Journal of the National Cancer Institute
Kathleen A Cronin 1, Susan Scott 1, Albert U Firth 2, Hyuna Sung 3, S Jane Henley 4, Recinda L Sherman 5, Rebecca L Siegel 3, Robert N Anderson 6, Betsy A Kohler 5, Vicki B Benard 4, Serban Negoita 1, Charles Wiggins 7, William G Cance 8, Ahmedin Jemal 3
2022 Oct 27
Editor of the portal:
Joaquim Cardoso MSc
health transformation portal
October 27, 2022
ABSTRACT
Background:
- The American Cancer Society, Centers for Disease Control and Prevention, National Cancer Institute, and North American Association of Central Cancer Registries collaborate to provide annual updates on cancer incidence and mortality and trends by cancer type, sex, age group, and racial/ethnic group in the United States.
- In this report, we also examine trends in stage-specific survival for melanoma of the skin (melanoma).
Methods:
- Incidence data for all cancers from 2001 through 2017 and survival data for melanoma cases diagnosed during 2001–2014 and followed up through 2016 were obtained from the Centers for Disease Control and Prevention- and National Cancer Institute-funded population-based cancer registry programs compiled by the North American Association of Central Cancer Registries.
- Data on cancer deaths from 2001 through 2018 were obtained from the National Center for Health Statistics’ National Vital Statistics System.
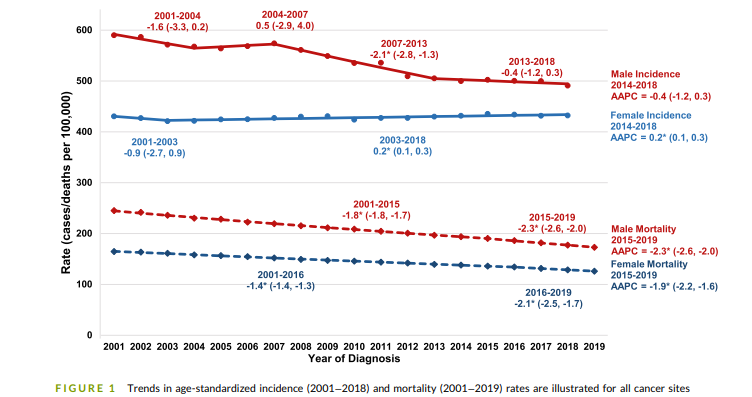
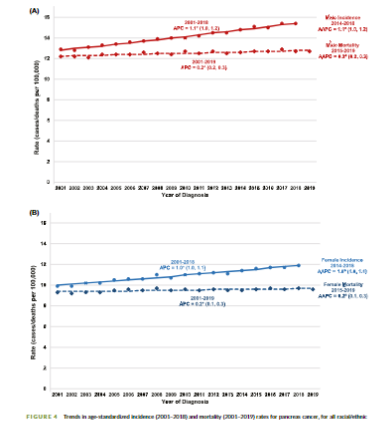
- Trends in age-standardized incidence and death rates and 2-year relative survival were estimated by joinpoint analysis, and trends in incidence and mortality were expressed as average annual percent change (AAPC) during the most recent 5 years (2013–2017 for incidence and 2014–2018 for mortality).
Results:
- Overall cancer incidence rates (per 100,000 population) for all ages during 2013–2017 were 487.4 among males and 422.4 among females.
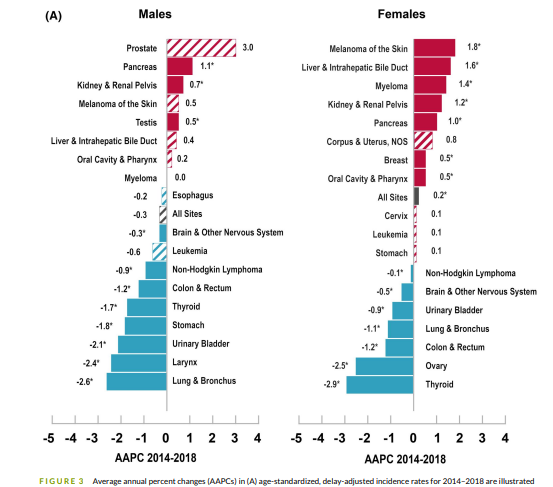
- During this period, incidence rates remained stable among males but slightly increased in females (AAPC = 0.2%; 95% confidence interval [CI] = 0.1% to 0.2%).
