public health unit
@ health transformation institute
Joaquim Cardoso MSc
Chief Researcher, Editor and
Senior Advisor
January 15, 2023
SUMMARY
Background
- Unmet need is a metric used to assess the performance of health care systems throughout the world.
- One of the primary objectives of the Brazilian health care system is to identify ways to improve the health outcomes of all citizens.
- To accomplish this challenging goal, the health care system in Brazil will need to identify and eliminate barriers and provide timely and adequate access to health care services to all.
Methods
- This study assessed the performance of the Brazilian health care system by focusing on the unmet need for health care services and medications.
- We evaluated the Brazilian National Health Survey data collected in 2013 and 2019 to determine the magnitude of socioeconomic-related inequalities associated with unmet health care needs.
- Primary contributing factors were identified via decomposition analysis of the calculated concentration indices (CInds).
Findings
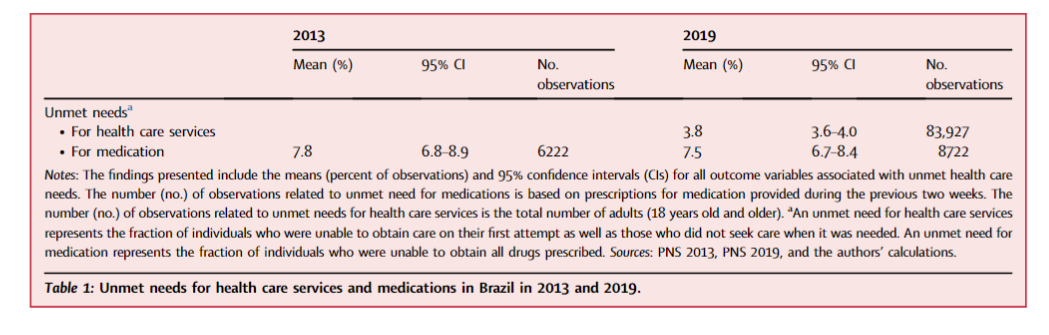
- Despite the availability of universal health care, 3.8% and 7.5% of the population in Brazil reported unmet needs for health care services and medications, respectively in the 2019 survey.
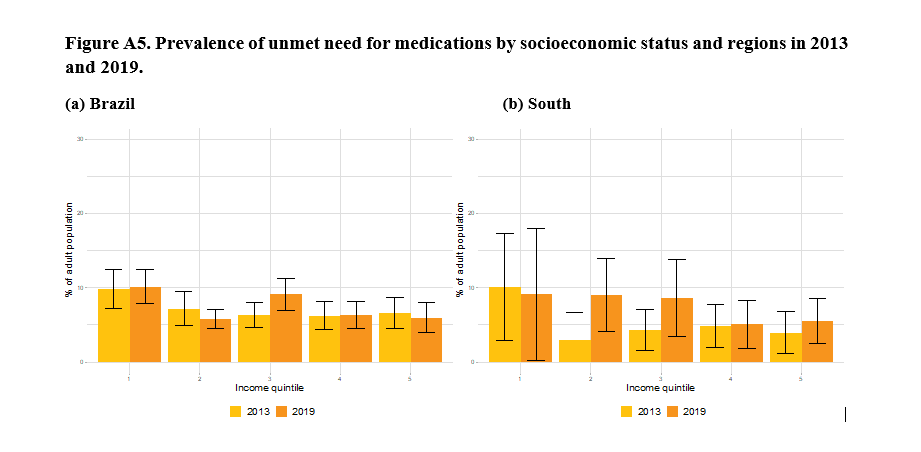
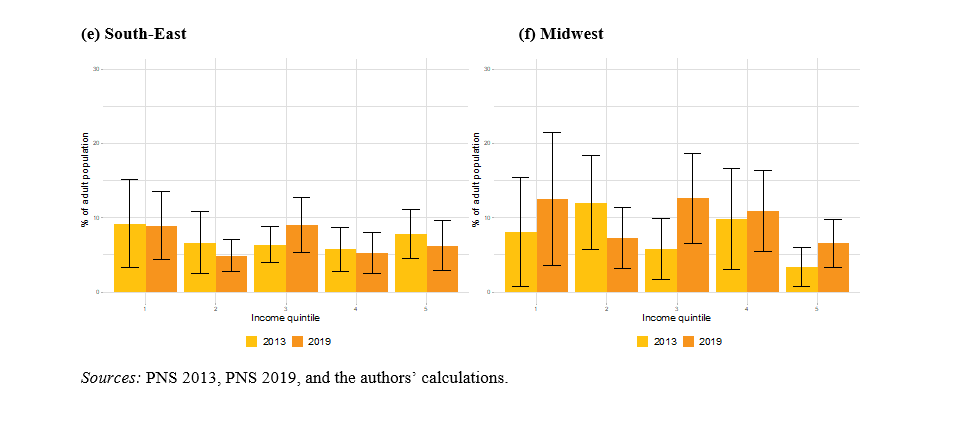
- Although the overall unmet need for medications remained unchanged between 2013 and 2019, CInd analysis revealed significant pro-poor inequalities with respect to unmet needs for both health care services and medications.
