Journal of Medical Artificial Intelligence
Victoria Tucci, Joan Saary , Thomas E. Doyle
March, 2022
stevensonedu
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of “The Health Revolution” Institute / AI Health
March 26, 2022
Artificially intelligent technology is revolutionizing healthcare. However, lack of trust in the output of such complex decision support systems introduces challenges and barriers to adoption and implementation into clinical practice.
The authors performed a comprehensive review of the literature to better understand the trust dynamics between medical artificial intelligence (AI) and healthcare expert end-users.
There were nine trust concepts that were consistently identified through both qualitative and quantitative methodologies, however, were more frequently analyzed qualitatively, including:
- Complexity (5.3% of total articles identified) (2,11);
- Accuracy (5.3%) (12,13);
- Continuous updating of evidence base (7.0%) (12,14,15);
- Fairness (8.8%) (2,4,16,17);
- Reliability (10.5%) (8,13,17–19);
- Education (10.5%) (20–24);
- Interpretability (14.0%) (4,8,19,21,24,25);
- Transparency (28.1%) (2,4,8,11,15–18,21,23,26–30);
Explainability, transparency, interpretability, usability, and education are among the key identified factors thought to influence a healthcare professionals’ trust in medical AI and enhance clinician-machine teaming in critical decision-making healthcare environments.
In order to facilitate adoption of AI technology into medical practice settings, significant trust must be developed between the AI system and the health expert end-user.
ORIGINAL PUBLICATION (full version)

ABSTRACT
Objective:
We performed a comprehensive review of the literature to better understand the trust dynamics between medical artificial intelligence (AI) and healthcare expert end-users.
We explored the factors that influence trust in these technologies and how they compare to established concepts of trust in the engineering discipline.
By identifying the qualitatively and quantitatively assessed factors that influence trust in medical AI, we gain insight into understanding how autonomous systems can be optimized during the development phase to improve decision-making support and clinician-machine teaming.
This facilitates an enhanced understanding of the qualities that healthcare professional users seek in AI to consider it trustworthy.
We also highlight key considerations for promoting on-going improvement of trust in autonomous medical systems to support the adoption of medical technologies into practice.
Background:
Artificially intelligent technology is revolutionizing healthcare.
However, lack of trust in the output of such complex decision support systems introduces challenges and barriers to adoption and implementation into clinical practice.
Methods:
We searched databases including, Ovid MEDLINE, Ovid EMBASE, Clarivate Web of Science, and Google Scholar, as well as gray literature, for publications from 2000 to July 15, 2021, that reported features of AI-based diagnostic and clinical decision support systems that contribute to enhanced end-user trust.
Papers discussing implications and applications of medical AI in clinical practice were also recorded.
Results were based on the quantity of papers that discussed each trust concept, either quantitatively or qualitatively, using frequency of concept commentary as a proxy for importance of a respective concept.
Conclusions:
Explainability, transparency, interpretability, usability, and education are among the key identified factors thought to influence a healthcare professionals’ trust in medical AI and enhance clinician-machine teaming in critical decision-making healthcare environments.
We also identified the need to better evaluate and incorporate other critical factors to promote trust by consulting medical professionals when developing AI systems for clinical decision-making and diagnostic support.
Keywords: Artificial intelligence (AI); trust; healthcare; medical technology adoption; decision support system
Explainability, transparency, interpretability, usability, and education are among the key identified factors thought to influence a healthcare professionals’ trust in medical AI and enhance clinician-machine teaming in critical decision-making healthcare environments.

This is an excerpt of the original publication. For the full version of the paper, please, refer to the original long version of the paper.
Introduction
Rapid development of healthcare technologies continues to transform medical practice ( 1).
The implementation of artificial intelligence (AI) in clinical settings can augment clinical decision-making and provide diagnostic support by translating uncertainty and complexity in patient data into actionable suggestions ( 2).
Nevertheless, the successful integration of AI-based technologies as non-human, yet collaborative members of a healthcare team, is largely dependent upon other team users’ trust in these systems.
Trust is a concept that generally refers to one’s confidence in the dependability and reliability in someone or something ( 3).
We refer to AI as a computer process that algorithmically makes optimal decisions based on criteria utilizing machine learning-based models ( 2).