- Overall cancer death rates (per 100,000 population) during 2014–2018 were 185.5 among males and 133.5 among females.
- During this period, overall death rates decreased in both males (AAPC = -2.2%; 95% CI = -2.5% to — 1.9%) and females (AAPC = -1.7%; 95% CI = -2.1% to — 1.4%); ]
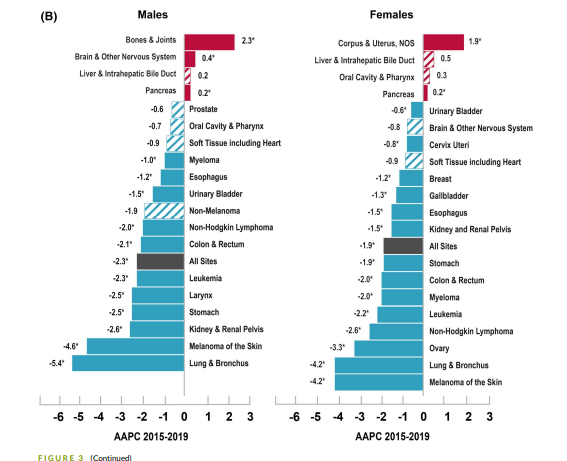
- death rates decreased for 11 of the 19 most common cancers among males and for 14 of the 20 most common cancers among females, but increased for 5 cancers in each sex.
- During 2014–2018, the declines in death rates accelerated for lung cancer and melanoma, …
- … slowed down for colorectal and female breast cancers, and leveled off for prostate cancer.
- Among children younger than age 15 years and adolescents and young adults aged 15–39 years, cancer death rates continued to decrease in contrast to the increasing incidence rates.
- Two-year relative survival for distant-stage skin melanoma was stable for those diagnosed during 2001–2009 but increased by 3.1% (95% CI = 2.8% to 3.5%) per year for those diagnosed during 2009–2014, with comparable trends among males and females.
Overall cancer incidence rates (per 100,000 population) for all ages during 2013–2017 were 487.4 among males and 422.4 among females.
Overall cancer death rates (per 100,000 population) during 2014–2018 were 185.5 among males and 133.5 among females.
Conclusions:
- Cancer death rates in the United States continue to decline overall and for many cancer types, with the decline accelerated for lung cancer and melanoma.
- For several other major cancers, however, death rates continue to increase or previous declines in rates have slowed or ceased.
- Moreover, overall incidence rates continue to increase among females, children, and adolescents and young adults.
- These findings inform efforts related to prevention, early detection, and treatment and for broad and equitable implementation of effective interventions, especially among under-resourced populations.
Infographic
Selected highlights:
- Progress in reducing overall cancer mortality has accelerated during the most recent period, largely driven by steep declines for lung cancer mortality.
- This report demonstrated that the incidence of pancreatic cancer increased among both males and females since 2001.
- Increases in pancreatic adenocarcinomas and neuroendocrine tumors are partially explained by a decrease in unknown/other subtypes, which may be related to better access to pathology laboratory report sources by cancer registries.
- There have also been improvements in multimodality therapy for pancreatic adenocarcinoma, which have shown a small survival benefit.22
- Lung cancer rates declined during the most recent period for both incidence and mortality, reflecting the continuous decline in smoking prevalence and improved treatments.
- Nontreatment factors that also may have contributed to the steep decline in lung cancer mortality during the most recent period include improved access to care, which followed the expansion of Medicaid to a broader group of low‐income adults beginning in 2014.34
- Contrary to the rapid decline in the risk of tobacco‐related cancers, progress has stagnated for some cancers associated with metabolic factors, such as excess body weight,40 physical inactivity,41,42 and diabetes.43–46
- A more than decade‐long rise in uterine cancer incidence rates leveled off during 2014–2018 among White females but continued in all other groups by >2% per year during that period.
