Insights from the appointment-based model (ABM) which is a proactive approach to pharmacy practice …
… that synchronizes chronic prescription refills and couples it with regularly scheduled patient-pharmacist appointments to optimize medication management
This is a republication of the paper below, with the title above, preceded by an Executive Summary by the Editor of this Blog. For a full version of the original publication, please, refer to the second part of this post.
Telehealth in community pharmacy: A new “place” for the appointment-based model given COVID-19 and the future of health care
Health care is shifting to a virtual model, and it is imperative that pharmacy shifts along with it — Insights from Canada
Canadian Pharmacists Journal
Sara Rezahi, BSc; Annalise Mathers, MPH, BSc ; Pooja Patel; Tiana Tilli, PharmD, RPh, ACPR; Lisa Dolovich, BScPhm, PharmD, MSc
May 24, 2021
Key messages
Summarized by Joaquim Cardoso MSc.
Health Revolution Institute
New Care Models Revolution Unit
May 2, 2022
What is the background in Canada
- In Canada, virtual care, including telephone or video visits, has been part of the delivery of pharmacy services for many years.
- The COVID-19 pandemic has accelerated the need for pharmacy to integrate virtual approaches into routine medication management services and programs to promote virtual continuity of care and improve patient health.
What was the impact of the pandemic
- The pandemic affects continuity of health care and medication management, as patients may be uncomfortable or unable to leave their homes due to risk of exposure.
- In Canada, it is estimated that two-thirds of primary care physician patient visits are now virtual, in comparison to an estimated 4% prior to the pandemic.
What is the evidence about Community Telepharmacy Services
- Research is now also beginning to emerge that presents guidelines for optimizing the use of virtual care for specific chronic conditions such as diabetes.
Systematic reviews show that pharmacy clinical services delivered by telephone have a positive impact on
- medication adherence,
- patient self-management of chronic disease and
- clinical disease outcomes such as controlled blood pressure and blood sugar in hypertension and diabetes, respectively.
- In rural areas, virtual care provision has effectively identified medication discrepancies and drug therapy problems through video chat.16
What is the appointment-based model (ABM)
- The appointment-based model (ABM) is an example of a proactive approach to pharmacy practice that synchronizes chronic prescription refills and couples it with regularly scheduled patient-pharmacist appointments to optimize medication management.
- The ABM is a common approach in the United States and is gaining traction in Canada.
- Medication synchronization involves aligning chronic medications to 1 refill date so that all medications can be picked up on 1 scheduled day.
- While the synchronized pickup date can vary, most ABM models in the literature use a 30-day interval, with some using a 90-day interval.
Key findings from the literature guided decision-making on how to adapt a conventional ABM model
Telephone-based virtual models not only align with patient preference but are also more accessible in Canada. According to Statistics Canada, 99% of adults aged 65 and above in Ontario have telephone access, while only 80% have Internet access. Only 30% have used the Internet for video streaming or calling.
Given the current evidence, recommendations for adaption of a conventional in-person ABM can be seen in Table 2.
Conclusion
Implementing ABM to meet the needs of high-risk patients amid the COVID-19 pandemic has the potential to serve as a precedent for future virtual ABMs well beyond the COVID-19 pandemic for patients who are unable to visit a pharmacy in person due to physical or health-related barriers.
Furthermore, providing medication synchronization, preappointment calls and appointments via telephone, coupled with medication delivery, can allow for increased access to pharmacy services and will ensure patients continue to have access to pharmacy services as the COVID-19 pandemic continues.
Final message
Health care is shifting to a virtual model, and it is imperative that pharmacy shifts along with it.
Telehealth in community pharmacy: A new “place” for the appointment-based model given COVID-19 and the future of health care
Health care is shifting to a virtual model, and it is imperative that pharmacy shifts along with it — Insights from Canada
Canadian Pharmacists Journal
Sara Rezahi, BSc; Annalise Mathers, MPH, BSc ; Pooja Patel; Tiana Tilli, PharmD, RPh, ACPR; Lisa Dolovich, BScPhm, PharmD, MSc
May 24, 2021
Coronavirus disease 2019 (COVID-19) is a global pandemic, with over 133 million cases and nearly 3 million deaths confirmed worldwide as of April 2021.1
As the virus is transmitted via droplet contact, global recommendations suggest that individuals practise physical distancing and avoid nonessential activities outside their home to prevent community-based transmission.2,3
Vulnerable populations, such as those over 60 years of age, those with chronic illnesses or individuals with multimorbidities who are on multiple and/or complex medication regimens, are at increased risk of contracting COVID-19 and experiencing subsequent complications and poor outcomes.4,5
While pharmacies remain open as essential services, many people using pharmacy services belong to these vulnerable populations and so are less likely to visit their pharmacy. 5
The pandemic affects continuity of health care and medication management, as patients may be uncomfortable or unable to leave their homes due to risk of exposure.
