WHO
André Ilbawi, Cherian Varghese
Executive WHO editors and writers
February 2020
Purpose and scope
In 2017, by adopting World Health Assembly resolution WHA70.12 on cancer prevention and control, governments committed themselves to accelerating action against cancer.
This WHO Report on Cancer, led by WHO and prepared with the IARC, fulfils the mandate given to WHO.
Its purpose is to provide guidance for policy-makers in formulating a response to their national cancer burden by showing that cancer can be controlled as a public health priority by making strategic investments.
It thus describes priority policies and programmes in cancer control and evidence-based interventions along the cancer continuum. It sets an agenda for accelerated action to achieve political commitments.
The main target audience is government policy-makers, particularly in LMIC.
Its messages are, however, relevant to groups in countries at all income levels, including nongovernmental organizations, philanthropic foundations, academic institutions, the private sector and people living with cancer and their families.
Controlling cancer will require the best efforts of: governments to set policies and prioritize investments, communities to mobilize action, individuals to make healthy choices and use health care services, professional societies to strengthen coordination and complement capacity, industry to promote access and innovation and development partners and donors to make strategic investments.
The report seeks to change the dialogue on cancer from one based on fear of death, financial catastrophe, uncertainty and resignation (Box 1) to a positive message that cancer can be controlled through strategic, high-impact investments in programmes, policies and services.
Pragmatic decision-making and evidence-based interventions can yield value for money and sustainable development
Structure of the Report
The first section makes the case for accelerating action to control cancer globally.
The second describes effective action that can be taken along the continuum of cancer, from prevention through care, and form the basis for policies and programmes.
The last section provides guidance on decision-making, financing and implementing cancer control interventions.
The report complements the IARC World Cancer Report[1] (2), to be launched concurrently, as well as WHO global reports on tobacco[2] (5) and alcohol[3] (6).
The IARC report addresses the impact of cancer on the world, including the burden and trends in cancer, the known causes of certain cancers, the biological processes and research on the prevention of particular tumour types.
It provides the most up-to-date science on cancer.
This Report indicates how that science can be translated into policies and programmes for action.
The three key messages for policy-makers are as follows.
1. Globally, the cancer burden will increase by at least 60% over the next two decades, straining health systems and communities.
Cancer is a significant, growing public health concern (chapter 1). It is already responsible for one in six deaths globally, and the burden on individuals, communities, health systems and economies will continue to increase (chapter 2).
2. There have been rapid advances in cancer diagnosis and treatment; however, selection of programmes and products has been inefficient and uninformed, and access to effective services has been profoundly inequitable.
Cancer control can be a highly beneficial investment (chapter 2). If strategic programmes are prioritized, investments in cancer care can have a positive return, saving lives, reducing suffering and promoting equity, economic growth and increased productivity (chapter 2 and 7).
3. Countries should select and implement a set of prioritized interventions that are feasible for their health systems, adapted to their epidemiological burden and available to people of all ages and to disadvantaged groups.
No country can take on the entire cancer agenda; each must set priorities and address them in a phased manner.
Many current cancer control strategies do not adhere to global best practices and are not adapted to the capacity of national health systems (chapters 4 and 5), resulting in inappropriate resource allocation or diversion of resources and potential harm to patients and communities.
Evidence-based policies and programmes should be formulated (chapter 6) and monitored to ensure effective, high-quality care (chapter 8).
Coordination and collaboration are essential for successful implementation.
Annex 1 lists WHO tools and resources for cancer control, Annex 2 provides a glossary of terms used in this publication, and Annex 3 provides profiles of cancer control in countries and WHO regions. The country profiles are online.
BOX: Understanding cancer
A response to the increasing cancer burden requires accurate understanding of the disease and the potential impact of programmes and policies.
“Cancer” is a generic term for a large group of diseases that can affect any part of the body. A defining feature is the rapid creation of abnormal cells that grow beyond their usual boundaries and can then spread to other organs and tissues, a process referred to as metastasis.
Metastases are a common cause of death from cancer. Abnormal cells generally arise because of alterations in the DNA of cells that result in the growth and spread of related cells.