- The steady increase in breast cancer incidence since 2004 continued by 0.5% per year, which coincides with the deceleration of declining death rates, potentially slowing the progress against breast cancer death achieved since the early 1990s.55,56
- Black females also experience the highest rates of aggressive breast cancer subtypes — estrogen‐receptor–negative or triple‐negative — of all populations.
- Thyroid cancer incidence continued to decrease for both males and females overall, and this is the first year that it also decreased for AYAs after years of increasing rates.
- Prostate cancer incidence rates stabilized during 2014–2018 after sharply declining during 2007–2014.
- The ICD‐O‐3 revision in 2010 affected mostly hematopoietic malignancies and thus had a larger impact on incidence rates of childhood cancer.
Conclusions [excerpt]
- Cancer death rates continued to decline overall, for children, and for AYAs, and treatment advances have led to accelerated declines for several sites, such as lung and melanoma.
- Cancer incidence stabilized for males and children and increased for females and AYAs, reflecting changes in cancer risk factors, screening test use, and diagnostic practices.
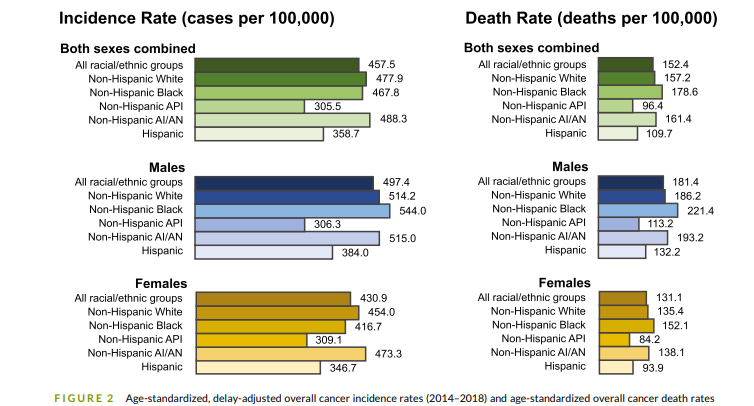
- The continuous, large racial/ethnic disparities in cancer incidence and mortality underscore the need to fully understand contributing factors for addressing the inequalities.
- Population‐based incidence and mortality data inform prevention, early detection, and treatment efforts to help reduce the cancer burden in the United States.DISCUSSION [excerpt]
ORIGINAL PUBLICATION (excerpt)

Introduction
The Centers for Disease Control and Prevention (CDC), the American Cancer Society, the National Cancer Institute (NCI), and the North American Association of Central Cancer Registries (NAACCR) have collaborated annually since 1998 to provide updated information about cancer occurrence and trends by cancer type, sex, age group, and racial/ethnic group in the United States.
Part 1 of this report focuses on national cancer statistics and highlights incidence, mortality, and survival trends in pancreatic cancer — for which the prognosis remains poor, with few of the advances in screening or treatment that are seen in other cancer sites.
The pancreas is one of the few cancer sites for which incidence and death rates have been increasing in recent years.
Statistics are presented overall and by subtype. Part 2 focuses on the impact of coronavirus disease 2019 (COVID‐19) on cancer diagnosis in 2020.
The pancreas is one of the few cancer sites for which incidence and death rates have been increasing in recent years.
Other sections:
See the original publication
Discussion [excerpt]
Progress in reducing overall cancer mortality has accelerated during the most recent period, largely driven by steep declines for lung cancer mortality.