Although trust is fundamental to influencing acceptance of AI into critical decision-making environments, it is often a multidimensional barrier that contributes to hesitancy and skepticism in AI adoption by healthcare providers ( 4).
Trust is a concept that generally refers to one’s confidence in the dependability and reliability in someone or something
Although trust is fundamental to influencing acceptance of AI into critical decision-making environments, it is often a multidimensional barrier that contributes to hesitancy and skepticism in AI adoption by healthcare providers
Historically, the medical community has sometimes demonstrated resistance to the integration of technology into practice.
For instance, the adoption of electronic health records was met with initial resistance in many locales.
Identified barriers included cost, technical concerns, security and privacy, productivity loss and workflow challenges, among others ( 5).
Therefore, we could expect that similar factors may contribute to the issues related to lack of trust in medical AI, which is also considered a practice-changing technology.
Historically, the medical community has sometimes demonstrated resistance to the integration of technology into practice. For instance, the adoption of electronic health records (EHRs) …
Identified barriers (in EHRs) included cost, technical concerns, security and privacy, productivity loss and workflow challenges, among others (5). Therefore, we could expect that similar factors may contribute to the issues related to lack of trust in medical AI …
It is imperative to elucidate the factors that impact trust in the output of AI-based clinical decision and diagnostic support systems; enhancing end-user trust is crucial to facilitating successful human-machine teaming in critical situations, especially when patient care may be impacted.
Ahuja et al. [2019] summarize numerous studies that have assessed the importance of optimizing medical AI systems to enhance teaming and interactions with clinician users ( 6).
Similarly, Jacovi et al. [2021] outline several concepts established in the discipline of engineering that are well understood to contribute to increased end-user trust in AI systems, including, but not limited to, interpretability, explainability, robustness, transparency, accountability, fairness, and predictability ( 7).
However, in contrast to the engineering literature, there appears to be a gap in the medical literature regarding exploration of the specific factors that contribute to enhanced trust in medical AI amongst healthcare providers.
We, therefore, wished to address this gap by performing a review of the literature to better understand the trust dynamics between healthcare professional end-users and medical AI systems.
Further, we sought to explore the key factors and challenges that influence end-user trust in the output of decision support technologies in clinical practice and compare the identified factors to established concepts of trust in the domain of engineering.
We recognize the challenges in AI research regarding inconsistency and lack of universally accepted definitions of key trust concepts.
We recognize the challenges in AI research regarding inconsistency and lack of universally accepted definitions of key trust concepts.
Since these are terms that are relevant for understanding the concept of trust, we accepted that terminology may be applied inconsistently throughout the literature.
The aim of this paper is to delineate the qualitatively and quantitatively assessed factors that influence trust in medical AI to better understand how autonomous systems can be optimized to improve both decision-making support and clinician-machine teaming.
A quantitative summary of the discourse in the healthcare community regarding factors that influence trustworthiness in medical AI will provide AI researchers and developers relevant input to better direct their work and make the outcomes more clinically relevant.
We specifically focus on healthcare professionals as the primary end-users of medical AI systems and highlight challenges related to trust that should be considered during the development of AI systems for clinical use.
A literature review is appropriate at this time as there currently does not exist a comprehensive consolidation of available literature on this topic.
As such, this review is an important primary step to synthesize the current literature and consolidate what is already known about trust in medical AI amongst healthcare professionals.
Since this has not been previously performed, it will enable identification of knowledge gaps and contribute to further understanding by summarizing relevant evidence.
By first collating information in the form of a literature review, this paper describes the breadth of available research and provides a foundational contribution to an eventual evidence-based conceptual understanding.
We aim to facilitate an understanding of the landscape in which this information applies to make valuable contributions to medical AI.
By elucidating the discourse in the medical community regarding key factors related to trust in AI, this paper also provides the foundation for further research into the adoption of medical AI technologies, as well as highlights key considerations for promoting trust in autonomous medical systems and enhancing their capabilities to support healthcare professionals.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://jmai.amegroups.com/article/view/10.21037/jmai-21-25/rc).
Methods
See the original publication

Results
We aimed to highlight the medical AI trust concepts/factors that are most frequently discussed amongst healthcare professionals by using frequency of discussed topics as a proxy for importance.