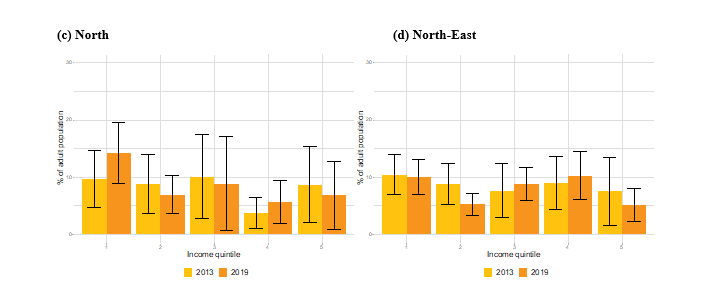
- The overall magnitude of these inequalities was higher in the poorer regions of the country.
- The use of private health insurance as well as individual health and socioeconomic status contributed significantly to the inequalities associated with unmet needs for health care services and medication throughout Brazil.
Although the overall unmet need for medications remained unchanged between 2013 and 2019, CInd analysis revealed significant pro-poor inequalities with respect to unmet needs for both health care services and medications.
Interpretations
- Policy interventions should focus on improving access to health care services, extending coverage to include pharmaceuticals, and targeting both financial and non-financial barriers to obtaining care, particularly those experienced by the poor and vulnerable populations in Brazil.
Policy interventions should focus on improving access to health care services, extending coverage to include pharmaceuticals, and targeting both financial and non-financial barriers to obtaining care, particularly those experienced by the poor and vulnerable populations in Brazil.
INFOGRAPHIC
DEEP DIVE (excerpt version of the paper)

Inequalities in unmet need for health care services and medications in Brazil: a decomposition analysis
The Lancet
Maíra Coube, Zlatko Nikoloski, Matías Mrejen, lias Mossialo
13 January 2023
RESEARCH IN CONTEXT
Evidence before this study
We employed the search terms “Brazil” and “unmet need” and “health care” and “medications” to identify relevant English and Portuguese language publications in PubMed and Google Scholar.
We identified only one descriptive study that systematically assessed unmet needs and their correlates in Brazil between the years 1998 and 2008.
Other studies were based solely on data that were not nationally representative and/or that highlighted unmet needs for specific health services or specific source of medication access.
Added value of this study
We evaluated results from two Brazilian National Health Surveys (Pesquisa Nacional de Saúde [PNS]) that spanned the years 2013–2019 with a focus on unmet needs for health care services and medications.
We examined the impact of private health insurance and socioeconomic inequalities on the extent of the inequalities observed that focused on unmet needs for both health care services and medication.
We also explored the evolution of unmet needs for medication between the years 2013 and 2019 at both national and regional levels.
Implications of all the available evidence
Although Brazil currently offers universal health care coverage, in the 2019 survey, 3.8% and 7.5% of the population reported unmet needs for both health care services and medication, respectively.
Moreover, the percentage of the population experiencing unmet needs specifically for medication remained unchanged between 2013 and 2019.
Individuals reporting unmet needs are heavily concentrated in the poorest segments of the population and the most economically-deprived regions of Brazil.
The use of private health care insurance and socioeconomic disparities exacerbate these inequalities.
