Hospitals continued to perform these eight overused procedures in 2020, analysis of Medicare data shows
Lown Institute
BY Aaron Toleos
May 17, 2022
Executive Summary
by Joaquim Cardoso
The Health Revolution
Multidisciplinary Research Institute
May 19, 2022
- From March-December 2020, hospitals delivered more than 100,000 low-value procedures to Medicare beneficiaries; that’s one every four minutes on average.
- Of the 100,000 procedures, 45,000 were unnecessary coronary stents and 30,000 were unnecessary back surgeries.
- From June to December 2020, with no vaccines available to vulnerable older adults, hospitals delivered low-value services to Medicare patients at rates similar to 2019.
- All of the hospitals on the US News Honor Roll ranking had rates of coronary stent overuse higher than the national average in 2020, and four had rates at least twice that.
- Our health system would also save an estimated $500 million if we didn’t put coronary stents into people without symptoms.
The nation’s hospitals performed more than 100,000 unnecessary and potentially harmful procedures on older patients between March and December 2020, according to a new analysis by the Lown Institute, a healthcare think tank.
Coronary stents and back surgeries were among the most-performed unnecessary procedures over this period.
Coronary stents and back surgeries were among the most-performed unnecessary procedures over this period.
The analysis of Medicare claims data shows that thousands of vulnerable patients were admitted to U.S. hospitals during the height of the pandemic, before COVID-19 vaccines were approved, for procedures that offer little to no clinical benefit or were more likely to harm patients than help them.
The analysis of eight unnecessary and potentially harmful procedures is the first to measure rates of overuse at U.S. hospitals during the COVID-19 pandemic.
… thousands of vulnerable patients were admitted to U.S. hospitals during the height of the pandemic, before COVID-19 vaccines were approved, for procedures that offer little to no clinical benefit or were more likely to harm patients than help them.
“You couldn’t go into your local coffee shop, but hospitals brought people in for all kinds of unnecessary procedures,” said Vikas Saini, MD, president of the Lown Institute.
“The fact that a pandemic barely slowed things down shows just how deeply entrenched overuse is in American healthcare.”
“You couldn’t go into your local coffee shop, but hospitals brought people in for all kinds of unnecessary procedures,”…
“The fact that a pandemic barely slowed things down shows just how deeply entrenched overuse is in American healthcare.”
Number of procedures, Mar-Dec 2020
Volume of eight low-value procedures in U.S. hospitals per Medicare claims
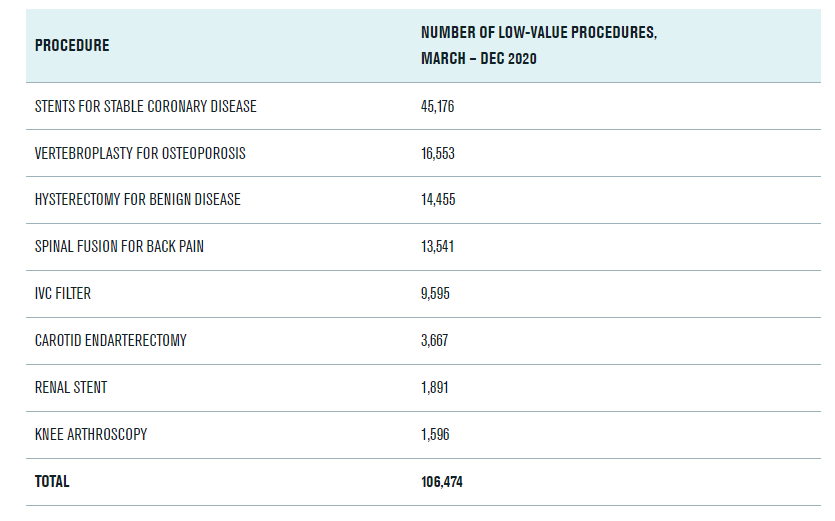
Coronary stents were the most overused by volume of all the procedures.
Across the country, approximately one in five met criteria for overuse, including at some of the nation’s most well-regarded hospitals.
For example, among the U.S. News top 20 hospitals, all had rates of coronary stent overuse above the national average, and four had rates at least double that: Cleveland Clinic (44%), Houston Methodist Hospital (44%), Mt. Sinai (42%), and Barnes Jewish Hospital (42%).
“We’ve known for over a decade that we shouldn’t be putting so many stents into patients with stable coronary disease, but we do it anyway,” said Dr. Saini. “As a cardiologist, it’s frustrating to see this behavior continue at such high levels, especially during the pandemic.”
