This is a republication of an excerpt of the paper “Digital transformation of healthcare sector — What is impeding adoption and continued usage of technology-driven innovations by end-users?”, with the title above. The post is preceded by an Executive Summary, by the Editor of the Portal.
health transformation institute (HTI)
research institute & knowledge portal
Joaquim Cardoso MSc*
Founder, and Chief Researcher & Editor
December 2, 2022
MSc* from London Business School — MIT Sloan Masters Program
Senior Advisor for Health Transformation & Digital Health
Executive Summary
What is the problem?
- The digital transformation of businesses is no longer debatable, and the effects are visible in all sectors.
- What is arguable, however, is why the transformation has not been seamless-particularly given the multiple benefits of digitalization.
What is the scope of the paper?
- We seek to address this question for the healthcare sector, where various reports have acknowledged end-users’ resistance to the adoption and continued usage of technology-driven innovations ( e-health innovations).
- These accounts, though, are largely anecdotal, and the volume of academic research in the area has remained rather confined.
What is the methodology?
- To address this paucity of insights, particularly after the onset of the pandemic, which has brought the healthcare sector to the fore, we conducted a qualitative study among healthcare providers (doctors, nurses, and other clinical staff).
- We conducted our study in the United Kingdom and analyzed the data using the classic approach of manual content analysis.
What is the objective?
- The key objective of our study was to identify the perceived barriers and other inhibiting factors that impede individuals’ adoption and continued usage of e-health innovations.
What are the findings?
- Through these efforts, we identified barriers from the perspectives of healthcare providers:
task-related, patient-care, and system barriers, healthcare organizations (threat perception and infrastructural barriers),
- patients (usability and resource barriers), and
- end-users in general (self-efficacy, tradition, and image barriers).
What are the recommendations?
- Our study makes a noteworthy theoretical contribution by proposing a conceptual framework for resistance to e-health innovations that is grounded in innovation resistance theory (IRT).
- We also make some useful suggestions for practice that have the potential to accelerate the diffusion of e-health innovations.
Infographic
Key points
Healthcare provider barriers
Based on the content analysis, healthcare providers experience barriers that can be categorized into three sub-themes:
- task-related barriers,
- patient-care barriers, and
- system barriers.
Organizational barriers
Our content analysis led us to categorize the organizational barriers in the healthcare space into two sub-themes:
- threat perception and
- infrastructural barriers.
Patient barriers
Through our content analysis, we identified two key sub-barriers that healthcare providers perceived among patients:
- usability and
- resource barriers.
End-user barriers
Here, we have categorized end-user barriers to e-health innovations into three sub-themes:
- self-efficacy barriers,
- tradition barriers, and
- image barriers.
Individual differences in perceived barriers
- The literature has extensively debated the effects of differences in respondents’ socio-demographic profile on their attitudes toward technology, including their resistance to various digital innovations
- In the specific context of resistance to e-health innovations, past studies have noted individual differences based on various socio-demographic aspects.
- Our review of the responses we received did not reveal any gender-based variations in the respondents’ perceptions of various barriers.
- Similarly, we noticed individual differences in perceived barriers across various specialties, particularly mental health and dermatology.
What are the theoretical implications of the study?
Our study offers three key theoretical contributions:
- First, ours is one of few attempts to examine the barriers to the use of e-health innovations for healthcare delivery and administration in the post-COVID-19 era.
- Second, regarding sources of individual differences in providers’ perceived barriers, our study makes interesting contributions that may have implications for research not only on e-health innovations but in other digital contexts as well.
- Finally, our study offers a concrete contribution by formulating a conceptual framework grounded in the seminal IRT (Ram & Sheth, 1989).
What are the practical implications of the study?
Three key practical implications emerge from our study:
- First, our findings indicate that despite the ongoing digital transformation of business and personal life, the perceived barriers impeding the adoption and continued use of e-health innovations are quite basic and related to issues in the day-to-day use of such innovations for consultation, diagnosis, and healthcare administration.
the perceived barriers impeding the adoption and continued use of e-health innovations are quite basic and related to issues in the day-to-day use of such innovations for consultation, diagnosis, and healthcare administration.
- Second, we recommend that regulators be mindful of their role in mitigating the barriers that hinder the diffusion of e-health innovations.
- Finally, because digital transformation is here to stay and facilitates cost-effective and time-efficient care, healthcare organizations (large hospitals in particular) that are associated with medical colleges and nursing schools should make the necessary curricular changes to ensure that all pre-service doctors, nurses, and other clinical staff receive mandatory training in technology use in the healthcare sector.
Second, we recommend that regulators be mindful of their role in mitigating the barriers that hinder the diffusion of e-health innovations.
Finally, because digital transformation is here to stay and facilitates cost-effective and time-efficient care, healthcare organizations (large hospitals in particular) that are associated with medical colleges and nursing schools should make the necessary curricular changes to ensure that all pre-service doctors, nurses, and other clinical staff receive mandatory training in technology use in the healthcare sector.
ORIGINAL PUBLICATION (excerpt)

Digital transformation of healthcare sector — What is impeding adoption and continued usage of technology-driven innovations by end-users?
Shilpa Iyanna a,b , Puneet Kaur c,d,* , Peter Ractham e , Shalini Talwarf , A.K.M. Najmul Islam g
23 August 2022
1. Introduction
The past several decades have brought technological advances that have impacted individuals’ work and personal lives in myriad ways.
We are living in an era of unprecedented digital transformation, which, in its simplest form, involves leveraging technology to ensure a multifold increase in firms’ reach and performance (Del Giudice et al., 2021, Westerman et al., 2014).
The evolution of technology — whether in the form of Industry 4.0′s digital transformation of the business world through technologies such as artificial intelligence (AI), 3D printing, and cloud computing (Adebanjo et al., 2021, Kapletia et al., 2019) or in the consumer space via technologies such as smartwatches, smart homes, and online food delivery (Pal et al., 2019, Talwar et al., 2021) — has revolutionized the ways individuals live, communicate, and work.
The evolution of technology — whether in the form of Industry 4.0′s digital transformation of the business world through technologies such as artificial intelligence (AI), 3D printing, and cloud computing , …
… or in the consumer space via technologies such as smartwatches, smart homes, and online food delivery — has revolutionized the ways individuals live, communicate, and work.
Notably, these rapidly emerging information and communication technologies (ICTs)/digital technologies have, over the past two decades, enhanced firms’ ability to navigate the turbulent business milieu and offered them multiple growth opportunities (Elia et al., 2021, Kaur et al., 2020; Popkova et al., 2021; Scuotto, Santoro, Bresciani, & Del Giudice, 2017).