Policy interventions might focus on improving coverage and access to critical pharmaceuticals while targeting financial and non-financial barriers to obtaining health care services, particularly for the poor and most vulnerable Brazilians.

Introduction
Timely and effective access to health care and affordable essential medications present ongoing challenges to the goal of achieving universal health coverage in many low- and middle-income countries.1
Both financial and non-financial barriers to access can impede the appropriate use of health care services and may lead to poorer overall health.2
Moreover, substantial inequalities regarding access to health care services and medication clearly exist even in countries that provide universal health care coverage.
In these cases, the unmet need for health care services is typically most pronounced in the most economically disadvantaged populations.
Thus, a careful analysis of unmet needs is an essential first step toward the design of policies focused on reducing health care inequalities.2, 3, 4, 5
Brazil presents a unique setting in which to analyse inequalities in access to health care services.
Brazil is currently one of the most economically-unbalanced countries in the world (Gini index of 48.9 in 2020).6
Furthermore, while Brazil supports a single-payer, publicly funded national health service known as the Unified Health System or Sistema Único de Saúde (SUS), over half of the total expenditure on health care comes from private sources.7
The SUS is a taxpayer-funded public health care system that provides services at all levels free of charge at the point of delivery.
The system has achieved significant gains over the past 30 years; improvements in both coverage and access to health care services have resulted in better health outcomes overall.8
Primary health care programming that covers over 60% of the population represents a central component of the national health service; it has improved the health of the Brazilian population9, 10, 11 and reduced health inequalities.12
Primary health care programming that covers over 60% of the population represents a central component of the national health service; it has improved the health of the Brazilian population9, 10, 11 and reduced health inequalities
However, while everyone is covered by the SUS, 28.5% of the population (primarily individuals with higher incomes who are formally employed and residing in urban centers) remains covered by one or more private health insurance schemes.13
However, while everyone is covered by the SUS, 28.5% of the population (primarily individuals with higher incomes who are formally employed and residing in urban centers) remains covered by one or more private health insurance schemes
Additionally, and despite significant advances, access to specialized care remains a major shortfall in the public health care sector and long waiting times persist.8
Additionally, and despite significant advances, access to specialized care remains a major shortfall in the public health care sector and long waiting times persist
Access to medication in Brazil has undergone significant changes in the past several years.
In theory, public health facilities in Brazil can provide access to pharmaceuticals listed in the National List of Essential Drugs at no charge to the patient.
However, in reality, access to medication is frequently constrained by rationing resulting from limited and intermittent stocks.
Most private health insurance programs available in Brazil do not cover the costs of prescription drugs; individuals carrying private insurance need to cover the cost of medication out-of-pocket.
In 2006, Brazil initiated a government-funded program that subsidizes the purchase of some medications (e.g., anti-diabetic and anti-hypertensive drugs) from retail pharmacies.
Recent reports suggest that this program has been largely successful in reducing avoidable hospitalizations due to diabetes.14
However, catastrophic health care expenditures, specifically related to the purchase of necessary medication, remain a major cause of financial hardship. This mainly affects low-income households15 with pronounced regional disparities.16
However, catastrophic health care expenditures, specifically related to the purchase of necessary medication, remain a major cause of financial hardship. This mainly affects low-income households15 with pronounced regional disparities.16
The highly-fragmented nature of Brazil’s health care system and persistent regional disparities remain major barriers to more equitable access to health care services.17
Brazil has large geographical variations with respect to the distribution of infrastructure, human resources, access to medication, and coverage by its national health care programs.16,18, 19, 20
These geographical variations in the supply of health care resources coupled with the aforementioned two-tiered (public versus private) financing system lead to disparities in both access to and quality of health care as well as protection from financial risk.17,21
Results from previous studies suggest that the limited availability of health care providers, infrastructure, and pharmaceuticals in underserved areas remains among the major challenges.
Likewise, the financial burden associated with seeking care (e.g., transportation costs) represents an additional barrier to access.22,23
Results from previous studies suggest that the limited availability of health care providers, infrastructure, and pharmaceuticals in underserved areas remains among the major challenges.
Likewise, the financial burden associated with seeking care (e.g., transportation costs) represents an additional barrier to access.