Such changes are multifactorial in origin, involving environmental agents (carcinogens or infections), alterations in developmental pathways, chance errors in DNA replication, impairments in the immune system and other factors.
The International Classification of Diseases (revision 11) lists more than 600 types of cancer, most of which require unique diagnostic and management approaches.
SOME MYTHS ABOUT CANCER
“Cancer cannot be prevented.”
· Between one third and one half of cancers can be prevented by eliminating or minimizing exposure to risk factors.
· The most common cause of cancer is tobacco use,
which accounts for 25% of all cancer deaths globally (chapter 3)[4] (1).
“Cancer is a death sentence.”
· One of the most important messages for the public is that cancer can be cured when detected early and treated effectively (chapter 4).
· It should not be viewed as a death sentence.
· Similarly, policy-makers should understand that cancer services can be cost-effective, and investing in cancer control will save lives (chapter 2).
“Cancer is contagious.”
· Cancerous cells cannot be transmitted from one person to another.
· Physical contact with a cancer patient should not be feared or discouraged.
· Certain infections, such as with human papillomavirus or hepatitis viruses, are known causes of cancer and can be spread from one person to another (chapter 3); highly-effective vaccines can prevent both HPV and hepatitis B.
“Everything causes cancer.”
· There is significant misinformation about what does and does not cause cancer and about individual relative risks.
· The IARC Monographs series is the definitive reference for evidence-based causes of cancer (chapter 3)[5] (2).
“Over-the-counter remedies can cure cancer.”
· Standard cancer treatments have been rigorously evaluated and should be prescribed and administered only by government-approved health care professionals (chapter 5).
· Replacing conventional treatment with over-the-counter products has been linked to lower survival[6] (3).
· Some complementary therapies can be used to support evidence-based, standard care in close consultation with government-approved health care professionals[7] (4).
· Accepted, effective cancer treatment generally requires a combination of surgery, medicines and radiotherapy (chapter 5).
“Children don’t develop cancer.”
· Childhood cancers accounts for approximately 2–3% of all cancer cases and require a unique approach to provide optimal care.
· Most childhood cancers are highly curable, reaching greater than 90% in some HIC, if they are promptly diagnosed and patients are referred and given multidisciplinary care (chapter 5).
“The latest equipment and medicine should be used for cancer treatment.”
· Some recent innovations in cancer treatment have improved outcomes;
· however, not all new cancer treatments have a high impact, and established standards may be more effective, feasible and appropriate.
· Policy-makers should refer to health technology agencies, and patients should seek discussions with trained health professionals in making decisions (chapters 5 and 7).

Comprehensive cancer control
Cancer control requires a comprehensive approach.
Generally, interventions can be organized thematically along the “cancer continuum”, from prevention to survivorship or end-of-life care, each of which requires unique activities and supporting policies (Fig. i.1).
Figure i.1. Interventions along the cancer continuum and examples of levels of care.
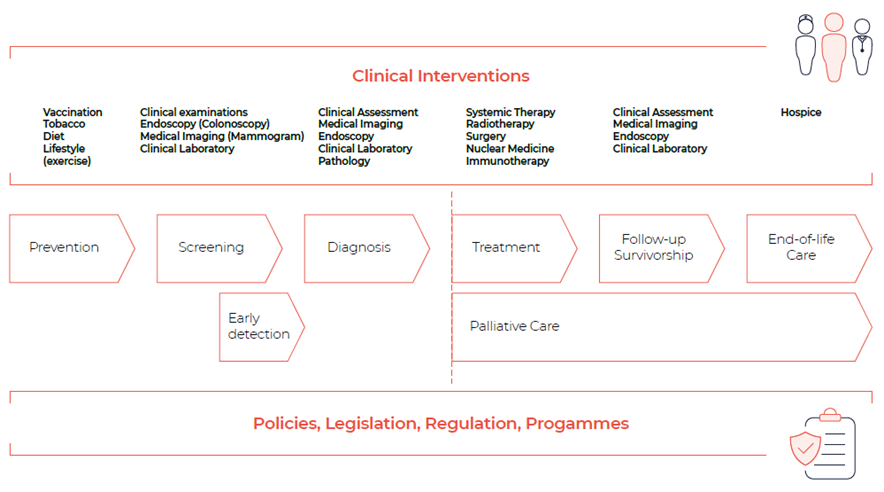
Source: adapted from reference 7[8].