Similarly, the Internet of Things (IoT) has significantly influenced the ways in which organizations create value in their day-to-day operations (Bresciani, Ferraris, & Del Giudice, 2018).
…these rapidly emerging information and communication technologies (ICTs)/digital technologies have, over the past two decades, enhanced firms’ ability to navigate the turbulent business milieu and offered them multiple growth opportunities
Similarly, the Internet of Things (IoT) has significantly influenced the ways in which organizations create value in their day-to-day operations
At the same time, big data has come to represent a key strategic advantage for firms and knowledge creation enablers (Bertello et al., 2021, Bresciani et al., 2021).
Undoubtedly, this favorable environment for business growth has expanded lucrative job opportunities, which have contributed to improve the quality of individuals’ lives in all spheres.
At the same time, big data has come to represent a key strategic advantage for firms and knowledge creation enablers
This tidal wave of technological innovations, which has become a veritable tsunami during the past few years, has, in particular, influenced the healthcare sector.
Multiple digitally-driven technological transformations have occurred not only in diagnostics and equipment but also in healthcare administration, management, and delivery.
This tidal wave of technological innovations, which has become a veritable tsunami during the past few years, has, in particular, influenced the healthcare sector.
The scholarly literature has noted the impact of some emergent technology-driven healthcare innovations, such as the health cloud, mobile health (m-health), telemedicine services, computerized physician order entry (CPOE), electronic medical record (EMR) systems, information technology-based assistive services, and clinical decision support systems (CDSSs; e.g., Heath & Porter, 2019; Zobair, Sanzogni, & Sandhu, 2020).
The scholarly literature has noted the impact of some emergent technology-driven healthcare innovations, such as:
… the health cloud, mobile health (m-health), telemedicine services, computerized physician order entry (CPOE), electronic medical record (EMR) systems, information technology-based assistive services, and clinical decision support systems
These innovations have substantially improved the diagnosis and administration of medical care (Choi, Park, Choi, & Yang, 2019).
However, they have not diffused as anticipated based on their multiple benefits.
These innovations have substantially improved the diagnosis and administration of medical care (Choi, Park, Choi, & Yang, 2019).
However, they have not diffused as anticipated based on their multiple benefits.
While acknowledging these benefits, including a reduction in diagnostic errors and improvements in healthcare delivery (PITAC, 2004),
… scholars have noted resistance from various stakeholders to various innovations and advances in digital healthcare technologies …
… — popularly called healthcare information technologies (HIT) or electronic health (e-health; e.g., Kelly et al., 2017, Sarradon-Eck et al., 2021).
… scholars have noted resistance from various stakeholders to various innovations and advances in digital healthcare technologies …
This resistance in the healthcare sector is not an anomaly; in fact, digital innovations in most sectors have faced both overt and covert user resistance to their acceptance and adoption (Talwar, Talwar, Kaur, Singh, & Dhir, 2021).
Underlying this resistance is the fact that digital transformation entails many threats, which past studies have documented in various contexts (Bresciani, Ciampi, Meli, & Ferraris, 2021).
In the healthcare sector specifically, Bhattacherjee and Hikmet (2007) revealed resistance to change as a factor that negatively impacted physicians’ intentions to use HIT.
Because these authors conducted their study during the initial phase of HIT innovations, it is reasonable to assume that such resistance has since decreased.
Nevertheless, the resistance persists, as scholars have recently observed in the context of mobile health (mHealth) apps (Sarradon-Eck et al., 2021) and electronic medical records (Ilie & Turel, 2020), among others.
This resistance in the healthcare sector is not an anomaly; in fact, digital innovations in most sectors have faced both overt and covert user resistance to their acceptance and adoption
Nevertheless, the resistance persists [to the use of HIT], as scholars have recently observed in the context of mobile health (mHealth) apps and electronic medical records , among others.
While researchers were attempting to decode the continued stakeholder resistance to e-health innovations, the COVID-19 pandemic emerged in 2020, adding another dimension to the puzzle.
Indeed, the outbreak of the pandemic and the subsequent restrictions on movement not only produced multiple economic and non-economic challenges across the globe (Laato et al., 2020, Talwar et al., 2021) but also exerted extremely pervasive effects on individuals and their behaviors (Ghobadian et al., 2022, Mohammed and Ferraris, 2021), including their approach toward digital transformation.
This is particularly true in the healthcare sector, where the pandemic posed the unprecedented challenge of safely caring for patients who suffered from diseases other than COVID-19 infections.
This task became even more difficult when elderly individuals and others with co-morbidities, such as diabetes, were found to be more susceptible to COVID-19 complications (Smith et al., 2020).
In this context, digital innovations/e-health solutions, such as telehealth (Monaghesh & Hajizadeh, 2020), presented feasible ways to offer medical care from a distance (Wax and Christian, 2020).
While researchers were attempting to decode the continued stakeholder resistance to e-health innovations, the COVID-19 pandemic emerged in 2020, adding another dimension to the puzzle.
In this context, digital innovations/e-health solutions, such as telehealth, presented feasible ways to offer medical care from a distance
The initial phase of the pandemic thus witnessed an increase in the use of e-health solutions and digital technologies for healthcare delivery and management.
Many observers interpreted this increase in use as a sign that resistance towards e-health innovations, which was quite prominent before the onset of the pandemic, was declining.
However, the increasing use of e-health solutions has not persisted as the spread of COVID-19 infections has slowed.
Indeed, recent studies have noted the reemergence of wariness among doctors towards the use of digital technologies, with many reverting to more physical interactions for healthcare delivery following the initial phase of the pandemic (Mehrotra et al., 2020, Webster, 2020).
The initial phase of the pandemic thus witnessed an increase in the use of e-health solutions and digital technologies for healthcare delivery and management.
Many observers interpreted this increase in use as a sign that resistance towards e-health innovations, which was quite prominent before the onset of the pandemic, was declining.
However, the increasing use of e-health solutions has not persisted as the spread of COVID-19 infections has slowed.
This behavior highlights the continued resistance toward e-health innovations, which makes it imperative, yet again, for researchers to identify the reasons that individuals — whether patients, doctors, or other clinical staff members — continue to resist the digital transformation of healthcare delivery and management despite the multiple benefits associated with it.
This behavior highlights the continued resistance toward e-health innovations, which makes it imperative, yet again, for researchers to identify the reasons that individuals — whether patients, doctors, or other clinical staff members — continue to resist the digital transformation of healthcare delivery and management despite the multiple benefits associated with it.
