the health strategist
institute for continuous health transformation
in health and tech
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
March 4, 2023
EXECUTIVE SUMMARY
The World Obesity Federation, in partnership with the World Health Organization, has released a report projecting that over half the world’s population will be either overweight or obese by 2035.
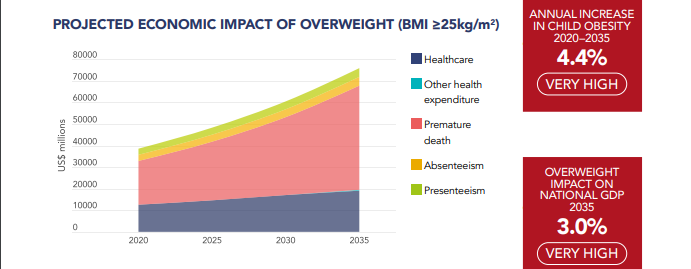
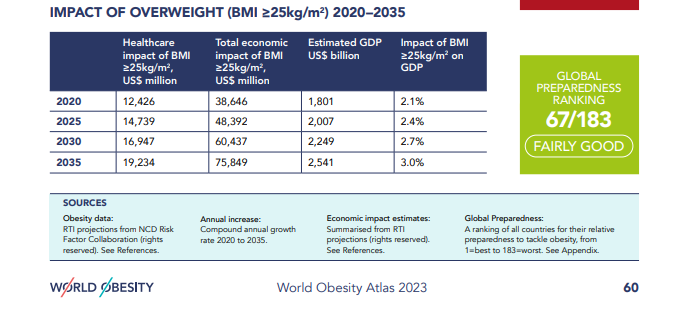
- The economic impact of a high body mass index (BMI) is estimated to reach $4.32tn annually, which equates to roughly 3% of global GDP.
- The projection represents an increase from $1.96tn, or 2.4% of global GDP, in 2020.
- The Atlas figures take into account the obesity-attributable healthcare costs of treating 28 obesity-related illnesses, including type 2 diabetes and several forms of cancer, in addition to lost economic productivity caused by both the inability to work and diminished performance on the job, as well as premature death.
- If current trends continue and policy inertia remains in place, the cost projections for the 161 countries included in the report may be underestimated.
- Some estimates of obesity’s economic impact in specific countries, including the U.S., have been larger than those in the Atlas.
INFOGRAPHIC

DEEP DIVE

Report: Obesity could cost the world over $4 trillion a year by 2035
StatNews
By Julia Belluz
March 2, 2023
The costs of obesity are projected to soar globally, in step with rising prevalence, according to a new report from the World Obesity Federation, the only global group focused solely on tracking obesity and a partner of the World Health Organization.
Over half the world’s population will be either overweight or have obesity by 2035, the report projected, while the economic impact of a high BMI could reach $4.32 trillion annually, if current trends continue and policy inertia around the disease remains in place.
That equates to roughly 3 percent of global GDP — about as much as the economy grows in a year or the same impact as the Covid-19 pandemic in 2020, the report authors said.
It’s also an increase from $1.96 trillion, or 2.4 percent of global GDP, in 2020.
“The costs are mind-boggling and a really good reason to make the case that any resources allocated to a comprehensive obesity strategy are investments and not costs,” said Johanna Ralston, CEO of the federation.
“In fact, there’s going to be enormous cost savings over time as well as improving people’s lives by avoiding complications and premature mortality associated with obesity itself.”

No country has seen a decline in obesity prevalence since 1975.
That includes childhood obesity rates, said Louise Baur, a University of Sydney professor and pediatrician, and the federation’s president.
“This means more adolescents now enter adulthood with established risk factors for chronic disease — they’re more likely to develop type 2 diabetes, or have heart disease risk factors or orthopedic problems, sleep apnea or fatty liver disease.”
A larger group of people living longer with obesity-related chronic illness is part of what’s driving the direct and indirect costs of obesity, which is what the report — called the World Obesity Atlas — estimated.
The Atlas’ figures take into account the obesity-attributable healthcare costs of treating 28 obesity-related illnesses, including type 2 diabetes and several forms of cancer, in addition to lost economic productivity caused by both the inability to work and diminished performance on the job, as well as premature death.