Existing evidence suggests that the inequalities in unmet health care needs largely reflect the overall socioeconomic inequalities in Brazil.
In the only published study that systematically assessed unmet needs for health care in Brazil, Osorio et al.24 reported a decrease in the percentage of the population facing unmet needs from 3.5% in 1998 to 2.9% in 2008, mostly due to issues related to costs and affordability.
By contrast, another more recent study focused on access to medicines through the public health system reported an increase in the proportion of people who did not obtain any medication from the public system between 2013 and 2019.25
Other studies focused on unmet needs for specific health services (e.g., mental health, access to pharmaceuticals) and/or presented findings that were not limited to health care in Brazil23,26,27 (see Appendix Table A1 for further details).
Thus, the goal of this study was to evaluate the unmet need for medications (years 2013 through 2019) and health care services (in 2019 only).
As part of this study, we planned to determine the link between unmet needs and their relevant determinants, notably, the impact of co-existing private health insurance as well as the socioeconomic and geographical disparities within the population of Brazil.
Methods and Other Sections
See the original publication (this is an excerpt version)

Discussion
The main objective of this study was to analyse inequalities associated with unmet needs and factors contributing to access to health care services and medications in Brazil.
The data used in this study were from a nationally representative survey conducted in 2013 and 2019.
The results of our analysis revealed that inequalities in unmet needs for both health care services and medications with primary impact on the poor.
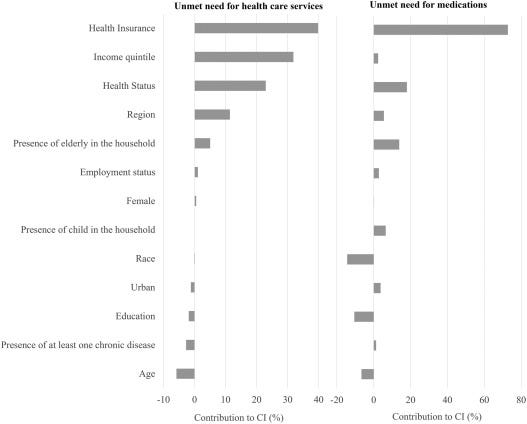
Moreover, the results from the decomposition analysis revealed that enabling factors (e. g., socioeconomic status and the use of private health insurance) and need factors (e.g., poor health) are the most significant contributors to these inequalities.
This result was confirmed by our analysis of the underlying factors contributing to these unmet needs.
This analysis revealed that the poorest individuals in the population were those who most frequently cited affordability as the reason that health care services and medication needs remained unmet.
Finally, our results are consistent when re-evaluated at the sub-national level.
Specifically, we found that the magnitude of unmet need for health care services and medications is particularly large in the Northern region of the country in which socioeconomic factors were identified as the largest contributors to the inequality with respect to the unmet need for medications.
While our results are largely comparable, our results on the prevalence of unmet needs are slightly higher than those described in a previous publication.24
This may be driven in part by the use of a different instrument (the National Household Sample Survey) in these previous analyses. Nonetheless, our results are consistent with the findings reported in other Latin American countries.
A large study that included results from 27 countries throughout the Americas measured unmet needs and concluded that those in the poorest groups are more likely to experience barriers to access to health care services due to financial reasons, availability of resources, geographic access, and acceptability.32
Previous assessments of unmet needs for health care services, particularly among the poor, have revealed that the Brazilian universal health system remains challenged due to ongoing barriers to access, unequal supply of health services, and even lack of information regarding the availability of health care services.33
Collectively, these results suggest that there remain significant challenges to providing equitable access to health care in both low- and middle-income countries and that these problems might persist even after the establishment of a large publicly funded national health system that provides universal health care coverage to all.
Our results focused on the unmet needs for medications complement those reported by the National Survey on Access, Use and Promotion of Rational Use of Medicines in Brazil (PNAUM), …
… which was a national household survey carried out between 2013 and 2014 that explored access to and use of essential medicines prescribed to adults to treat chronic non-communicable diseases (NCDs).34
Among the findings from this earlier study, ∼5.7% of all Brazilians who were aware of their medical diagnoses and who had received a prescription for appropriate treatment reported that they were unable to obtain all medications prescribed by the physician during the previous 30 days.35
These outcomes were reported most frequently in the Northeast and among those who were most severely affected by their disease.