Recognizing this need, the present study examines the factors that contribute to the renewed resistance from multiple organizational stakeholders, …
… such as doctors, nurses, and other clinical staff, to e-health innovations that had proved quite useful at the peak of the pandemic, as observed by various reports and studies (Wax and Christian, 2020; Monaghesh & Hajizadeh, 2020).
Recognizing this need, the present study examines the factors that contribute to the renewed resistance from multiple organizational stakeholders, …
Specifically, we aim to address the following research questions (RQs):
- RQ1. What are the perceived sources of resistance among end-users and healthcare organizations to the seamless adoption and continued usage of various e-health innovations?
- RQ2. Do individual differences, such as socio-demographic profile, healthcare specialty, level in the professional hierarchy (doctor, nurse, and so on), and number of years of experience, affect the perceived sources of resistance to healthcare providers’ adoption and continued use of various e-health innovations?
Specifically, we aim to address the following research questions (RQs):
RQ1. What are the perceived sources of resistance among end-users and healthcare organizations to the seamless adoption and continued usage of various e-health innovations?
RQ2. Do individual differences, such as socio-demographic profile, healthcare specialty, level in the professional hierarchy (doctor, nurse, and so on), and number of years of experience, affect the perceived sources of resistance to healthcare providers’ adoption and continued use of various e-health innovations?
We collected data from the target segment in the form of open-ended essays.
The qualitative study, conducted on Prolific Academic, produced 59 responses, which we subjected to a content analysis to identify the key themes.
The key outcomes of this qualitative inquiry include
(a) identifying the inhibiting factors exacerbating end-user resistance towards that e-health innovations that can transform the delivery and administration of healthcare services and
(b) generating insights regarding the effects of individual differences (age, gender, number of years of experience in the healthcare sector, specialty/department, e.g., oncology, urology, and level in the professional hierarchy) on healthcare providers’ resistance to the adoption and continued usage of e-health innovations.

2. Background literature
The extant literature has confirmed the resistance of doctors/physicians and clinical staff towards the acceptance and adoption of various e-health/HIT innovations, …
… such as telemedicine, electronic health records, and RFID (Radio Frequency Identification), to deliver and manage healthcare operations (e.g., Aboelmaged and Hashem, 2018, Dubin et al., 2020, Heath and Porter, 2019).
The extant literature has confirmed the resistance of doctors/physicians and clinical staff towards the acceptance and adoption of various e-health/HIT innovations, …
Broadly speaking, the prior literature has, in the past few years, identified a host of organizational, technological, professional, and patient-related inhibiting factors.
For instance, the existing scholarship (e.g., Kelly et al., 2017, Litvin et al., 2012) has linked resistance among doctors and clinical staff to these stakeholders’ concerns regarding changes in workflow and organizational issues.
Past studies have also linked these workflow concerns to the additional time these professionals may be required to commit to integrate these innovations into their practice, which, in turn, results in productivity issues (McAlearney et al., 2013, Yu et al., 2013).
Interestingly, prior studies have also highlighted some issues related to organizational behavior, such as change management, which may impede the adoption of these innovations in the healthcare space (e.g., Bush et al., 2017, Segrelles-Calvo et al., 2017).
Some of the key organizational issues include lack of training and routines (Fossum et al., 2011, Hossain et al., 2019), deficient IT support (McAlearney et al., 2013), and lack of infrastructure (Ser, Robertson, & Sheikh, 2014).
Broadly speaking, the prior literature has, in the past few years, identified a host of organizational, technological, professional, and patient-related inhibiting factors.
Raising a common concern related to technology usage, Bhattacherjee and Hikmet (2007) and Lin et al. (2012) emphasized the need to explore technology use anxiety/technology rejection to better understand the reasons behind healthcare providers’ resistance to e-health innovations.
- Some technology-related concerns identified in past studies include system functionality (Heath & Porter, 2019), complexity (De Wit et al., 2019), and misalignment between the technology and the logic of care (Plumb et al., 2017).
- Beyond the organizational and technological issues, some studies have also acknowledged doctors and clinical staff members’ concerns regarding the ways in which these innovations may affect patient well-being and safety.
- Some of the identified issues in this regard include threats to patients’ data privacy and security (Sarradon-Eck et al., 2021), adverse impacts on patient care (Heath & Porter, 2019), and medical liability concerns (Caffery, Taylor, North, & Smith, 2017).
… some authors emphasize the need to explore technology use anxiety/technology rejection to better understand the reasons behind healthcare providers’ resistance to e-health innovations.
A comprehensive review of the literature reveals that given the size of the healthcare sector, studies examining the drivers of providers’ resistance to e-health innovations remain scant.
Furthermore, most prior studies that have examined this resistance have focused on specific innovations, such as
- electronic health records (e.g., Al-Rayes et al., 2019, Ngafeeson and Manga, 2021),
- clinical decision support systems (e.g., Fossum et al., 2011, Zakane et al., 2014),
- the epidemic prevention cloud (Hsieh & Lin, 2020),
- computerized physician/provider order entry systems (e.g., Hoonakker et al., 2013), and
- telemedicine (Del Giudice Bagot et al., 2020, Segrelles-Calvo et al., 2017).
This limited scope and coverage underscores the need to better understand end-users’ responses to e-health innovations in a broader and more over-arching manner.
A comprehensive review of the literature reveals that given the size of the healthcare sector, studies examining the drivers of providers’ resistance to e-health innovations remain scant.
This limited scope and coverage underscores the need to better understand end-users’ responses to e-health innovations in a broader and more over-arching manner.
In addition, extremely few studies have examined the effects of individual differences on doctors and clinic staff members’ resistance to the adoption of e-health innovations.
- While scholars have identified various sources of individual differences in providers’ resistance, these sources, including personal innovativeness (Beglaryan, Petrosyan, & Bunker, 2017), …
- … professional status as physician or surgeon (Bush et al., 2017), profession- and specialty-related differences (Cresswell et al., 2017), and gender- and age-related differences regarding technology usage (Baudin, Gustafsson, & Frennert, 2020), remain underexplored.
Because resistance is a complex human response that can be driven by a variety of factors, additional research must explore the effects of various sources of individual differences on these professionals’ resistance to the use of e-health innovations.
In addition, extremely few studies have examined the effects of individual differences on doctors and clinic staff members’ resistance to the adoption of e-health innovations.
Because resistance is a complex human response that can be driven by a variety of factors, additional research must explore the effects of various sources of individual differences on these professionals’ resistance to the use of e-health innovations.
Finally, most existing studies were conducted during the pre-COVID-19 period, and none have examined the resistance of doctors and clinical staff towards the continued usage of various e-health innovations following their use of such innovations during the pandemic.
