Stat
By K. Jane Muir
Jan. 13, 2022
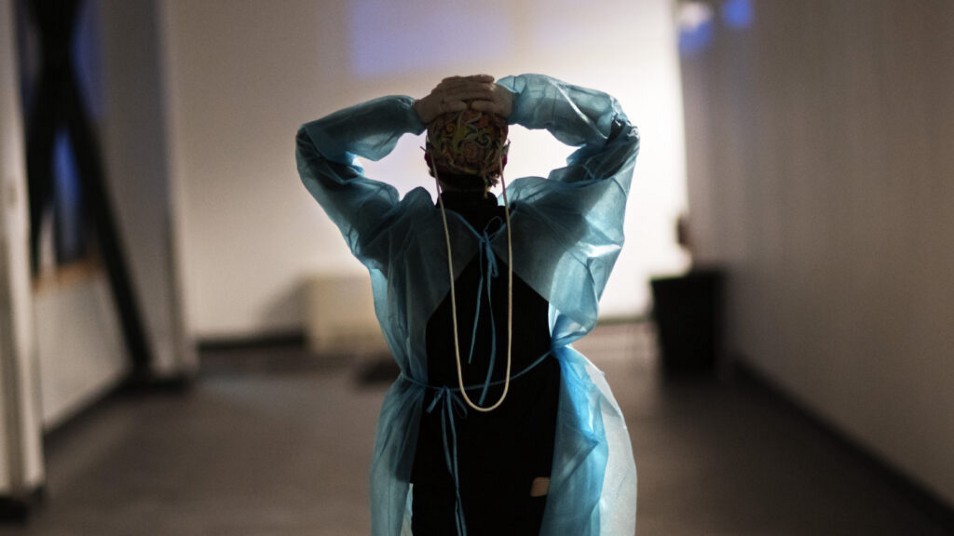
It’s been said so often it’s almost trite: Burnout among nurses drags down hospitals’ quality of care, hollows out the ranks of nurses, and smashes to smithereens any resilience they might have built.
But just as plain as the human tragedy of burnout and attrition in this group of health care workers is the frankness of its remedy:
What ails our nation’s nurses can be solved with
- changes in how they are paid,
- an infusion of cash to support them, and
- policies that link nurse burnout and attrition rates to hospitals’ bottom lines.
Academics have linked nurse burnout to job turnover, which typically costs a hospital between $3.6 to nearly $7 million a year.
Beyond its direct financial costs, their turnover also reduces the quality of patient care and leaves health care teams highly fragmented.
As an emergency department nurse and researcher, I’ve watched this fragmentation unfold as nurses care for patients in high-stakes encounters with little knowledge of their colleagues and the skills and expertise they bring.
In a pattern seen well before the pandemic began, nurses are choosing to leave their workplaces, retire, or take more lucrative health care jobs like travel nursing, an arrangement in which nurses work on a temporary contract basis for a hospital commonly through a third-party staffing agency.
Long gone are the days of nurses’ commitment to one hospital, with plans to climb its clinical ladder and truly invest in a single organization’s culture through service and collaboration.
The tsunami of interest in travel nursing is the direct result of nurses feeling undervalued by their home hospitals.
During the pandemic, many have been reassigned from their specialty areas to units with high staffing needs: a neonatal nurse, for example, might be reassigned to care for adult patients, despite being formally trained to care for newborns.
Staff nurses who, given their tenure, deeply understand an institution’s people, culture, and the communities they serve, now orient and work alongside travelers who make three times their wage — or more — for parachuting in and doing the same work.
In the team-based dance that is health care, nurses now work alongside caregivers whose names, competence levels, and styles they’ll barely come to know over their 13-week terms.
I can expect to enter any given shift working with team members I’ve never met before and who may not be working with me a month from now.
Cohesion is eroding because pay structures have become lopsided, and make some nurses feel even more deeply unseen and undervalued.
Today, whether a nurse is a hospital veteran or a well-paid traveler, it’s hard to escape feeling expendable.
Before the pandemic, one-third of nurses reported burnout, and turnover was about 17% per year.
Since the emergence of Covid-19, burnout has hovered around 50% among nurses while turnover rates have risen to between 20% and 30%.
Given the payout for travel nursing, this field has exploded. All these forces make clear that the old nursing models no longer work.
But the solution is both economic and at hand.
Scientific models that tabulate the financial impacts of burnout and turnover help explain the economic power and cost savings of investing in burnout reduction programs.
In a modeling study I conducted with several colleagues at the University of Virginia, we determined that hospitals that invest in burnout reduction programs — everything from safe staffing to well-being initiatives to meaningful raises and bonuses and clear lines for professional mobility — spend about 30% less on burnout-related costs.
And new nurses who work at such burnout-savvy hospitals tend to stay at their jobs about 20% longer.
… hospitals that invest in burnout reduction programs … spend about 30% less on burnout-related costs
Embedded within the direct savings achieved by burnout reduction are powerful indirect benefits.
Less attrition means health care colleagues know one another, instead of each day being like a pick-up football game.
And that cohesion and collegiality is tied to fewer adverse health care events — errors of commission and omission — all of which ensure a hospitals’ sound economy. Paying attention to burnout reduction pays.
Hospitals often measure quality via markers of good care that are closely tied to their reimbursement rates and cashflow.
So while following protocols to prevent catheter-acquired infections, pressure ulcers, and falls are obviously good for patients, they’re also essential to hospitals’ overall economic health.
Like those measures, the economic case for investing in nurses’ well-being and retention can help buttress a hospital’s bottom line.
Although nurses are central to ensuring that quality metrics are met, which is directly tied to how much hospitals are paid, their work tends to be invisible within hospitals’ economies.
Nurses and the work they do are routinely undervalued: their work “comes with the room.”
It’s time to tie hospitals’ balance sheets, along with their accreditation status and government reimbursement rates, to the health and well-being of their nursing staffs.
It’s time to tie hospitals’ balance sheets, along with their accreditation status and government reimbursement rates, to the health and well-being of their nursing staffs.
By elevating nurses’ value with money (through improved wages, hazard pay, and regular bonuses) and agency (more equitable workloads, less burdensome recordkeeping, and regular opportunities to lead and be heard), they will stay committed to their workplaces.
Money might not mean the end of burnout, but it will slow the hemorrhage of nurses and make them feel seen, valued, and invested in.
And while money for raises and perks talks, so does follow-through. Hospitals must commit to regular and rigorous assessments to track nurse burnout in the same way they keep tabs on infections, errors, and falls.
These changes will make hospitals more aware of the bottom-line impact of valuing nurses, more able to nimbly adjust salaries and bonus cycles, more likely to expand well-being programs and professional development practices to anticipate and prevent nurse burnout and attrition before it happens.
Health systems must also commit to fewer travel nurses, instead taking a “whatever it takes” approach to hire and retain staff nurses.
Finally, hospitals can commit to hiring more nurses into leadership positions in their institutions as a cost-effective mechanism to improve patient care delivery and the issues facing the largest health workforce: nurses.
About the author
K. Jane Muir is an emergency department nurse, researcher, and family nurse practitioner student at the University of Virginia who will begin a post-doctoral fellowship through the National Clinician Scholars Program at the University of Pennsylvania in July 2022.
Originally published at https://www.statnews.com on January 13, 2022.