Liver cancer mortality has stabilized since 2013 among males and since 2014 among females after years of increasing rates. Mortality declines have slowed for colorectal and female breast cancer and have ceased for prostate cancer after periods of accelerated declines. Incidence trends largely reflect changes in risk factors in the population, screening behaviors, and diagnostic practices; whereas changes in risk factors, screening, and treatment all affect mortality trends.16 Unlike mortality, incidence continues to increase among females and remains stable among males. The most rapid increases in incidence were seen for pancreas, kidney, and testis cancers among males and for melanoma, liver cancer, and myeloma among females. The AYA age group experienced increases in overall cancer incidence and the slowest mortality decline. The incidence trend for childhood cancers overall stabilized between 2015 and 2019, although it continued to increase in racial/ethnic groups. Because the number of childhood cancers is small and there is more variance in the rate estimates, it is harder to find statistically significant joinpoints than in other groups. Although there is some evidence that incidence may be leveling off for specific racial/ethnic groups, the joinpoint model has not found a significant joinpoint signaling a change in trend within racial/ethnic groups.
This report demonstrated that the incidence of pancreatic cancer increased among both males and females since 2001.
Although pancreatic cancer accounts for only 3% of new cancer diagnoses, it accounts for 8% of cancer deaths and is now the fourth leading cause of cancer deaths in the United States for both males and females.17 Approximately 10%–15% of pancreatic cancers may have a familial component.18 Although no screening modality has demonstrated efficacy in reducing pancreatic cancer mortality in clinical trials, people with known genetic mutation syndromes may benefit from screening with endoscopic ultrasound or magnetic resonance imaging.18
Increases in pancreatic adenocarcinomas and neuroendocrine tumors are partially explained by a decrease in unknown/other subtypes, which may be related to better access to pathology laboratory report sources by cancer registries.
Pancreatic adenocarcinoma represented approximately 80% of pancreatic cancer cases diagnosed. There are very few symptoms until the disease has progressed, and pancreatic adenocarcinomas typically acquire invasive and metastatic capacity early in their course, explaining why greater than 85% of patients have regional or distant spread at the time of diagnosis.19 Survival for pancreatic adenocarcinoma remains low, with a predicted 1‐year survival rate of 38% and a 5‐year survival rate of 10% for cases diagnosed in 2018. Pancreatic neuroendocrine tumors generally are slower growing, and approximately 50% are localized at the time of diagnosis. The current results indicate that neuroendocrine pancreatic cancers had higher survival than pancreatic adenocarcinomas, which tend to be diagnosed at a late stage, when surgical resection is not recommended.19 Neuroendocrine pancreatic cancers also had higher survival than unspecified/ other types, which were mostly diagnosed among older adults. Relative survival increased from 2001 to 2018 for both adenocarcinomas and neuroendocrine tumors, but this good news is tempered by the overall increase in pancreatic cancer incidence during this same period. This increase in incidence is generally attributed to the increase in obesity prevalence, which has offset declines in smoking prevalence.20 Improvements in medical imaging techniques and increased use of imaging also may have contributed to improved detection and diagnosis of pancreatic cancer.21
There have also been improvements in multimodality therapy for pancreatic adenocarcinoma, which have shown a small survival benefit.22
Emerging data about the efficacy of neoadjuvant chemoradiotherapy followed by surgery and chemotherapy have shown improved 5‐year overall survival compared with surgery followed by chemotherapy.23 Nonetheless, progress in treating pancreatic adenocarcinoma has been incremental at best, as demonstrated by the modest gains in survival over time. In contrast, pancreatic neuroendocrine tumors have shown sustained increases in 5‐year survival since 2000. These results are based on advances in multimodality therapies, including surgery, ablation/embolization, and a variety of chemotherapeutic approaches.24,25
Lung cancer rates declined during the most recent period for both incidence and mortality, reflecting the continuous decline in smoking prevalence and improved treatments.
Adult smoking prevalence declined from >40% during the early 1960s to 13% in 2019.26,27 The decline in lung cancer death rates during the most recent period, however, was more than double the decline for incidence, in part reflecting recent advances in targeted and immune therapies for non‐small cell lung cancer (NSCLC).28 The US Food and Drug Administration approved the first targeted therapy for NSCLC in 2003,29 followed by the approval of several other targeted therapies, recommendations for genetic mutation testing of all individuals with nonsquamous NSCLC for relevant genetic targets in 2012, and approval of several immune checkpoint inhibitors in 2015–2016.30 Other treatment advances for lung cancer include minimally invasive surgery31; stereotactic body radiation therapy for inoperable, early stage cancer32; adjuvant therapy; and supportive and palliative care.33 Treatment advances that increase survival may delay or prevent cancer deaths; data on additional years of mortality rates will provide insight into the longer term benefits of these treatments.