An understanding of provider resistance in this context has the potential to illuminate the inhibiting factors that outweigh the potential gains associated with the use of these innovations for effective healthcare delivery and management.
The present study addresses these gaps via a qualitative inquiry.
Finally, most existing studies were conducted during the pre-COVID-19 period, and none have examined the resistance of doctors and clinical staff towards the continued usage of various e-health innovations following their use of such innovations during the pandemic.
3. Methods and other Sections
See the original publication (this is an excerpt version only)

4. End-user resistance to e-health innovations
4.1. Healthcare provider barriers
Healthcare provider barriers refer to various inhibiting factors that doctors, nurses, and other clinical staff experience in the use of e-health innovations, such as EHR, CDSS, AccuRx text, and video consultation.
Based on the content analysis, healthcare providers experience barriers that can be categorized into three sub-themes:
- task-related barriers,
- patient-care barriers, and
- system barriers.
4.1.1. Task-related barriers
Task-related barriers refer to the impediments that healthcare providers experience involving workflow changes, system use, time commitment, communication challenges, and others.
In particular, the respondents emphasized challenges related to communication; the key issues here included the appropriate use of systems in communicating with other healthcare providers, miscommunication about updates and changes, and miscommunication because of documentation in different places.
Prior studies have also identified issues in communication-related to the use of specific e-health innovation products, such as telemedicine (Stronge, Nichols, Rogers, & Fisk, 2008), CDSS (Fossum et al., 2011), tele-orthopedics (Caffery et al., 2017), and health information technology (Alohali, Carton, & O’Connor, 2020).
The respondents also noted issues associated with their staff members’ efficient use of systems, which staff members were still learning to use.
Here, the main impediment the respondents identified was the potential for human error in data entry, including incorrectly uploading handwritten notes, uploading limited information, and struggling to keep records up to date.
Once again, past studies have likewise identified data entry and information-related issues among the impediments doctors and clinical staff encounter (e.g., Campling et al., 2017, McAlearney et al., 2013).
For instance, one of the respondents, a nurse in the geriatrics department with seven years of experience in the healthcare sector, noted:
“The major challenge is communication between the systems- even within the epic. For example, pointclickcare has no connectivity with epic- so a patient arrives from the hospital to the rehab/snf a nurse will have to enter all the orders manually after I verified them. Plenty of time to mess up. Another problem if hospital a has epic — hospital b has it — they most likely have different builds which don’t talk to each other. then you have to hit the care everywhere button and dig through a garbage heap of data.” [P23, Male, 33 years old]
In addition to the communication and data-related barriers, healthcare providers at different levels also noted that the use of e-health innovations for different functions had
- changed their work flow,
- increased their time spent on the system,
- imposed tedious documentation requirements,
- caused them to exceed the allotted consultation time, and
- increased their stress due to system outages, difficulties in reading, reviewing, comparing, and editing data, and challenges integrating paper and online records.
In fact, these workflow issues are long standing, as revealed by prior studies in the area (e.g., Kelly et al., 2017, Ser et al., 2014).
A respondent who had six years of experience and was associated with a pharmacy remarked:
“Sometimes, there is a lack of standard formatting within the EHR, which makes things difficult to read. It is also sometimes difficult to locate certain items (usually under menus or multiple sub-menus), although that would be similar to trying to locate items in a paper file. The primary drawback vs physical files is that e-health records usually lack a function to simultaneously compare or review items.” [P5, Female, 30 years old]
4.1.2. Patient-care barriers
Because the healthcare system and providers’ primary concern is to offer the best care to patients suffering from various diseases, concerns regarding the impact of e-health innovations on the quality of provider–patient interactions, the correctness of diagnoses, tracking progress, and others are particularly important.
Indeed, care quality concerns have persisted long after the introduction and increasing adoption of e-health innovations (Grabenbauer et al., 2011, Taylor et al., 2015, Yu et al., 2013).
Our study likewise found that healthcare providers’ worries regarding the effects of e-health innovations on the quality of care have not abated.
… care quality concerns have persisted long after the introduction and increasing adoption of e-health innovations [in early 2010´s] .
Our study likewise found that healthcare providers’ worries regarding the effects of e-health innovations on the quality of care have not abated.
We uncovered the following key concerns.
- First, updating records hinders patient interaction.
- Second, online interactions affect the adequacy of the information patients share.
- Third, online interactions entail a risk of unnecessary self-diagnosis.
- Fourth, in the case of certain illnesses, such as mental health issues, technology use can potentially compound the problem.
- Finally, diagnoses in certain specialties require a visual inspection.
A doctor with 13 years of experience in dermatology noted:
“The quality of consultation can be variable. This is largely dependent on technology, such as the reliability of internet speed, video quality, and sound quality. This is especially important in a specialty like dermatology where a lot of this is visually related.” [P33, Male, 37]
Another respondent, a clinical staff member with eight years of experience in biochemistry, shared:
“Primarily issues with keeping results and reference ranges etc. up to date, as we cannot edit the system ourselves as we could previously. We now need to do this through the system provider, which delays important changes being implemented which impacts on patient care.” [P41, Female, 31 years old]
4.1.3. System barriers
Design, usability, reliability, and ease of use are perhaps the most common concerns impeding the digital/technology-enabled transformation of any sector, including healthcare.
System barriers — issues related to the interface, design, quality, reliability, ease of use, and other characteristics of e-health systems — emerged as primary concerns among the healthcare providers in our study.
Once again, issues related to these systems’ intuitiveness and usability have long persisted, with academic researchers noting their existence with concern (Grabenbauer et al., 2011, Heath and Porter, 2019, Litvin et al., 2012).
The persistence of these concerns is both interesting and alarming because the digitalization of healthcare — starting with Healthcare 1.0 in the 1970s through Healthcare 4.0 in 2016 (Tanwar, Parekh, & Evans, 2020) — has a sufficiently lengthy history for firms offering e-health innovations to overcome system-related barriers.
The persistence of these concerns is both interesting and alarming because the digitalization of healthcare — starting with Healthcare 1.0 in the 1970s through Healthcare 4.0 in 2016 — has a sufficiently lengthy history for firms offering e-health innovations to overcome system-related barriers.
However, these issues continue to cause problems in the form of clunky, non-intuitive designs, limited technology reliability (i.e., servers crashing), interruptions due to system downtime, and difficulties accessing, locating, and transferring data.