“We’ve known for over a decade that we shouldn’t be putting so many stents into patients with stable coronary disease, but we do it anyway …As a cardiologist, it’s frustrating to see this behavior continue at such high levels, especially during the pandemic.” — Dr. Saini –

UNNECESSARY CORONARY STENTS
Hospitals performed more than 45,000 coronary stents from March-December 2020 that met criteria for overuse.
Coronary stenting, in which a wire mesh stent is used to open a blocked artery, has shown to be no more beneficial than medication therapy alone for patients with stable coronary disease.
What’s at stake?
Risks of stenting include blood clots that can lead to stroke or heart attack, injury to the heart arteries, infection at the catheter site, allergic reaction to the dye or contrast used, and kidney damage from the dye or contrast.
Additionally, every 1000 low-value coronary stents performed in hospitals is associated with 9 hospital-acquired conditions or patient safety events (not counting the risk of contracting COVID-19).
Our health system would also save an estimated $500 million if we didn’t put coronary stents into people without symptoms.
Our health system would also save an estimated $500 million if we didn’t put coronary stents into people without symptoms.
Which hospitals placed the most low-value stents in 2020?
Among general hospitals (not specialty hospitals) the worst offenders for unnecessary stenting were NYU Langone Medical Center, St Francis Hospital, and Mt. Sinai Hospital in the New York City area, and Scripps Memorial Hospital and Cedars-Sinai Medical Center in Southern California.
For each of these hospitals, low-value stents made up at least one third of all of the stents placed in 2020.
STENTS, U.S. NEWS HOSPITALS
All 20 hospitals on the U.S. News Honor Roll had rates of coronary stent overuse above the national average in 2020. Four hospitals (Cleveland Clinic, Houston Methodist Hospital, Mount Sinai Hospital, and Barnes Jewish Hospital) had overuse rates at least double the national average.
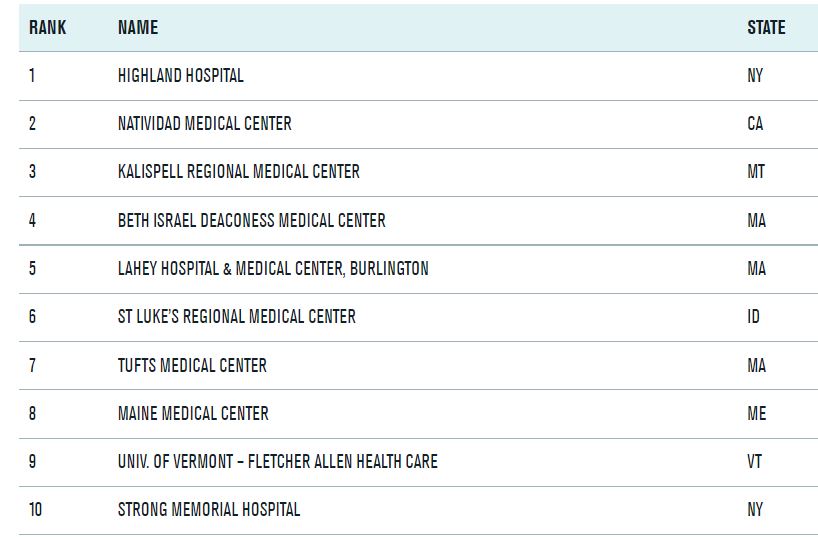
TOP HOSPITALS, AVOIDING OVERUSE
These are the top 50 hospitals for avoiding overuse on the 2022 Lown Hospitals Index for Social Responsibility.
This ranking includes overuse of eight common low-value procedures and four low-value tests. Data for these rankings comes from 2018–2020 Medicare claims.
TOP 10 LIST
BOTTOM 50 HOSPITALS, AVOIDING OVERUSE
These are the 50 lowest ranked hospitals for Avoiding Overuse on the 2022 Lown Hospitals Index for Social Responsibility. This ranking includes overuse of eight common low-value procedures and four low-value tests. Data for these rankings comes from 2018–2020 Medicare claims.
See the original publication
Methodology
For this analysis, the Lown Institute used data from the 100% Medicare claims database from January — December 2020 to evaluate volume of overuse for eight common low-value procedures.
Procedures and overuse criteria were based on our previously published research into measurement of low-value care at hospitals.
Panel Discussion: Join us May 17, 2022 at 1 p.m. ET for a live event as we discuss our latest overuse findings, featuring the Lown Institute’s Vikas Saini, Shannon Brownlee, and Kelsey Chalmers:
METHODOLOGY, OVERUSE DURING COVID
The Lown Institute used data from the 100% Medicare claims database from January — December 2020 to evaluate overuse of eight common low-value services. Procedures and overuse criteria were based on our previously published research into measurement of low-value care at hospitals. Procedures included were:
Arthroscopic knee surgery — Surgery to remove damaged cartilage or bone in the knee using an arthroscope (tiny camera). Defined as overuse for patients with osteoarthritis or “runner’s knee” (damaged cartilage). Excluding patients with meniscal tear.