Studies that focused on access to medications for specific NCDs found heterogeneity in unmet needs based on individual diagnoses, with values ranging from 2.1% for hypertension,36 and 2.2% for diabetes37 to 8.5% for chronic respiratory disease.38
Collectively, these results suggest that the prevalence of unmet needs for medications among those with NCDs is lower than the prevalence of overall unmet needs reported by the entire population of Brazil.
This might reflect the successful implementation of national policies designed to supply medicines for NCDs at no cost.14
However, our findings also highlight persistent regional inequalities and high prevalence of unmet needs for some specific conditions.
As noted above, the results of our analysis at the regional level are consistent with those emerging at the national level, and both point to significant inequalities in unmet needs for both, health care services and medications specifically in the North when compared to the rest of the country.
This is likely to be a result of both economic and health care-related factors.
As noted above, the results of our analysis at the regional level are consistent with those emerging at the national level, …
… and both point to significant inequalities in unmet needs for both, health care services and medications specifically in the North when compared to the rest of the country.
The North is the largest region in Brazil yet is among the lowest among all regions in the country with respect to socioeconomic development.
In terms of the Gross Regional Product (GRP) per capita, the North is in fourth place among the five designated regions; the GRP of the North trails those of the Midwest, South, and Southeast.39
Moreover, the heavy concentration of unmet need for health care services in the North region may be also due to the difficulties involving the number of health professionals who choose to practice in this region, geographical accessibility to an SUS pharmacy, the poor infrastructure of the primary health care units, and difficulties with transportation of both health care teams and patients.22,27,40
Moreover, the heavy concentration of unmet need for health care services in the North region may be also due to the difficulties involving the number of health professionals who choose to practice in this region, geographical accessibility to an SUS pharmacy, the poor infrastructure of the primary health care units, and difficulties with transportation of both health care teams and patients.
The results of our analysis also revealed that the unmet need for medications remained unchanged between 2013 and 2019 and that this finding was driven by an interplay between the socioeconomic and geographical disparities described above.
In other words, while the unmet need for medications diminished somewhat among those who were comparatively wealthy, it increased among those who remain poor; these results ultimately offset one another.
This increase in unmet needs for medications among the poor was exacerbated by the existing geographical inequalities, which are particularly pronounced in the North.
The extent of this increase outweighed some of the improvements reported in other regions (e.g., the Midwest).
As discussed in the paragraphs above, the North is the poorest region in Brazil and experiences significantly worse health outcomes largely due to problems related to access to health care services.41
As discussed in the paragraphs above, the North is the poorest region in Brazil and experiences significantly worse health outcomes largely due to problems related to access to health care services.
We also found that unmet needs for health care services and medications were further exacerbated by access to private health insurance.
As private health insurance is available only to those with the ability to pay and is largely related to employment status, its use tends to be unequally distributed and heavily concentrated among the wealthier members of a given population.
Hence, the advantage that it provides to those who can afford it may exacerbate inequalities in access to health care services compared to those who must rely solely on publicly-available services.
This situation leads to an implicit two-tier system in which the wealthy have “double coverage” by both SUS and private health insurance, whereas the poorer individuals rely solely on SUS.
The case of Brazil reveals the difficulties when attempting to offer adequate care and timely services to all at no cost at the point of care.
For example, data from PNS for 2019 suggest that up to a fifth of the individuals with private health insurance still rely on health care services provided through the public health system.
For example, data from PNS for 2019 suggest that up to a fifth of the individuals with private health insurance still rely on health care services provided through the public health system.
Results focused on inequalities in unmet needs for health care and medications during this period are particularly relevant because our survey was performed during a time of major economic recession and increased poverty rates nationwide.
In 2019, the Gross Domestic Product (GDP) per capita was 6.8% lower (in adjusted currency values) than in 2013.
At the same time, the unemployment rate grew from 7% in 2013 to 11.9% in 2019. During this period, the poverty headcount ratio at $3.2 (2011 PPP (Purchasing Power Parity)) per day grew from 8% to 10%.6
Our results suggest that inequalities in unmet need for medications also grew during this interval.