One respondent, a clinical specialist engineer with 13 years of experience in medical physics, noted:
“Technology isn’t reliable with servers going down or unable to transfer data across from one to another.” [P49, Male, 43 years old]

4.2. Organizational barriers
Organizational barriers refer to various factors at the organizational level of the healthcare sector that cause resistance to the adoption as well as the effective and efficient continued use of various e-health innovations.
Our content analysis led us to categorize the organizational barriers in the healthcare space into two sub-themes:
- threat perception and
- infrastructural barriers.
4.2.1. Threat perception
Scholars have long discussed risk barriers in varied technology contexts, including online travel agencies, mobile wallets, and food delivery apps (e.g., Talwar et al., 2020, Talwar et al., 2021).
Scholars have long discussed risk barriers in varied technology contexts, including online travel agencies, mobile wallets, and food delivery apps
Since their entrance into the healthcare sector, e-health innovations — as well as the risks associated with them, such as routine system failure risks and very sector-specific medical liability risks (e.g., Poss-Doering et al., 2018, Hans et al., 2018, Wang et al., 2015) — have figured prominently in past research.
Our study, conducted in 2021, found that similar concerns still plague healthcare organizations, …
… causing multiple stakeholders to resist the adoption or continued, seamless use of e-health innovations — despite the ability of those innovations to promote a much-needed digital transformation of the sector.
Our study, conducted in 2021, found that similar concerns [about e-health innovations — as well as the risks associated with them] still plague healthcare organizations, …
…causing multiple stakeholders to resist the adoption or continued, seamless use of e-health innovations — despite the ability of those innovations to promote a much-needed digital transformation of the sector.
The key issues identified in this context include
- the risk of a system crash,
- low reliability of computer systems,
- vulnerability to cyberattacks,
- concerns about data security,
- issues related to patient privacy, and
- susceptibility to litigation and medical liability.
A doctor in the ENT department with five years of experience explained:
“When I’ve worked at hospitals with electronic prescribing, I’ve always found it easier, but we switched back to paper after the NHS cyberattack of 2018 so I guess vulnerability to cyberattack.” [P55, Male, 36 years old]
Another respondent, a nurse in the geriatrics department with seven years of experience in the healthcare sector, expressed concerns regarding the risk of litigation:
“Risk for litigation and the complexity of visits. My notes have grown pages long — with extra fluff to hit arbitrary billing requirements that just add extra time. Clicking buttons for metrics that are set by IT and administration that have no concept or concern for my patients.” [P23, Male, 33 years old]
4.2.2. Infrastructural barriers
Infrastructural barriers capture obstacles associated with the limited availability of hardware, the quality of software, and the planning and execution of the entire set-up to support digitalization in healthcare organizations.
Our qualitative inquiry, conducted in the UK, a developed economy, confirmed several key infrastructural constraints, including the lack of uninterrupted internet connectivity.
Past scholars have noted internet connectivity as well as a limited number of computers and ineffective software among the key barriers associated with the use of e-health innovations (e.g., Plumb et al., 2017, Ser et al., 2014, Serrano et al., 2020).
Our qualitative inquiry, conducted in the UK, a developed economy, confirmed several key infrastructural constraints, including the lack of uninterrupted internet connectivity.
We found similar barriers in the present context.
For instance, one respondent, a clinical staff member with two years of experience in optical treatment, observed:
“The software we use is good, but we only have one computer at the practice, and so only one practitioner can enter information at any given time.” [P6, Female, 50 years old]
Another respondent, a nurse with 20 years of midwifery experience, described the lack of infrastructural support for the use of e-health innovations:
“…access to computers and the Internet in all settings and having enough devices so that all staff can access [the system] when they need to [as well as] problems with software/updates, especially out of hours when there is no support service.” [P17, Female, 41 years old]
In sum, the key issues identified from the infrastructural perspective include
- the lack of equipment, which hinders simultaneous use,
- the need for regular server and software upgrades, systems that lack cross-compatibility,
- uniformity, and integration at the organizational level, which poses challenges for accessing information, and
- the absence of ownership of the data.

4.3. Patient barriers
Patient barriers refer to healthcare providers’ perceptions about the difficulties their patients experience in the use of e-health innovations.
Because the healthcare system exists for patient care, patient acceptance of e-health innovations is crucial for the diffusion of such innovations.
Through our content analysis, we identified two key sub-barriers that healthcare providers perceived among patients:
- usability and
- resource barriers.
4.3.1. Usability barriers
Many past studies have examined the barriers patients experience in the adoption and subsequent use of e-health innovations.
These studies have identified a variety of barriers — from practical usability issues to technology anxiety (e.g., Deng et al., 2014, Alohali et al., 2020, Tsai et al., 2020).
… studies have identified a variety of barriers — from practical usability issues to technology anxiety
Although healthcare providers served as the unit of analysis in our study, we were able to identify-two pertinent sub-barriers related to patients.
Such barriers are important to acknowledge because healthcare providers understand their patients intimately, and if they perceive that the patients are uncomfortable using e-health innovations, they will also have reservations about using them.
The key usability barriers the providers perceived their patients to have were
- the usability and interactivity of mobile apps,
- difficulty in accessing information,
- complex and confusing usage, and
- the language barrier for patients who did not speak English as their first language.
A respondent with two years of experience in digital health remarked:
“People frequently complain about usability — especially with mobile apps — and aren’t always motivated to continue using. Concern about data security and privacy can also be an issue.” [P33, Female, 25 years old]
Another respondent, a clinical staff member with 14 years of experience in podiatry, acknowledged the confusion e-health innovations can create for patients:
“The technologies cannot be used by every service user. The difficulty is they do not understand the technology and get confused.” [P59, Female, 37 years old]
4.3.2. Resource barriers
We have used the term “resource barriers” to represent the limited nature of patients’ device or internet connectivity, which can hinder their use of e-health innovations.
Our respondents articulated these concerns when discussing the challenges associated with the effective use of e-health innovations.
For example, a healthcare staff member with one year of experience in general practice surgery observed:
“Not all info can be accessed by the NHS app. Many of our regular patients are elderly, so they cannot access EHRs (i.e., booking the COVID vaccine/ virtual appointments) and would feel better coming in face to face, which isn’t always possible at the moment. Furthermore, most of them don’t have compatible mobile phones.” [P18, Female, 22 years old]
Similarly, a speech and language therapist with three years of experience commented:
“The Internet is very frequently a problem. Some poorer families do not have access to the Internet other than their phone data, and it could come at a cost to engage in a session.” [P46, Female, 27 years old]
On the whole, the key issues we identified in this context include problems with
- internet access,
- limited access to information through apps,
- the difficulties elderly patients encounter in accessing systems,
- the lack of universal access among patients to compatible mobile phones, and
- patients’ use of phones that do not support downloading apps or enable video consultations.