Carotid endarterectomy — Procedure to remove plaque buildup from a carotid (neck) artery in a patient to prevent stroke. Considered overuse when performed on female patients without stroke symptoms or history of stroke.
Coronary artery stenting — Procedure to place a stent or balloon in a coronary artery. Defined as overuse when performed on patients with stable heart disease (not having a heart attack or unstable angina). Excluding patients with past diagnosis of unstable angina or heart attack within the past two weeks, or any procedures performed in the emergency department.
Hysterectomy — Procedure to remove the uterus. Considered overuse for patients without a diagnosis of cancer or carcinoma in situ.
Inferior Vena Cava (IVC) filter — Procedure to place a filter (a medical device) in the large vein in the abdomen to prevent blood clots from moving to the lungs. Considered overuse for all patients except those with history of multiple pulmonary embolism.
Renal artery stenting — Procedure to place a stent or balloon in the renal (kidney) artery. Considered overuse for patients with high blood pressure or plaque buildup in the artery. Excluding patients that had diagnosis of fibromuscular dysplasia of the renal artery (abnormal twisting of the blood vessels).
Spinal fusion/laminectomy — Procedure to fuse vertebrae together (spinal fusion) or remove part of a vertebra (laminectomy). Defined as overuse for patients with low-back pain, excluding patients with radicular symptoms, trauma, herniated disc, discities, spondylosis, myelopathy, radiculopathy, radicular pain or scoliosis.
Vertebroplasty — Procedure to inject cement into the vertebrae to relieve pain from spinal fractures. Considered overuse for patients with spinal fractures caused by osteoporosis. Excluding patients with bone cancer, myeloma, or hemangioma.
Methodology
For this analysis, the Lown Institute used data from the 100% Medicare claims database from January — December 2020 to evaluate volume of overuse for eight common low-value procedures.
Procedures and overuse criteria were based on our previously published research into measurement of low-value care at hospitals.
Panel Discussion: Join us May 17, 2022 at 1 p.m. ET for a live event as we discuss our latest overuse findings, featuring the Lown Institute’s Vikas Saini, Shannon Brownlee, and Kelsey Chalmers:
METHODOLOGY, OVERUSE DURING COVID
The Lown Institute used data from the 100% Medicare claims database from January — December 2020 to evaluate overuse of eight common low-value services. Procedures and overuse criteria were based on our previously published research into measurement of low-value care at hospitals. Procedures included were:
Arthroscopic knee surgery — Surgery to remove damaged cartilage or bone in the knee using an arthroscope (tiny camera). Defined as overuse for patients with osteoarthritis or “runner’s knee” (damaged cartilage). Excluding patients with meniscal tear.
Carotid endarterectomy — Procedure to remove plaque buildup from a carotid (neck) artery in a patient to prevent stroke. Considered overuse when performed on female patients without stroke symptoms or history of stroke.
Coronary artery stenting — Procedure to place a stent or balloon in a coronary artery. Defined as overuse when performed on patients with stable heart disease (not having a heart attack or unstable angina). Excluding patients with past diagnosis of unstable angina or heart attack within the past two weeks, or any procedures performed in the emergency department.
Hysterectomy — Procedure to remove the uterus. Considered overuse for patients without a diagnosis of cancer or carcinoma in situ.
Inferior Vena Cava (IVC) filter — Procedure to place a filter (a medical device) in the large vein in the abdomen to prevent blood clots from moving to the lungs. Considered overuse for all patients except those with history of multiple pulmonary embolism.
Renal artery stenting — Procedure to place a stent or balloon in the renal (kidney) artery. Considered overuse for patients with high blood pressure or plaque buildup in the artery. Excluding patients that had diagnosis of fibromuscular dysplasia of the renal artery (abnormal twisting of the blood vessels).
Spinal fusion/laminectomy — Procedure to fuse vertebrae together (spinal fusion) or remove part of a vertebra (laminectomy). Defined as overuse for patients with low-back pain, excluding patients with radicular symptoms, trauma, herniated disc, discities, spondylosis, myelopathy, radiculopathy, radicular pain or scoliosis.
Vertebroplasty — Procedure to inject cement into the vertebrae to relieve pain from spinal fractures. Considered overuse for patients with spinal fractures caused by osteoporosis. Excluding patients with bone cancer, myeloma, or hemangioma.
Originally published at https://lowninstitute.org on May 17, 2022.
Names mentioned
Vikas Saini, MD, president of the Lown Institute
Shannon Brownlee, and Kelsey Chalmers