While pharmacies remain open as essential services, many people using pharmacy services belong to these vulnerable populations and so are less likely to visit their pharmacy
Telehealth is defined as a service that effectively connects individuals and their health care providers when an in-person interaction is not clinically necessary and facilitates health care provider-to-patient consultation.6
The most commonly used telehealth approaches are virtual visits, chat-based interactions, remote patient monitoring and technology-enabled modalities used for patient education or interprofessional communication.6
Virtual visits are synchronous, interactive encounters between a patient and a health care provider via video, telephone or live chat.6
Although virtual services within primary health care settings were available prior to the COVID-19 pandemic and many patients expressed interest in using these services, uptake of virtual care was slow to emerge in primary care until the pandemic; since this time, there has been a significant rise in the use of virtual care services.7
In Canada, it is estimated that two-thirds of primary care physician patient visits are now virtual, in comparison to an estimated 4% prior to the pandemic.8
Furthermore, a retrospective review of primary care physicians and patients who used virtual care services for 18 months showed that virtual visits could replace in-person visits and that 51% of patients had completed at least 1 virtual visit.9
Research is now also beginning to emerge that presents guidelines for optimizing the use of virtual care for specific chronic conditions such as diabetes.10
In Canada, it is estimated that two-thirds of primary care physician patient visits are now virtual, in comparison to an estimated 4% prior to the pandemic
Research is now also beginning to emerge that presents guidelines for optimizing the use of virtual care for specific chronic conditions such as diabetes
The COVID-19 pandemic provides a tremendous opportunity to expand the use of telehealth in pharmacy to reach people in their homes and ensure continuing delivery of care.
The COVID-19 pandemic provides a tremendous opportunity to expand the use of telehealth in pharmacy to reach people in their homes and ensure continuing delivery of care.
Virtual care, including telephone or video visits, has been part of the delivery of pharmacy services for many years.
Virtual care, including telephone or video visits, has been part of the delivery of pharmacy services for many years [In Canada]
- Systematic reviews show that pharmacy clinical services delivered by telephone have a positive impact on medication adherence, patient self-management of chronic disease and clinical disease outcomes such as controlled blood pressure and blood sugar in hypertension and diabetes, respectively.11–13
Systematic reviews show that pharmacy clinical services delivered by telephone have a positive impact on medication adherence, patient self-management of chronic disease and clinical disease outcomes such as controlled blood pressure and blood sugar in hypertension and diabetes, respectively
- In a study comparing the effect of home blood pressure telemonitoring (biweekly phone calls by the pharmacist that taper to every 2 months) combined with pharmacist management vs usual care, the number of patients with controlled blood pressure was significantly higher in the pharmacist telemonitoring group, with this group showing increased medication adherence. 14
- Another study demonstrated that patients receiving pharmacist telemonitoring had a significant reduction in their A1c compared to a retrospective chart review of characteristically similar patients who received usual care (2.07% vs 0.66% decrease in A1c).15
- Virtual care provision in rural areas has effectively identified medication discrepancies and drug therapy problems through video chat.16
The COVID-19 pandemic has accelerated the need for pharmacy to integrate virtual approaches into routine medication management services and programs to promote virtual continuity of care and improve patient health.
The COVID-19 pandemic has accelerated the need for pharmacy to integrate virtual approaches into routine medication management services and programs to promote virtual continuity of care and improve patient health.
The appointment-based model (ABM)
The appointment-based model (ABM) is an example of a proactive approach to pharmacy practice that synchronizes chronic prescription refills and couples it with regularly scheduled patient-pharmacist appointments to optimize medication management.17–21
The ABM is a common approach in the United States and is gaining traction in Canada.22
Medication synchronization involves aligning chronic medications to 1 refill date so that all medications can be picked up on 1 scheduled day.
While the synchronized pickup date can vary, most ABM models in the literature use a 30-day interval, with some using a 90-day interval.17–21
The appointment-based model (ABM) is an example of a proactive approach to pharmacy practice that synchronizes chronic prescription refills and couples it with regularly scheduled patient-pharmacist appointments to optimize medication management.
The ABM is a common approach in the United States and is gaining traction in Canada
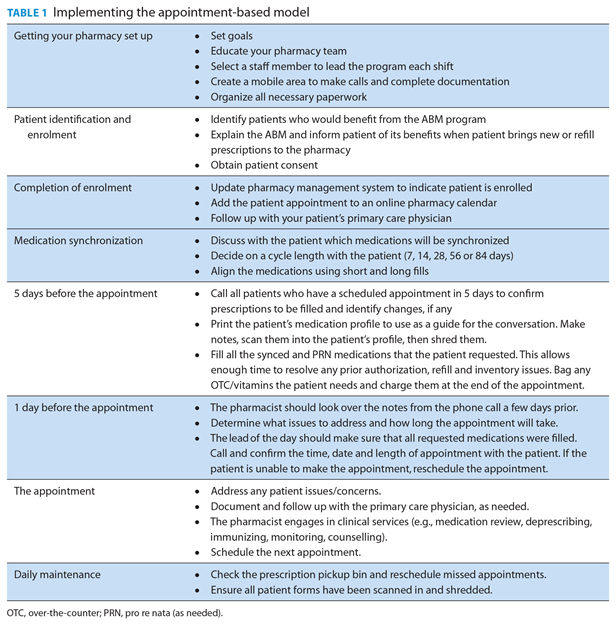
The general steps of the ABM are shown in Table 1. 23,24
Historically, the ABM interaction was conducted entirely in person and required the patient to be physically present for the pharmacist appointment and medication pickup.