Nontreatment factors that also may have contributed to the steep decline in lung cancer mortality during the most recent period include improved access to care, which followed the expansion of Medicaid to a broader group of low‐income adults beginning in 2014.34
Lung cancer screening use slightly increased from 4% in 2014 to 6.5% in 2020 nationwide,35,36 with the rate in 2020 as high as 18%–20% in states with comprehensive screening programs, such as Kentucky and Massachusetts.36 Also, between 2013 and 2018, the proportion of lung cancer cases diagnosed at localized stage increased from 20% to 28%, perhaps in part because of increased screening.17 Although there has been considerable progress in reducing mortality from lung cancer, it remains the leading cause of cancer death in every racial/ethnic group and greater than 30 million adults currently smoke cigarettes.37 The broad and equitable application of proven tobacco control policies, such as raising excise tax on tobacco products, banning flavored tobacco products, and enacting and implementing smoke‐free laws to promote cessation and discourage initiation, may help to further reduce smoking prevalence.38,39
Contrary to the rapid decline in the risk of tobacco‐related cancers, progress has stagnated for some cancers associated with metabolic factors, such as excess body weight,40 physical inactivity,41,42 and diabetes.43–46
Increasing incidence trends continued for cancers of the female breast, colorectum (among AYAs), and pancreas, and trends have decelerated or stabilized since the mid‐ 2010s for myeloma and cancers of the uterus and kidney. A parallel rise in death rates occurred only for colorectal (among AYAs), pancreatic, and uterine cancers; however, the earlier declines in death rates slowed for breast cancer. The staggering rise in obesity,47 diabetes,48 and total sitting time49 continues among adults and youth, highlighting opportunities to halt these unfavorable trends.
A more than decade‐long rise in uterine cancer incidence rates leveled off during 2014–2018 among White females but continued in all other groups by >2% per year during that period.
The stabilization in the incidence rates among White females appeared to be driven by more common and less aggressive subtypes (i.e., endometrioid subtype), whereas nonendometrioid subtypes continued to rise rapidly in all groups.50 Well established risk factors for uterine cancer include excess body weight, diabetes, physical inactivity, nulliparity (no births), fewer births, and earlier age at menarche,51 which may have contributed to the increasing incidence trends; however, reasons for the more rapid rise of nonendometrioid subtypes remain unknown.52 Uterine cancer death rates continued to increase in all groups, although there are indications that they have stabilized since 2016.17 Despite the similar incidence of uterine cancer among Black and White females, uterine cancer death rates are twice as high in Black females, and this disparity is increasing.53 Nonendometrioid subtypes account for 35% of all uterine cancers among Black females, which is considerably higher than the 16% among White females,50 likely contributing to the disproportionately higher death rate among Black females — although Black females had worse survival across all stages and subtypes.50,54 In addition to multilevel interventions to help females achieve and maintain a healthy body weight and physical activity level, identifying the factors associated with increasing trends in aggressive uterine cancers, the higher prevalence of aggressive disease among Black females, and the racial disparity in survival may help further inform public health programs aimed at reducing this burden.52
The steady increase in breast cancer incidence since 2004 continued by 0.5% per year, which coincides with the deceleration of declining death rates, potentially slowing the progress against breast cancer death achieved since the early 1990s.55,56
The increase in breast cancer incidence may reflect continuing decreases in parity rates57,58 and advancing age at first birth58 as well as increases in obesity47 and alcohol consumption.59 The racial gap in the breast cancer death rate persists; the death rate during 2015–2019 was 28.0 per 100,000 among Black females, which was 40% higher than the 19.9 per 100,000 among White females (who ranked second) and 140% higher than the 11.7 among API females (who have the lowest rates). The highest breast cancer death rates seen among Black females are partially caused by the significant barriers to providing access to timely, high‐quality medical care, which require addressing multiple dimensions of disparity across the continuum of cancer care.60–68
Black females also experience the highest rates of aggressive breast cancer subtypes — estrogen‐receptor–negative or triple‐negative — of all populations.