The concepts were categorized according to whether they were qualitatively and/or quantitatively evaluated in the respective articles in which they were investigated.
The data is graphically displayed in two distinct presentation formats to highlight comparisons between the number and type of AI trust concepts that were quantified compared to those that were presented qualitatively in the literature (see Figures 2,3).
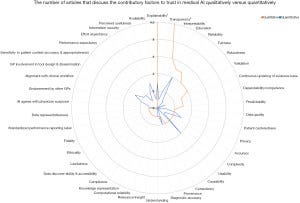
A quantitative presentation of the number of papers that discuss AI trust-related concepts identifies the areas of current focus of research endeavor.
Identifying the key factors and how commonly each are found thereby highlights the most common as well as under-represented (or possibly overlooked) concepts.
Overall, there were a total of 42 factors identified that contribute to enhanced end-user trust in medical AI systems.
Of these 42 factors,
- 10 were solely analyzed quantitatively,
- 16 were solely analyzed qualitatively, and
- 16 were examined both qualitatively and quantitatively.
Note that all percentages are based on the total number of articles identified.
There were nine trust concepts that were consistently identified through both qualitative and quantitative methodologies, however, were more frequently analyzed qualitatively, including:
- Complexity (5.3% of total articles identified) (2,11);
- Accuracy (5.3%) (12,13);
- Continuous updating of evidence base (7.0%) (12,14,15);
- Fairness (8.8%) (2,4,16,17);
- Reliability (10.5%) (8,13,17–19);
- Education (10.5%) (20–24);
- Interpretability (14.0%) (4,8,19,21,24,25);
- Transparency (28.1%) (2,4,8,11,15–18,21,23,26–30);
The sixteen trust factors that were only analyzed qualitatively included:
- Data representativeness (1.8%) (17);
- Standardized performance reporting label inclusion (1.8%) (12);
- Fidelity (1.8%) (25);
- Ethicality (1.8%) (25);
- Lawfulness (1.8%) (25);
- Data discoverability and accessibility (1.8%) (15);
- Compliance (1.8%) (15);
- Knowledge representation (1.8%) (29);
- Relevance/insight (1.8%) (11);
- Consistency (3.5%) (42,43);
- Causability (3.5%) (21,27);
- Predictability (5.3%) (8,13,25);
- Dependability/competence (5.3%) (8,19,28);
- Validation (7.0%) (4,8,17,25);
- Robustness (7.0%) (2,16,17,25);
The additional 10 factors that were only analyzed through quantitative methods included:
- Availability (1.8%) (44);
- Effort expectancy (1.8%) (45);
- Endorsement by other general practitioners (GPs (1.8%) (46);
- AI agreement with physician suspicions (1.8%) (47);
- Information security (3.5%) (48,49);
- Performance expectancy (3.5%) (45,50);
- Sensitivity to patient context (3.5%) (46,51);
- Alignment with clinical workflow (3.5%) (46,52);
- Perceived usefulness (5.3%) (44,52,53);
- GP involvement in tool design and dissemination (5.3%) (42,43,46).
Overall, explainability was discussed consistently across 23 included articles, and was the factor examined the most often.
This suggests it is one of the most important concepts for trust in medical AI.
Overall, explainability was discussed consistently across 23 included articles, and was the factor examined the most often.
This suggests it is one of the most important concepts for trust in medical AI.
In articles that included both qualitative and quantitative examination of concepts, the trust factors that were more often quantitatively analyzed tended to focus on provenance ( 46, 54), usability ( 42– 44), and privacy ( 52, 55, 56) (see Figures 2,3).
In articles that included both qualitative and quantitative examination of concepts, the trust factors that were more often quantitatively analyzed tended to focus on provenance, usability, and privacy .
This reveals an apparent gap in the literature; these concepts may benefit from further qualitative analysis amongst medical professional populations to provide AI researchers more insight into aspects to consider when developing AI technology to facilitate clinical adoption.
Among the articles that solely explored AI trust concepts quantitatively, education and usability were discussed most often.
Other top contributory factors to enhanced end-user trust in medical AI identified quantitatively were explainability, privacy, GP involvement in tool design and dissemination, and perceived usefulness (see Figures 2,3).