But the cost projections for the 161 countries included in the report, while enormous, may be underestimated, researchers who weren’t involved in the Atlas told STAT.
For example, “They ignore the entire issue of long-term disability in their economic calculations,” a major driver of obesity-related costs, said Barry Popkin, professor of nutrition at the UNC Gillings School of Global Public Health at the University of North Carolina.
Some estimates of obesity’s economic impact in specific countries, including the U.S., have been larger than those in the Atlas.
A recent Milken Institute study put the total annual cost of chronic diseases caused by obesity and excess weight at $1.72 trillion in the U.S. alone in 2016 — just shy of the Atlas’ worldwide cost estimate for 2020 — and equivalent to 9.3 percent of nationwide GDP.
Another global obesity report, from the OECD, included a more modest estimate for the U.S. — 4.4 percent of GDP lost — closer but still higher than the Atlas’ U.S. estimate of 3.5 percent for 2020.
Since the Atlas brings global data together, the researchers were limited to metrics that are available across all 161 countries, explained health policy analyst Adeyemi Okunogbe, a report author based at the global health think tank RTI International.
Many low-resource countries don’t have data on obesity-related disability, unemployment, or early retirement, for example, which may have driven down the projected economic burden.

Another potential limitation is that the Atlas groups together the impact of overweight and obesity based on BMI, since that’s how global data the researchers drew on were compiled.
Excess weight isn’t always correlated with poor health, said William Dietz, director of the Sumner M. Redstone Global Center for Prevention and Wellness at George Washington University, and it may have been more accurate to look at obesity alone.
Popkin argued that the approach, however, may be appropriate. “For much of the world, the biological insult in terms of increased risk or likelihood of diabetes and hypertension starts before a BMI of 25, while for Caucasians it starts later around 29–30,” he said.
The threshold for clinical obesity starts at a BMI of 30. While an imperfect diagnostic tool, BMI is useful for estimating overweight and obesity in populations, he added.
The report authors also didn’t dive into the potential costs and cost savings of the new class of GLP1-based diabetes and obesity drugs, such as Ozempic and Wegovy.
While considered highly effective, the drugs can carry a price tag of upwards of $1,000 per month for patients using them for weight loss, since many insurance companies don’t yet cover them for that purpose.
The drugs may also reduce the long-term risks and costs of obesity and its associated diseases, such as type 2 diabetes.
“Health plans are very reluctant to approve the use of these medications because they think they’re opening a Pandora’s box,” Dietz said, something he attributes to the bias that obesity is a “self-induced illness.”

Relatedly, the report doesn’t capture the economic toll of weight stigma, and its very real impact on the livelihood of people living with obesity, a penalty that’s especially harsh for women.
According to an Economist analysis, research from the U.S., Canada, Britain, and Denmark showed overweight women tend to have lower salaries, while women with obesity take a 10 percent income hit.
“That is a tremendous cost that is probably not reflected in any of the direct medical costs,” said Dietz.
“And it may contribute to medical costs, because among the most biased and stigmatizing people in the life of a person with obesity are physicians.”

Whatever the precise economic toll of obesity turns out to be, one thing is for sure: the burden is growing and it won’t be evenly spread around the world.
The biggest cost increases are projected for low- and middle-income countries, where obesity rates are growing fastest.
The total economic impact of obesity is projected to increase fourfold by 2060 in high-income countries, and 12 to 25 times in lower resource settings.
This urgency isn’t currently reflected in obesity policy, said Ralston.
“A global treaty would be fantastic but there’s not been a concerted political will behind that.”
Perhaps as the impact of the disease on health and wealth becomes more visible, that urgency will arrive, she added.
“I’d like to think we will be prepared for it as momentum grows. Policies don’t often change until there’s an existential threat.”
Originally published at https://www.statnews.com on March 2, 2023.
Names mentioned (selected list)
- Johanna Ralston, CEO of the federation.
- Louise Baur, a University of Sydney professor and pediatrician, and the federation’s president
- Barry Popkin, professor of nutrition at the UNC Gillings School of Global Public Health at the University of North Carolina.
- Adeyemi Okunogbe, a report author based at the global health think tank RTI International.
- William Dietz, director of the Sumner M. Redstone Global Center for Prevention and Wellness at George Washington University,