Ascribing underlying reasons for such high rates among Black females is complex, although premenopausal abdominal adiposity,69,70 earlier age at menarche,71–73 higher parity without breastfeeding,74 and multiple genetic variants75–78 have been identified as risk factors for estrogen receptor–negative breast cancer. Importantly, residential segregation, neighborhood disadvantage, and lower neighborhood socioeconomic status (SES) have been associated with increased risk for estrogen receptor–negative breast cancer among Black females,79–83 even after controlling for multiple behavioral and lifestyle factors.79 Findings from these studies point to structural factors as significant elements contributing to racial disparity in breast cancer subtypes. Addressing structural racism may contribute to health equity in breast cancer mortality.84
Thyroid cancer incidence continued to decrease for both males and females overall, and this is the first year that it also decreased for AYAs after years of increasing rates.
However, rates increased for AI/ AN males and females. The declines are thought to reflect changes in diagnosis practices beginning in 2009.85 Prior studies have shown increases in both incidence and death rates of distant‐stage thyroid cancer from the 1990s to the early 2010s,86,87 suggesting that there is a genuine increase in the risk of thyroid cancer that likely reflects changes in the prevalence of underlying risk factors, such as excess body weight.88
Prostate cancer incidence rates stabilized during 2014–2018 after sharply declining during 2007–2014.
These trends coincided with changes in the use of prostate‐specific antigen (PSA) testing, which followed the US Preventive Services Task Force recommendations against PSA‐based prostate cancer screening for men aged 75 years or older in 200889 and for all men in 2012.90 Routine PSA testing declined from 2007 to 2013 and remained unchanged from 2013 to 2018.91 Prostate cancer incidence rates, however, continued to increase for regional‐stage and distant‐stage disease,92 which may have contributed to the recent stabilization of prostate cancer mortality after years of a declining trend.92 Other factors that also may have contributed to the stabilized mortality include the rise in obesity prevalence,93 which is associated with advanced‐stage or aggressive forms of prostate cancer.94,95 In 2018, the US Preventive Services Task Force recommended informed decision making for PSA‐based screening in men aged 55–69 years,96 reversing its prior recommendations. Long‐term monitoring of prostate cancer incidence and mortality may help assess the effects of the 2018 recommendation.
Last year’s report focused on increased survival and rapid declines in mortality for melanoma after the introduction of new treatments, including targeted treatments and immune checkpoint inhibitors.97
After a period during which melanoma mortality was declining sharply and incidence was increasing, incidence rates among males have stabilized since 2016, and mortality among males has stabilized since 2017. Among females, incidence has increased for melanoma faster than for any other cancer site, whereas melanoma mortality has decreased. The AYA age group has experienced decreasing melanoma incidence rates since 2001, suggesting that public health efforts, such as limiting tanning bed use, are having an effect on this age group.98
Death rates for cancers of the oral cavity and pharynx increased among White males and females but not among other racial/ethnic groups.
This group of cancers is anatomically and histologically diverse, arising from exposure to different causal factors, such as alcohol use, tobacco use, and human papillomavirus infection.99 Recent studies suggest that increases in oral cavity and pharynx cancer are caused primarily by increases in human papillomavirus‐ associated types.100,101
In previous annual reports to the nation, incidence rates for API and AI/AN persons included Hispanic and non‐Hispanic ethnicities, whereas this year’s report is based on non‐Hispanic API and non‐ Hispanic AI/AN ethnicities.