Among the articles that solely explored AI trust concepts quantitatively, education and usability were discussed most often
Other top contributory factors to enhanced end-user trust in medical AI identified quantitatively were explainability, privacy, GP involvement in tool design and dissemination, and perceived usefulness
Considering the entirety of the available literature, and despite more articles focusing on qualitative analysis of this concept, explainability appears to be the most important factor to enhancing trust in medical AI systems according to healthcare professionals.
… explainability appears to be the most important factor to enhancing trust in medical AI systems according to healthcare professionals.
Discussion
Substantial investments in AI research and regulation suggest that this technology could become an essential clinical decision-making support tool in the near future ( 57).
Substantial investments in AI research and regulation suggest that this technology could become an essential clinical decision-making support tool in the near future
Existing literature in the domain of machine learning discusses methods that have been applied to successfully train data-driven mathematical models to support healthcare decision-making processes ( 2, 58, 59).
This is a common basis for the engineering of medical AI, which has future applications in clinical decision-making and complex domains, like precision medicine, to optimize patient health outcomes ( 60).
Similarly, the CONSORT-AI reporting guideline extension provides direction for research investigators to help promote transparency and completeness in reporting clinical trials for medical AI interventions ( 61).
As such, it may enhance trust in the AI technology upon clinical integration and support clinical decision-making processes by facilitating critical appraisal and evidence synthesis for interventions involving medical AI.
The use of this reporting guideline is important to consider for clinical trials involving AI to promote end-user trust by ensuring a comprehensive evaluation of the technology before deployment and integration into clinical environments.
… the CONSORT-AI reporting guideline extension provides direction for research investigators to help promote transparency and completeness in reporting clinical trials for medical AI interventions ( 61). The use of this reporting guideline is important to consider for clinical trials involving AI …
However, while there is substantial discussion regarding the technical and engineering aspects of such intelligent systems, healthcare professionals often remain hesitant to adopt and integrate AI into their practice ( 62).
However, while there is substantial discussion regarding the technical and engineering aspects of such intelligent systems, healthcare professionals often remain hesitant to adopt and integrate AI into their practice
As such, it is necessary to better understand the factors that influence the trust relationship between medical experts and AI systems. This will not only augment decision-making and diagnostics, but also facilitate AI adoption into healthcare settings.
…it is necessary to better understand the factors that influence the trust relationship between medical experts and AI systems.
This will not only augment decision-making and diagnostics, but also facilitate AI adoption into healthcare settings.
The unique aspect of our study is the focus on a synthesis of factors that are considered contributory to the enhancement of trust in the output of medical AI systems from the perspective of healthcare experts.
We identified a disparity in the volume of literature that qualitatively versus quantitatively discusses each AI trust factor. This highlights a gap in the analytic assessment of AI trust factors and identifies trust topics that still require quantification amongst the medical community.
We identified a disparity in the volume of literature that qualitatively versus quantitatively discusses each AI trust factor.
This highlights a gap in the analytic assessment of AI trust factors and identifies trust topics that still require quantification amongst the medical community.
Explainability is discussed the most frequently overall across the qualitative and quantitative literature, and it is thus considered to be the most important factor influencing levels of trust in medical AI.
Explainability is discussed the most frequently overall across the qualitative and quantitative literature, and it is thus considered to be the most important factor influencing levels of trust in medical AI.
Our findings tend to be consistent with literature in both medicine and engineering that have a large focus on supporting clinicians in making informed judgments using clinically meaningful explanations and developing technical mechanisms to engineer explainable AI ( 40, 63).
Since frequency was used as a surrogate for presumed importance, we acknowledge that there may exist other concepts related to trust in medical AI that are more important to healthcare professionals yet discussed less frequently, and thus may not be fully reflected in this paper.
As well, explainable AI models, like decision trees, come at the expense of algorithm sophistication and are limited by big data ( 2). As such, achieving balance between algorithm complexity and explainability is necessary to enhancing trust in medical AI.
… explainable AI models, like decision trees, come at the expense of algorithm sophistication and are limited by big data ( 2).
As such, achieving balance between algorithm complexity and explainability is necessary to enhancing trust in medical AI.
We note that there is heterogeneity between the medical AI trust factors that are commonly quantified as compared to qualitatively assessed.