Among the most significant of these challenges is the fact that some poorer families lack internet access, which means that they must rely on their phones’ data plans and may thus face additional expenses if they opt to engage in a virtual health session.
While the past literature has devoted extremely limited attention to this aspect, scholars have acknowledged that patients’ limited resources may impede the adoption and subsequent usage of e-health innovations (e.g., Dubin et al., 2020).
While the past literature has devoted extremely limited attention to this aspect, scholars have acknowledged that patients’ limited resources may impede the adoption and subsequent usage of e-health innovations

4.4. End-user barriers
End-user barriers capture the inhibiting factors healthcare providers believe both they and their patients face.
These factors, which emerged from our coding of participating healthcare providers’ qualitative responses, align well with the barriers to innovations identified by past studies in the context of both tangible products and services and digital innovations (e.g., Ram and Sheth, 1989, Talwar et al., 2020).
Here, we have categorized end-user barriers to e-health innovations into three sub-themes:
- self-efficacy barriers,
- tradition barriers, and
- image barriers.
4.4.1. Self-efficacy barriers
Self-efficacy barriers represent the inhibiting factors that arise from end-users’ (i.e. healthcare providers and patients’) limited abilities to use e-health innovations effectively and competently.
Acknowledging the existence of these barriers across all user groups, prior research has linked them to a lack of technical aptitude and computer use skills, among other factors (e.g., Bhatnagar et al., 2017, Dubin et al., 2020, Plumb et al., 2017).
The respondents in our study admitted that both they and their patients lack the necessary degree of technology savviness.
The respondents in our study admitted that both they and their patients lack the necessary degree of technology savviness.
For example, a doctor with two years of experience in the accident and emergency department observed:
“The user must be well aware of how to use computers and should have good computer knowledge.” [P40, Male, 27 years]
Another respondent, a clinical psychologist with five years of experience, noted:
“I work in an area where patients don’t have access to the latest technology or phone/internet data plans. Older generations sometimes find using technology difficult to learn, both patients and staff members. When the system goes down, it creates a lot of problems as we can’t access necessary information.” [P2, Female, 41 years old]
In sum, our respondents observed various challenges, including
- the inability of some providers and patients to use certain technologies,
- a lack of technological understanding among both patients and healthcare providers, and
- patients and providers’’ inadequate degree of technology competence, particularly in terms of computer use skills.
4.4.2. Tradition barriers
Tradition barriers refer to the barriers that users (both healthcare providers and patients) experience as a result of their habits and/or the status quo.
We have extrapolated the term “tradition barrier” from innovation resistance theory (IRT), which Ram and Sheth (1989) proposed.
In the context of our study, tradition barriers represent inhibiting factors such as
- patients’ preference for visiting a health facility to receive a diagnosis,
- patients’ resistance to change and hesitance to interact with the necessary apps,
- a generational gap wherein older patients who are not tech-savvy prefer the “old” way of doing things,
- the need for healthcare providers to be trained and change their habits before using new systems,
- persistent negative attitudes toward technology among certain users, and
- hospitals’ continued partial adherence to old systems, which entails a combination of digital and hard-copy records and makes the use of e-health innovations counterproductive.
To our knowledge, prior studies in the area have not specifically examined tradition barriers, although some have alluded to patients and healthcare providers’ resistance to change as an obstacle (e.g., Al-Rayes et al., 2019; Beglaryan et al., 2017; Mikolasek, Witt, & Barth, 2018).
Our respondents offered some interesting observations regarding tradition barriers.
For instance, an end-of-life care nurse with 15 years of experience in palliative care remarked:
“Challenge is associated with people being competent and up to speed with how it works and positively embracing the technology.” [P1, Male, 37 years old]
Another respondent, a medical laboratory technician with six years of experience, observed:
“Our clients (many older) struggle with accessing information and need to be instructed step by step. Many older patients are upset that we cannot give them hard copies and must access thief information online or requested to be sent via mail.” [P35, Female, 27 years old]
4.4.3. Image barriers
The present study defines image barriers as the perception among healthcare providers that e-health innovations can negatively impact themselves and their patients.
As with tradition barriers, we have extrapolated these “image barriers” from the classic IRT barriers (Ram & Sheth, 1989).
Past studies have described image barriers as the degree to which end-users harbor negative perceptions about a particular innovation (Claudy, Garcia, & O’Driscoll, 2015).
To our knowledge, the extant literature has not specifically examined image barriers.
However, some scholars have observed negative perceptions among end-users — both healthcare providers and patients — toward e-health innovations (e.g., Cocosila and Archer, 2016, Taylor et al., 2015, Zobair et al., 2020).
… some scholars have observed negative perceptions among end-users — both healthcare providers and patients — toward e-health innovations
The following responses confirm the existence of these image barriers in healthcare providers’ minds.
For example, a medical scribe with six years of experience in emergency medicine commented:
“The primarily challenge using e-health for me is feeling disconnected from the patient. While doing vital signs, I find myself turning from the patient to the computer to enter and back. It makes conversation disjointed, as well as my attention decreased from the patient. This is not a new problem with e-health; it is well-documented and attributable for decline in healthcare job satisfaction. Secondarily, all the administrative tasks in Epic can be frustrating. Every day is a new dot phrase or a new wording required for the chart. It’s hard to keep up with and I always feel there should be a simpler way. Again, this is not a new problem. The entirety of the scribe job was to reduce this burden from the primary healthcare providers and allow them more facetime with the patient. The inefficiency of current e-health systems has created an entirely new role in healthcare, which I find sad.” [P27, Female, 23 years old]
A doctor with nine years of experience in sexual health also lamented:
“With tele medicine you don’t get a chance to build a rapport or examine patients. Sometimes that’s okay, but you could end up missing something.” [P39, Female, 34 years old]
Overall, the key image barriers among providers include
- difficulties in capturing and maintaining patient engagement,
- limited opportunities to build a rapport with patients, a sense of disconnection from patients,
- the potential for a decline in healthcare job satisfaction,
- the perception of frequent system changes, the perception of current e-health systems as inefficient,
- the potential for notification fatigue, which may cause staff to overlook patient alerts and just “click through,” and
- the belief that e-observations hinder the ability to notice trends.
From the patient perspective, the perceived image barriers largely stem from patients’ belief that remote consultations are not as effective as face-to-face interactions and from their lack of confidence that submitting an online form will result in action being taken on their request.
From the patient perspective, the perceived image barriers largely stem from patients’ belief that remote consultations are not as effective as face-to-face interactions …
… and from their lack of confidence that submitting an online form will result in action being taken on their request.