This change in reporting resulted in a small increase in incidence rates among non‐Hispanic API persons compared with all API persons and a larger increase for non‐Hispanic AI/AN persons compared with all AI/AN persons (Table S2).102,103 Population estimates are based on race and ethnicity reported by respondents or their proxies in the US census; however, methods are used to correct for missing responses. For example, individuals who self‐report as Hispanic may not see themselves captured in the race variable and may not answer the race question in the census.104 In the 2010 census, those reporting Hispanic ethnicity were more likely to have missing race information than the total population.105 When race is missing or is categorized as some other race, it is assigned by the US Bureau of the Census using other available information.106 Changes in methodology with the 2010 census resulted in the US Bureau of the Census assigning more people with Hispanic ethnicity and missing or some other race to the AI/AN category than in previous years, artificially inflating the Hispanic AI/AN denominator and thus yielding lower cancer rates for all AI/AN persons.102,107 In addition, there are issues of misclassification of race and ethnicity in medical records and death certificates, causing underestimation of cancer incidence and death rates, with the greatest impact on AI/AN and Hispanic populations.102,103,108–110 Reporting cancer rates among non‐Hispanic AI/AN persons residing in PRCDA counties is considered to improve the accuracy of cancer burden estimates among AI/ AN people.110 In the current report, compared with other racial/ ethnic groups, AI/AN persons residing in PRCDA counties had the highest cancer incidence rate overall, the second highest among males, and the highest among females
In previous reports, the definition of malignant cases included when calculating rates and trends was restricted to those that would have been reportable to registries from 1975 and forward.
For this report, a change was made to include reportable cases based on the definitions in place during the year of diagnosis.
This includes changes that occurred with the release of the ICD‐O‐3,2 which went into effect in 2001, and the release of ICD‐O‐3 Revision 1, which went into effect in 2010.3,5 For example, in 2010, new morphology codes meant that more hematopoietic tumors were considered malignant. As a result of these changes, age‐adjusted incidence for all cancer sites combined in 2001 increased about 1% compared with the prior definition, and a smaller impact was seen in 2010 for age‐adjusted incidence rates compared with the prior definition.6
The ICD‐O‐3 revision in 2010 affected mostly hematopoietic malignancies and thus had a larger impact on incidence rates of childhood cancer.
The incidence rate for childhood cancers in last year’s report gave an incidence rate of 16.8 per 100,000 for diagnosis years 2013–2017, while in this year’s report the incidence rate for childhood cancers is 17.8 per 100,000 for diagnosis years 2014– 2018. The rate would have been 17.0 per 100,000 if the old definition had been used. Comparable differences for childhood lymphoma were not observed because most new morphology codes reportable since 2010 were Langerhans cell histiocytosis, which were classified as miscellaneous in the SEER site categorization.
CONCLUSIONS
- Cancer death rates continued to decline overall, for children, and for AYAs, and treatment advances have led to accelerated declines for several sites, such as lung and melanoma.
- Cancer incidence stabilized for males and children and increased for females and AYAs, reflecting changes in cancer risk factors, screening test use, and diagnostic practices.
- The continuous, large racial/ethnic disparities in cancer incidence and mortality underscore the need to fully understand contributing factors for addressing the inequalities.
- Population‐based incidence and mortality data inform prevention, early detection, and treatment efforts to help reduce the cancer burden in the United States.
About the authors & affiliations:
Kathleen A Cronin 1, Susan Scott 1, Albert U Firth 2, Hyuna Sung 3, S Jane Henley 4, Recinda L Sherman 5, Rebecca L Siegel 3, Robert N Anderson 6, Betsy A Kohler 5, Vicki B Benard 4, Serban Negoita 1, Charles Wiggins 7, William G Cance 8, Ahmedin Jemal 3
Affiliations
- 1Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Maryland, USA.
- 2Information Management Services, Inc, Rockville, Maryland, USA.
- 3Department of Surveillance and Health Equity Science, American Cancer Society, Atlanta, Georgia, USA.
- 4Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
- 5North American Association of Central Cancer Registries, Springfield, Illinois, USA.
- 6National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, Maryland, USA.
- 7New Mexico Tumor Registry, University of New Mexico Comprehensive Cancer Center, Albuquerque, New Mexico, USA.
- 8American Cancer Society, Atlanta, Georgia, USA.
References
See the original publication
Originally published at https://pubmed.ncbi.nlm.nih.gov on October 27, 2021.