For instance, education and usability were important concepts that were frequently quantified in the included literature.
Gaining a foundational background in AI is thought to be conducive to an increased trust and confidence in the system.
By understanding the functionality of AI, healthcare trainees would be able to gradually develop a relationship with such systems ( 20, 24).
For instance, in a recent questionnaire by Pinto Dos Santos et al., 71% of the medical student study population agreed that there was a need for AI to be included in the medical training curriculum ( 64).
… in a recent questionnaire … 71% of the medical student study population agreed that there was a need for AI to be included in the medical training curriculum ( 64).
Further, usability is a component of user experience and is dependent upon the efficacy of AI features in accommodating for, and satisfying, user needs to enhance ease of use ( 65).
Further, usability is a component of user experience and is dependent upon the efficacy of AI features in accommodating for, and satisfying, user needs to enhance ease of use
This is particularly important in clinical decision-making environments where healthcare provider end-users rely on ease of use to make critical judgements regarding patient care.
As such, poor usability, i.e., complex AI user interfaces, can hinder the development of trust in the AI system ( 12).
… poor usability, i.e., complex AI user interfaces, can hinder the development of trust in the AI system
Transparency and interpretability were also common factors particularly among qualitative assessments.
Transparency and interpretability were also common factors particularly among qualitative assessments.
These are also topics of focus in the engineering literature regarding the technical development of trustworthy AI programs ( 7).
Transparency enables clinician users to make informed decisions when contemplating a recommendation outputted by a medical AI system.
It also supports trust enhancement as transparent systems display their reasoning processes.
Transparency enables clinician users to make informed decisions when contemplating a recommendation outputted by a medical AI system.
It also supports trust enhancement as transparent systems display their reasoning processes.
In this way, healthcare professionals can still apply their own decision-making processes to develop differential diagnoses and complement the AI’s conclusions because they can understand the methodical process employed by the system.
It follows that fairness is also an important factor to the user-AI trust relationship in healthcare ( 4, 16).
It follows that fairness is also an important factor to the user-AI trust relationship in healthcare
AI algorithms are inherently susceptible to discrimination by assigning weight to certain factors over others.
AI algorithms are inherently susceptible to discrimination by assigning weight to certain factors over others.
This introduces the risk of exacerbating data biases and disproportionately affecting members of protected groups, especially when under-representative training datasets are used to develop the model ( 2, 66).
As such, implementing explainable and transparent AI systems in medical settings can aid physicians in detecting potential biases reflected by algorithmic flaws.
As such, implementing explainable and transparent AI systems in medical settings can aid physicians in detecting potential biases reflected by algorithmic flaws.
Interpretability was also found to be commonly considered impactful to the AI trust relationship because it allows medical professionals to understand the AI’s reasoning process.
This prevents clinicians from feeling constrained by an AI’s decision ( 67).
Although not quantified, robustness is the ability of a computer system to cope with errors in input datasets and characterizes how effective the algorithm is with new inputs ( 2).
It is also an important factor that is commonly discussed in the engineering discipline as a critical component of trustworthy AI programs.
Even with small changes to the initial dataset, poor robustness can cause significant alterations to the output of an AI model ( 2).
Although not quantified, robustness is the ability of a computer system to cope with errors in input datasets and characterizes how effective the algorithm is with new inputs ( 2).
It is also an important factor that is commonly discussed in the engineering discipline as a critical component of trustworthy AI programs.
Advances in AI capabilities will expand the role of this decision-support technology from automation of repetitive and defined tasks, towards guiding decision-making in critical environments, which is typically performed exclusively by medical professionals.
Advances in AI capabilities will expand the role of this decision-support technology from automation of repetitive and defined tasks, towards guiding decision-making in critical environments, which is typically performed exclusively by medical professionals.
As such, healthcare providers may increasingly rely on AI.
As such, healthcare providers may increasingly rely on AI.
Increased reliance on this technology requires a foundational trust relationship to be established in order to execute effective decision-making; this is also referred to as ‘calibrated trust’ ( 68).
Increased reliance on this technology requires a foundational trust relationship to be established in order to execute effective decision-making; this is also referred to as ‘calibrated trust
As such, our findings are relevant for those working to develop and optimize medical AI software and hardware to facilitate adoption and implementation in healthcare settings.