4.5. Individual differences in perceived barriers
The literature has extensively debated the effects of differences in respondents’ socio-demographic profile on their attitudes toward technology, including their resistance to various digital innovations (Talwar, Talwar, et al., 2020).
The literature has extensively debated the effects of differences in respondents’ socio-demographic profile on their attitudes toward technology, including their resistance to various digital innovations
In the specific context of resistance to e-health innovations, past studies have noted individual differences based on various socio-demographic aspects.
- For instance, Beglaryan et al. (2017) identified personal innovativeness — an individual characteristic — among the major barriers to physicians’ EHR acceptance.
- Meanwhile, Bush et al. (2017) confirmed differences between pediatric physicians and surgeons’ resistance and attitudes toward an EHR platform that supported structured data entry systems (SDES).
- Similarly, other studies have noted differences in resistance depending on profession, practice, and specialty (Barrett and Stephens, 2017, Cresswell et al., 2017, Wang et al., 2015), gender, age (Baudin et al., 2020), and other factors.
However, these findings are too narrow.
Our review of the responses we received did not reveal any gender-based variations in the respondents’ perceptions of various barriers.
However, distinct age-related differences emerged, with respondents observing the presence of a generational gap and a particular resistance among older patients to the use of e-health innovations.
… distinct age-related differences emerged, with respondents observing the presence of a generational gap and a particular resistance among older patients to the use of e-health innovations.
One respondent, a pharmacist with 12 years of experience in infectious diseases, offered the following insights:
“One of the greatest challenges is the generational gap with older patients who are not as tech-savvy and have great difficulty either downloading the necessary applications or being able to log into the system for virtual telehealth visits.” [P8, Male, 34 years old]
Similarly, we noticed individual differences in perceived barriers across various specialties, particularly mental health and dermatology.
In this regard, a psychologist with 20 years of experience noted:
“Also, in mh (mental health) we have to consider paranoia and psychosis and how this can affect the way we use technology. We have to do a huge amount of face-to-face contact. Using technology can at times worsen a patient’s presentation and often simply isn’t an option.” [P3, Female, 41 years old]

5. Discussion and implications
Because e-health innovations had received a lukewarm response prior to the COVID-19 pandemic and have become prominent only during the current health crisis, …
… it is important to understand whether the concerned stakeholders are using e-health systems as a temporary resort or as a long-term solution.
Indeed, observers have expressed valid concerns that the end of the pandemic (or at least the full vaccination of the vast majority of the population) may serve as the pivotal point at which e-health systems reassume a fringe role or become a preferred mode treatment.
Already, various studies and reports have noted a reversion to the traditional, largely non-digital method of healthcare delivery and administration (e.g., Mehrotra et al., 2020), indicating the persistence of end-user resistance towards e-health innovation.
Recognizing that digital transformation driven by relevant and useful innovations is the only way to make healthcare cost-effective, accessible, and inclusive, we contend that this continued resistance cannot be ignored.
… various studies and reports have noted a reversion to the traditional, largely non-digital method of healthcare delivery and administration , indicating the persistence of end-user resistance towards e-health innovation.
Recognizing that digital transformation driven by relevant and useful innovations is the only way to make healthcare cost-effective, accessible, and inclusive, we contend that this continued resistance cannot be ignored.
We thus conceptualized our study to examine the barriers healthcare providers perceive to exist against e-health innovations introduced in their organizations and against such innovations in general.
We proposed two research questions to achieve the objectives of our study.
In response to RQ1, which explored the perceived barriers impeding end-users and healthcare organizations’ seamless adoption and continued usage of various e-health innovations, we collected data from healthcare providers through a qualitative study and analyzed the data to identify open, axial, and selective codes.
In doing so, we identified four broad categories of barriers from four perspectives: healthcare providers, healthcare organizations, patients, and all end-users (both providers and patients).
Within each broad group, we also identified sub-barriers.
As presented in Table 2, these included three sub-barriers — task-related, patient-care, and system barriers — for healthcare providers, two sub-barriers — threat perception and infrastructural barriers — for healthcare organizations, two sub-barriers — usability and resource barriers — for patients, and three sub-barriers — self-efficacy, tradition, and image barriers — for both healthcare providers and patients as end-users.
We discussed each sub-barrier in detail based on the respondents’ perspectives and the findings of prior studies.
Next, in response to RQ2, which examined the impact of individual differences, such as socio-demographic factors, healthcare specialty, level in the professional hierarchy (doctor, nurse, etc.), and number of years of experience, on perceived barriers, we examined the collected data using the socio-demographic details in Table 1.
Our findings confirmed the existence of age-related and specialty-related differences in the perceived barriers.
Our findings confirmed the existence of age-related and specialty-related differences in the perceived barriers.
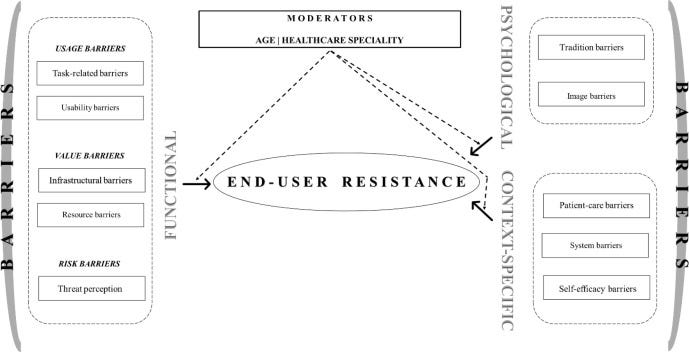
Based on our findings, we propose a conceptual framework grounded in Ram and Sheth (1989) IRT.
In its classic version, IRT identified five barriers: usage, value, risk, tradition, and image.
Subsequently, the theory combined usage, value, and risk as functional barriers and tradition and image as psychological barriers.
In its classic version, IRT identified five barriers: usage, value, risk, tradition, and image. Subsequently, the theory combined usage, value, and risk as functional barriers and tradition and image as psychological barriers.
Functional barriers capture the changes that an innovation may require in end-users’ existing habits, routines, and workflow (Ram & Sheth, 1989).
Within this category, usage barriers describe the perceived incompatibility of the innovation with the users’ practices.
Meanwhile, value barriers refer to the performance-to-price value of any innovation or the cost of using that innovation compared to those of prevailing practices.
Finally, risk barriers arise from end-users’ assessments of the uncertainties the innovation might bring.
In contrast, psychological barriers capture end-users’ perceptions regarding the innovation’s potential incompatibilities with their current beliefs and values (Ram & Sheth, 1989).