The ABM approach has enormous potential to transition to virtual care.
Table 1 Implementing the appointment-based model
The ABM has multiple benefits for both patients and pharmacists.
Scheduled appointments provide an opportunity to plan for how to address medication-related issues (e.g., drug changes, side effect management) and optimize medication regimens (e.g., perform medication reviews, deprescribing).
It provides pharmacists with an opportunity to fulfill their role as health promoters to plan ahead and offer, where relevant, adult immunizations, lifestyle modification education, disease state monitoring and referrals to other health care professionals.
The ABM may also reduce medication nonadherence,25 since scheduled appointments to pick up medications decrease the number of trips to the pharmacy and increase number of refills.18–21
Having synchronized and scheduled refill dates creates a predictable workflow and increases pharmacy revenue and so the ABM offers increased, scheduled opportunities for pharmacists to conduct billable services and potentially increase pharmacy revenue.26,27
Recognizing the effectiveness of ABM, we considered the challenge of providing ABM in a model that incorporates telehealth approaches, given the new obstacles presented by COVID-19.
Key findings from the literature guided decision-making on how to adapt a conventional ABM model:
- A previous ABM study comparing in-person only, in-person initial meeting with telephone follow-up and telephone-only care all improved adherence and increased prescription refill numbers. 17
- Research focusing on telephone-based interventions for the ABM has shown improvement in medication adherence.18–21
- While there is no evidence for video-based ABMs within pharmacy, literature comparing video and telephone physician consultations shows that both video and telephone consults are of similar length and quality, but video has more technical difficulties.28
- Studies of older adults over 55 years of age suggest a preference for telephone rather than video consultations due to barriers including audiovisual difficulties (e.g., difficulty hearing or reading onscreen text), reduced cognitive ability (e.g., remembering passwords), Internet connection issues and low computer literacy (e.g., inexperience in computer use).29,30
- Telephone-based virtual models not only align with patient preference but are also more accessible in Canada.
According to Statistics Canada, 99% of adults aged 65 and above in Ontario have telephone access, while only 80% have Internet access.31,32
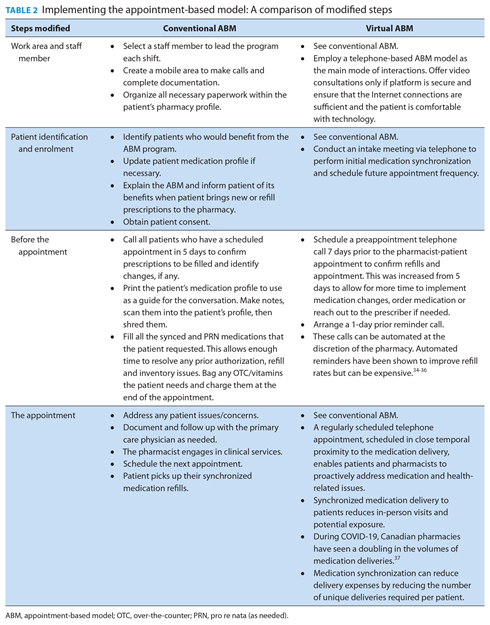
Only 30% have used the Internet for video streaming or calling.33 - Given the current evidence, our recommendations for adaption of a conventional in-person ABM can be seen in Table 2.
Given the current evidence, our recommendations for adaption of a conventional in-person ABM can be seen in Table 2.
Table 2 Implementing the appointment-based model: A comparison of modified steps
Conclusion
Implementing ABM to meet the needs of high-risk patients amid the COVID-19 pandemic has the potential to serve as a precedent for future virtual ABMs well beyond the COVID-19 pandemic for patients who are unable to visit a pharmacy in person due to physical or health-related barriers.
Implementing ABM to meet the needs of high-risk patients amid the COVID-19 pandemic has the potential to serve as a precedent for future virtual ABMs well beyond the COVID-19 pandemic
for patients who are unable to visit a pharmacy in person due to physical or health-related barriers.
Furthermore, providing medication synchronization, preappointment calls and appointments via telephone, coupled with medication delivery, can allow for increased access to pharmacy services and will ensure patients continue to have access to pharmacy services as the COVID-19 pandemic continues.
Health care is shifting to a virtual model, and it is imperative that pharmacy shifts along with it.
…providing medication synchronization, preappointment calls and appointments via telephone, coupled with medication delivery, can allow for increased access to pharmacy services and will ensure patients continue to have access to pharmacy services as the COVID-19 pandemic continues.
Health care is shifting to a virtual model, and it is imperative that pharmacy shifts along with it.
References and additional information
See the original publication
Originally published at https://journals.sagepub.com