These results are also relevant to inform healthcare professionals about which AI trust factors are quantified in terms of importance amongst the medical community.
An end-user’s perception of the competence of an AI system not only impacts their level of trust in the technology, but also has a significant influence on how much users rely on AI, and thus impacts the effectiveness of healthcare decisions ( 69).
An end-user’s perception of the competence of an AI system not only impacts their level of trust in the technology, but also has a significant influence on how much users rely on AI …
However … the level of trust in medical AI may not necessarily be positively correlated with clinical or patient outcomes…
They introduce the concept of ‘optimal trust’
However, Asan et al. [2020] explain that the level of trust in medical AI may not necessarily be positively correlated with clinical or patient outcomes ( 2).
They introduce the concept of ‘optimal trust’ and note that trust maximization does not necessarily result in optimal decision-making via human-AI collaboration, since the user accepts the outcomes generated by the AI system without critical judgment.
This can be particularly dangerous in clinical settings where patient life is at risk.
Optimal trust entails maintaining a certain level of mutual skepticism between users and AI systems regarding clinical decisions.
Since both are susceptible to error, the development of AI should incorporate mechanisms to sustain an optimal trust level ( 2, 69).
Optimal trust entails maintaining a certain level of mutual skepticism between users and AI systems regarding clinical decisions.
Since both are susceptible to error, the development of AI should incorporate mechanisms to sustain an optimal trust level .
Our study provides insight into the breadth of factors that may contribute to achieving an optimal trust relationship between human and machine in medical settings and exposes components that may have been previously overlooked and require further consideration.
Our findings are consistent with the notion that incorporation of explainability, transparency, fairness, and robustness into the development of AI systems contributes to achieving a level of optimal trust.
According to our results, these factors are frequently assessed qualitatively in the healthcare literature as topics that are considered important to trusting an AI system for medical professionals.
It follows that quantification of these factors would provide better insight into the demand to incorporate them in medical AI development.
Achieving optimal trust in AI likely entails consideration of a range of factors that are important for healthcare professionals.
However, Figures 2,3 clearly depict that to date, the focus has been skewed to only a few commonly discussed factors, and that numerous other factors may require further consideration during the AI technology engineering and development phase, prior to deployment into clinical settings.
This is important because the consequence of failing to consider this breadth of factors is insufficient trust in the AI system, which itself constitutes a barrier to adoption and integration of AI in medicine.
This is important because the consequence of failing to consider this breadth of factors is insufficient trust in the AI system, which itself constitutes a barrier to adoption and integration of AI in medicine.
We also acknowledge that the discrepancies in linguistics within, and between, professional domains are a limitation of the field and a barrier to a fully comprehensive search strategy.
Although the search strategy was developed to capture relevant articles discussing factors influencing trust in medical AI, it also returned a significant quantity of articles that were not actually discussing trust concepts related to medical AI, but rather focused on direct implications and applications of this technology in healthcare settings.
Although the focus of this paper was a summative assessment of the qualitatively and quantitatively measured factors impacting trust in medical AI, the implications of integrating this technology may also influence trust in AI in healthcare settings.
… the implications of integrating this technology may also influence trust in AI in healthcare settings.
Implementing AI-based decision-support systems inevitably disrupts the physician’s practice model, as they are required to adopt a new thinking process and mechanism for performing a differential diagnosis that is teamed with an intelligent technology.
Willingness to adopt AI, therefore, likely relates in part to the impact of AI on the medical practice, which in turn may affect trust in AI.
Willingness to adopt AI, therefore, likely relates in part to the impact of AI on the medical practice, which in turn may affect trust in AI.
For instance, physicians have been trained with the Hippocratic Oath, thus introducing a machine that can interact, as well as interfere with, the patient-physician relationship may increase hesitancy in trusting and adopting AI.
A recent qualitative survey by Laï et al. [2020] found that while healthcare professionals recognize the promise of AI, their priority remains providing optimal care for their patients ( 62).
A recent qualitative survey by Laï et al. [2020] found that while healthcare professionals recognize the promise of AI, their priority remains providing optimal care for their patients
Physicians generally avoid relinquishing entrusted patient care to a machine if it is not adequately trustworthy. So, integration of medical AI into clinical settings also has deeper philosophical implications.
