what they can afford to spend on healthcare, and this spend is not correlated with improved patient outcomes.
While many mistakenly assume these issues emerge from a cost crisis in healthcare, they are driven by a global value crisis in healthcare, as stated by Stefan Larsson, Jennifer Clawson and Josh Kellar in The Patient Priority.[1]
There is an urgent need to change the way healthcare is delivered globally.
Healthcare delivery needs to transform and re-focus on healthcare that creates value, as guided by patient outcomes and accountability for resources in the healthcare systems.
Value-based payment models should no longer be considered a leap of faith.
The World Economic Forum is advancing this call to action using a value-based healthcare framework under the purview of the Global Coalition for Value in Health.
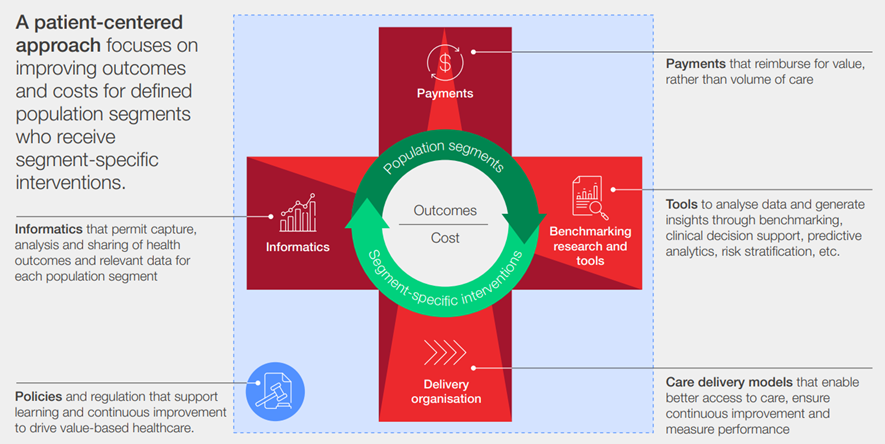
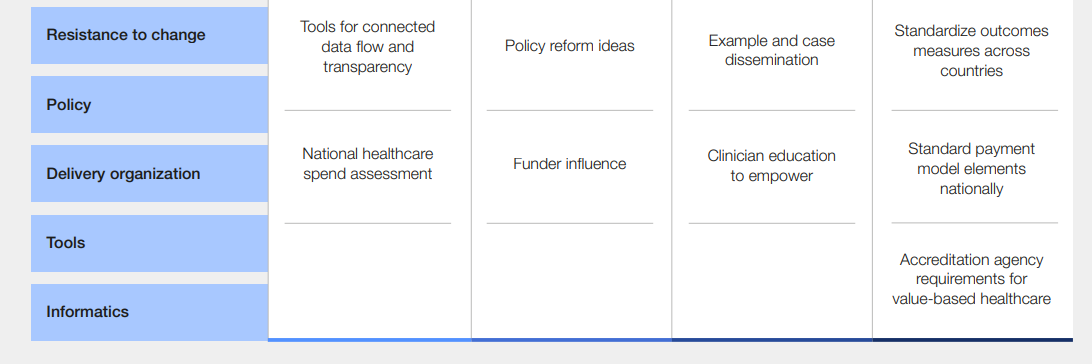
This patient-centred approach focuses on improving outcomes and costs for defined population segments that receive segment-specific interventions.
Healthcare transformation is complex, and its metamorphosis requires the orchestration of many levers of change.
The 2017 Value in Healthcare: Laying the Foundation for Health System Transformation report outlined key interdependent levers of change: payments, benchmarking, research and tools, delivery organization, informatics standards and policy.[2]
FIGURE 1 The value in healthcare framework for a value-based health system
Source: World Economic Forum, Accelerating the Pace of Health System Transformation, 2018
Value-based healthcare cannot exist without a focus on outcomes that matter to patients
Michael Porter and Elizabeth Teisberg introduced value-based healthcare in 2006, suggesting a radical transformation of the global healthcare systems, which resonated across stakeholders, given the urgent need for reform.
Understanding what value in healthcare means is critical.
The widely accepted definition of value in healthcare is the health outcomes that matter to patients relative to the resources or costs required to deliver those outcomes.
Value-based healthcare is an approach that aligns industry stakeholders (payers, providers, pharma/medtech, policy-makers) around a shared objective of improving patient health outcomes, providing the autonomy and accountability to providers to pursue the best way to deliver healthcare for the money spent.[3]
The defining aspect of value-based healthcare is that it seeks to address the issues experienced in healthcare today by reminding stakeholders that they all share a singular objective, providing value to the patient.