Primary prevention of cancer consists of modification of factors that increase the risk of cancer (see chapter 3).
The goal of early detection is to identify cancer or precancerous lesions as early as possible by one of two distinct approaches: early diagnosis or screening (see chapter 4).
The main diagnostic steps are assessing the anatomical extent of disease and the cancer type and subtype.
Common cancer treatments are systemic therapy (e.g. chemo-, endocrine and targeted therapy), surgery, radiotherapy, nuclear medicine, bone-marrow transplantation and cancer cell therapy.
Survivorship care is the provision of services after completion of treatment for cancer and includes surveillance to identify recurring cancer and any toxicity of treatment (see chapter 5).
Palliative care is an approach to improving the quality of life of patients with life-threatening diseases and of their families and is part of the management strategy at the time of a cancer diagnosis[9] (8).
Effective planning of cancer control requires contextualization to the country situation, with information from population-based cancer registries and information systems (see chapter 6).
Services and interventions must be integrated, multisectoral and inter-disciplinary. An integrated national cancer response must be appropriate for the capacity of the health service and the epidemiological burden.
This report sets forth an agenda for action in comprehensive cancer control for today and the next decade.
Box 1: Cancer and UHC: Providing care for all
Cancer control must be a pillar of any strategy towards achieving UHC, an SDG included in Agenda 2030 (target 3.8), and must be founded on the principles of equitable access to health services, financial protection of the whole population and prioritization of interventions that provide value for money.
The impact of the cancer burden on patients, communities and economies summarized in this Report indicate that the public health and policy approach must be based on UHC.
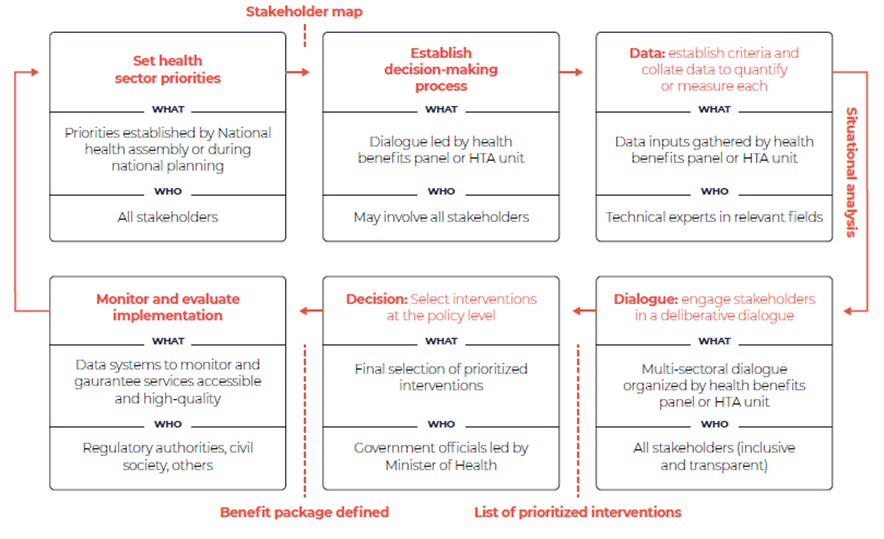
The interventions in a country’s benefits package should be chosen in accordance with these principles and the resources and capacity available (Box 1) and with services defined as essential by WHO, such as “best buys” and the Model List of Essential Medicines (EML) and Diagnostics (EDL), and by other normative agencies.
Both population-based (generally for prevention) and clinical (health services) interventions should be selected.
Any new intervention against cancer included in a benefits package should be scaled up progressively to reach the entire target population before the introduction of new services, consistent with the principles of progressive realization (Fig. i.2).
The growing challenge posed by cancer to our societies can be addressed only if it is based on the objective of achieving UHC and health for all.
Fig. i.2. Identifying and implementing priority interventions as part of UHC
References:
See the original publication
Originally published at https://www.who.int