Physicians generally avoid relinquishing entrusted patient care to a machine if it is not adequately trustworthy. So, integration of medical AI into clinical settings also has deeper philosophical implications.
Lastly, we noted greater expansion of AI applications in certain distinct medical specialties, including dentistry and ophthalmology ( 70, 71).
This confirms that AI adoption in some areas of healthcare may be broader than others, and they tended to be disciplines in which sophisticated technical instrumentation is already commonly utilized.
Lastly, we noted greater expansion of AI applications in certain distinct medical specialties, including dentistry and ophthalmology ( 70, 71).
This confirms that AI adoption in some areas of healthcare may be broader than others, and they tended to be disciplines in which sophisticated technical instrumentation is already commonly utilized.
Limitations of this study
Although the users of AI technology can be diverse, the focus of this paper is limited to the healthcare discipline. We acknowledge that trust relationships with AI systems could significantly differ for other relevant stakeholders such as patients, and insurance providers. As such, the incorporation of more perspectives from unique stakeholders in the medical community may offer a more extensive perspective of the factors contributing to trust in medical AI.
We acknowledge that there are challenges in the realm of AI research regarding the inconsistency and lack of universally accepted definitions of key terms, including transparency, explainability, and interpretability. Given that these are concepts anticipated to be relevant for understanding the concept of trust, we were obligated to accept that terminology may be applied inconsistently in the literature.
We also recognize that although we use frequency of discussed topics as a surrogate for significance, it only reflects a degree of perceived importance, as it is also possible that the current research focus is misdirected, or that concepts deemed important in one discipline would not necessarily translate to those deemed relevant in another discipline using the same medical AI. We acknowledge that this also does not identify the unknown unknowns regarding factors that contribute to trust in medical AI for healthcare providers.
Further, we acknowledge that there may be bias in the categorization of implicit AI trust concepts, as mapping these to an explicit concept was partly based on the authors’ professional judgment; however, established definitions were consulted to increase objectivity when deciding the explicit concepts upon which the implicit ones would be mapped.
The timeframe of this study was limited to articles published beyond the year 2000 until July 2021.
As AI is rapidly developing and the integration of medical AI in clinical practice is becoming more pertinent, we recommend on-going monitoring of this literature, as well as review of other domains that may discuss AI trust concepts that were not identified in this paper.

Conclusions
In order to facilitate adoption of AI technology into medical practice settings, significant trust must be developed between the AI system and the health expert end-user.
Overall, explainability, transparency, interpretability, usability, and education are among the key identified factors currently thought to influence this trust relationship and enhance clinician-machine teaming in critical decision-making environments in healthcare.
There is a need for a common and consistent nomenclature between primary fields, like engineering and medicine, for cross-disciplinary applications, like AI.
We also identify the need to better evaluate and incorporate other important factors to promote trust enhancement and consult the perspectives of medical professionals when developing AI systems for clinical decision-making and diagnostic support.
To build upon this consolidation and broad understanding of the literature regarding the conceptualization of trust in medical AI, future directions may include a systematic review approach to further quantify relevant evidence narrower in scope.
Acknowledgments
We would like to thank the Biomedic.AI Lab at McMaster University for their on-going support and feedback throughout the process of this study. We would also like to thank the Department of National Defense Canada for their funding of the Biomedic.AI Lab activities through the Innovation for Defence Excellence and Security (IDEaS) Program.
References
See the original publication.
Cite this article as:
Tucci V, Saary J, Doyle TE. Factors influencing trust in medical artificial intelligence for healthcare professionals: a narrative review. J Med Artif Intell 2022;5:4.
Originally published at https://jmai.amegroups.com.
About the authors & additional information
Victoria Tucci 1^, Joan Saary2,3, Thomas E. Doyle4,5,6
1Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada;
2Division of Occupational Medicine, Department of Medicine, University of Toronto, Ontario, Canada;
3Canadian Forces Environmental Medicine Establishment, Toronto, Ontario, Canada;
4Department of Electrical and Computer Engineering, McMaster University, Hamilton, Ontario, Canada;
5School of Biomedical Engineering, McMaster University, Hamilton, Ontario, Canada;
6Vector Institute of Artificial Intelligence, Toronto, Ontario, Canada