Aligning on “value for the patient”
The World Economic Forum’s value-based healthcare report series set a comprehensive framework describing the components of a value-based health system, sharing that “a patient-centred approach focuses on improving outcomes and costs for defined population segments who received segment-specific interventions”.
There cannot be a value-based healthcare system without being patient- or population-segment-centric in improving outcomes and costs.
True value-based healthcare goes beyond reducing costs, seeking to enable integrated patient care aligned with patient outcomes and quality.
Transformation will only be financially sustainable if care delivery and payment models are interlinked and if the payment system reinforces value creation.
Transformation will only be financially sustainable if care delivery and payment models are interlinked and if the payment system reinforces value creation.

Payment reform to drive value-based healthcare
To enable value-based healthcare across integrated, multidisciplinary teams, incentives and payment models must exist to support it.
Transformation will only be financially sustainable if care delivery and payment models are interlinked and if the payment system reinforces value creation.
Payment models have a powerful influence over healthcare impacting organizational and provider behaviour, health equity and innovation.
These three areas are sources of challenges and levers to drive change, and how healthcare systems structure their payments can impact all three.
- 1.Provider behaviour
- 2.Health equity
- 3.Innovation
1.Provider behaviour:
Legacy reimbursement systems have created volume-based business models.
These payment models influence their sense of accountability for patients and their outcomes, and how they feel about their purpose and value as caretakers.
Legacy reimbursement systems have created volume-based business models.
2.Health equity:
Updated payment mechanisms have the potential to improve health equity by incentivizing integrated care models and generating transparency for outcomes.
However, if payment models are constructed without an intentional goal of equity or if resources for transformation are not available to traditionally under-resourced provider organizations, any new payment model could end up widening disparities.
Updated payment mechanisms have the potential to improve health equity by incentivizing integrated care models and generating transparency for outcomes.
3.Innovation:
Healthcare payments received across stakeholders influence their motivations to innovate.
At the provider level, a payment model can incentivize or disincentivize the use of innovative treatments on a patient, especially when payers delineate which activities they will reimburse.
Payment models that incentivize higher patient value will drive industry, suppliers and providers to focus on innovation.
This report is designed to urge and galvanize a broader scale-up of value-based payment models.
It outlines key findings from case studies provided by experienced organizations and stakeholders, a shared lexicon adopted from Porter/Teisberg, and suggested action to align an environment that enables scale.
Outline of the publication [see the full version]
- 1 Moving to a high-value equitable healthcare system: the urgent case for value-based payments
- 2 How value-based payments are used today
- 3 Pathway for payment change
- 4 Barriers to adoption and scaling of value-based payments
- 5 Recommendations to drive payment change

Conclusion
It is the intention of this insight report to instill a sense of urgency across all stakeholders to change the way healthcare is delivered globally, to invest every healthcare dollar spent in what works best for the patient through the acceleration of the adoption of value-based payment models.
It is important to reemphasize the need for healthcare stakeholders to work together and find a common mission.
As the Forum truly believes, change can only occur when everyone comes to the table together, as the many examples provided show how rewarding, motivating and above all impactful such collaboration is.
Many things need to transform concurrently for payment models to change, including the other four enablers of value-based care: tools, care delivery models, informatics and policies.
While this report focused on ways to galvanize the adoption and scale-up of value-based payments to progress the overall value-based healthcare agenda, it is hoped that it encourages efforts across all four enablers in the value in healthcare framework to truly catalyse a health transformation.
The Forum’s Platform for Shaping the Future of Health and Healthcare has hosted the Global Coalition for Value in Healthcare since its launch in 2019 under the auspices of the Forum’s Annual Meeting.
For more information, visit the Global Coalition for Value in Healthcare website.
Endnotes
[1] Larsson, Stefan, Jennifer Clawson and Josh Kellar, The Patient Priority, McGraw Hill, 2022.
[2] World Economic Forum, Value in Healthcare: Accelerating the Pace of Health System Transformation, 2018.
[3] Ibid.
Names mentioned
Stefan Larsson, Distinguished Fellow, World Economic Forum; Chairman and Co-Founder, International Consortium for Health Outcomes Measurement (ICHOM) in The Patient Priority
Stefan Larsson, Jennifer Clawson and Josh Kellar in The Patient Priority.
Michael Porter and Elizabeth Teisberg