Collectively, these results suggest that barriers to accessing needed medications in Brazil grew among those with lower income during this economic downturn.
Nevertheless, efforts to ascertain the direct impact of the economic recession on unmet needs will require additional analysis using alternative data and methodological approaches that exceed the scope of the current work.
Additionally, institutional reforms and public spending restrictions implemented in Brazil during this period may have increased the division between public and private health financing and thus led to increased inequities.7
World Bank reported that public health expenditures in Brazil decreased from 44.52% of total health expenditure in 2013 to 40.74% in 2019.6
Considering that the use of private insurance was identified as the largest contributor to inequalities in unmet need for health care services and medication, this represents a concerning trend that might exacerbate future health-related inequalities.
This study has some specific limitations.
First, Andersen’s behavioural model of health services utilisation31 which was employed to categorise the covariates used in this analysis exhibits only limited capacity to generalize results.42
However, despite this limitation, and acknowledging that various factors may contribute to the search for health care, this model provides a framework that permits us to consider many of these factors and their interrelationships.
The Andersen model also offers additional guidance in interpreting results by identifying the factors that contribute to income-related inequalities in health care.
Second, given its nature, the CInd and decomposition analysis facilitates the acquisition of correlational as opposed to causal inference.
Third, socioeconomic inequalities measured by the CInd (e.g., income distribution) represent only a partial approach to this complex issue, as there are other potentially relevant factors, including race and sex, that are not considered.
However, the decomposition analysis assessed the contributions of other factors, including age, race, sex, area of residence, and the presence of one or more non-communicable diseases to the observed socioeconomic inequalities.
Given the availability of question on unmet need in the analysed surveys, only the datasets for 2013 and 2019 were used in this analysis.
Finally, a comparison of our results with those presented in international studies focused on unmet needs and that used survey data based on individuals’ own assessments2 reveals some important conceptual differences.
For example, our final derived variable of unmet need for health care services and medications considers only events of the previous two weeks rather than the previous 12 months and entails an implicit concept of health need as opposed to a more explicit question focused on the receipt of treatment or medications as needed.
However, despite these limitations, this paper presents an all-encompassing analysis of the inequalities in the unmet need for health care services and medications in Brazil in 2019 and the evolution of the unmet need for medications from 2013 to 2019.
Our study also identifies the factors that provide the strongest contributions and documents the relevance of private health insurance as the main driver of these inequalities in the unmet need for health care services and medications, even within the context of universal health coverage.

Conclusion
Our findings reveal that there remain inequalities in unmet needs for health care services and medications in Brazil.
Collectively, our results support the view that efforts to achieve equality in the delivery of health care services and access to medications should be ongoing and remain important policy concerns.
Our findings also have implications for policy development in other middle-income countries that provide universal health care coverage.
First, our findings are consistent with the results reported by several Organization for Economic Co-operation and Development (OECD)-aligned countries and the Americas that have achieved universal or near-universal health care coverage for their populations.
Specifically, OECD findings reveal that inequalities in access to health care services persist over time despite increases in health care expenditures and investments directed at expanding infrastructure.2,3,32,43, 44, 45
Second, our findings revealed that more Brazilians reported unmet needs for medications compared to health care services, notably those who are among the poor and disadvantaged populations.
Therefore, policy interventions should focus on extending coverage for pharmaceutical needs and might target both financial and non-financial barriers to obtaining health care services, particularly among the poor and vulnerable individuals residing in the lower-resourced regions of the country.46
…more Brazilians reported unmet needs for medications compared to health care services, notably those who are among the poor and disadvantaged populations.
Future research will be needed to meet the challenge of monitoring the evolution of unmet needs for health care services and medications as well as identifying their determinants.
References
See the original publication https://www.sciencedirect.com
About the authors & affiliations
Maíra Coube b c,
Zlatko Nikoloski a ,
Matías Mrejen c,
Elias Mossialos a
a) Department of Health Policy, London School of Economics and Political Science, London, WC2A 2AE, United Kingdom
b) Fundação Getúlio Vargas, São Paulo, Brazil
c) Instituto de Estudos para Políticas de Saúde (IEPS), São Paulo, Brazil