Within this category, tradition barriers refer to conflicts between the innovation and end-users’ prevailing behaviors, processes, norms, and prior experiences.
Image barriers represent end-users’ unfavorable assessments of the innovation in terms of its image and efficacy as well as the consequences of its use.
In the years that followed the publication of Ram and Sheth (1989) seminal work, scholars have used IRT in multiple contexts — some in its generic version and others in its expanded version to identify context-specific barriers (e.g., Seth et al., 2020, Talwar et al., 2020).
Drawing upon these past studies, we categorize the identified barriers constituting end-user resistance to e-health innovations into three broad groups:
- (a) functional barriers,
- (b) psychological barriers, and
- © context-specific barriers.
We further divide each of these into pertinent sub-groups.
Accordingly, within functional barriers, we categorize task-related and usability barriers as classic usage barriers because they pertain to the challenges healthcare providers and patients perceive to be involved in the use of e-health innovations.
Next, we classify infrastructural and resource barriers as classic value barriers because they represent the cost/economic implications of the use of e-health innovations, which may reduce the benefits healthcare organizations and patients expect to derive from such innovations.
Finally, and quite logically, we classify threat perception as a classic risk barrier because it pertains to various vulnerabilities healthcare organizations may face if they utilize these innovations.
Our content analysis of the collected data also revealed the existence of two classic psychological barriers: tradition and image.
Therefore, we employ the same terminology to represent these barriers.
Finally, we extend the classic IRT to the context of healthcare by proposing patient-care, system, and self-efficacy barriers as context-specific barriers.
In addition to the barriers mentioned above, our conceptual model includes two moderating variables — age and healthcare specialty, which our study confirmed as potential sources of individual differences in the experienced barriers. Fig. 1 presents the proposed conceptual framework.
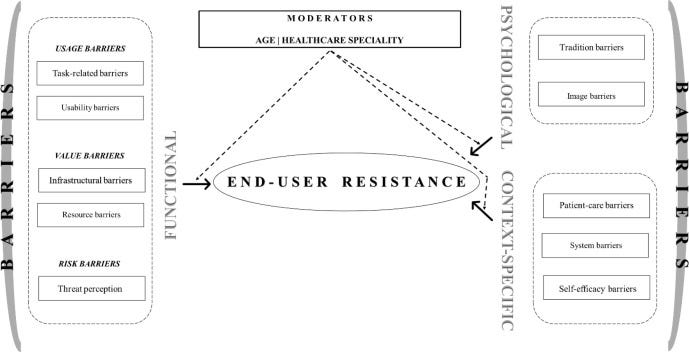
Fig. 1. Conceptual framework: End-user resistance to e-health innovations.
The findings of our study enabled us to make useful contributions to theory and practice, as discussed below.
5.1. Theoretical implications
Our study offers three key theoretical contributions.
First, ours is one of few attempts to examine the barriers to the use of e-health innovations for healthcare delivery and administration in the post-COVID-19 era.
In this regard, our study enriches the literature by identifying the barriers experienced by healthcare providers associated with different specialties and experienced in the use of different e-health innovations.
Past studies have focused on specific innovations, such as EHR (e.g., Barrett & Stephens, 2017), or they have confined themselves to specific specialties, such as mental health (e.g., Ser et al., 2014).
In contrast, our study provides broader insights that can guide future researchers efforts to examine the barriers to e-health innovations in different settings.
Second, regarding sources of individual differences in providers’ perceived barriers, our study makes interesting contributions that may have implications for research not only on e-health innovations but in other digital contexts as well.
While analyzing the qualitative responses, we observed no differences in the perceived barriers based on gender, experience, or level in the professional hierarchy.
Rather, we noted differences solely based on age and healthcare specialty.
These findings narrow the scope of future inquiry and provide researchers with specific inputs to advance their investigations in this area.
While analyzing the qualitative responses, we observed no differences in the perceived barriers based on gender, experience, or level in the professional hierarchy.
Rather, we noted differences solely based on age and healthcare specialty.
Finally, our study offers a concrete contribution by formulating a conceptual framework grounded in the seminal IRT (Ram & Sheth, 1989).
In essence, the framework discussed in the preceding part identifies various barriers that constitute consumers’ (end-users’) resistance to e-health innovations.
Specifically, it offers a classification of these barriers into the classic IRT barriers of usage, value, and risk as functional barriers and tradition and image as psychological barriers.
In addition, it identifies context-specific barriers that reflect end-users’ resistance to innovations in the healthcare sector.
It further identifies the pertinent moderating variables that can affect the strength of the association between each barrier and such resistance.
This framework thus advances research in the area by clarifying the key challenges scholars face in examining varied healthcare settings.
This framework thus advances research in the area by clarifying the key challenges scholars face in examining varied healthcare settings.
5.2. Practical implications
Three key practical implications emerge from our study.
First, our findings indicate that despite the ongoing digital transformation of business and personal life, the perceived barriers impeding the adoption and continued use of e-health innovations are quite basic and related to issues in the day-to-day use of such innovations for consultation, diagnosis, and healthcare administration.
This revelation suggests that firms engaged in the development of e-health innovations should first focus on providing a simple and intuitive interface, preferably with voice support to guide users.
This revelation suggests that firms engaged in the development of e-health innovations should first focus on providing a simple and intuitive interface, preferably with voice support to guide users.
In addition, we strongly suggest structuring apps that support patient–provider interactions so that they do not require a high-speed internet connection and do offer multi-language options for users who do not speak English as their first language.
In essence, we recommend that firms offering these innovations align their products with their end-users’ profile, appreciating that in the healthcare sector, these users possess varying degrees of technological expertise and access.
In essence, we recommend that firms offering these innovations align their products with their end-users’ profile, appreciating that in the healthcare sector, these users possess varying degrees of technological expertise and access.
Taking these steps would accelerate the diffusion of such innovations by overcoming the usage-related barriers that healthcare providers experience and perceive their patients to experience.
Second, we recommend that regulators be mindful of their role in mitigating the barriers that hinder the diffusion of e-health innovations.
For instance, our study reveals that concerns regarding cyberattack, data security and patient privacy, and litigation and medical liability act as risk barriers inhibiting the adoption and continued use of e-health innovations.
For instance, our study reveals that concerns regarding cyberattack, data security and patient privacy, and litigation and medical liability act as risk barriers inhibiting the adoption and continued use of e-health innovations.
We, therefore, suggest that concerned regulatory bodies issue specific guidelines and enact appropriate statutes that align with the nature of the healthcare sector and offer legal protection to healthcare providers against unjustified litigation/liability arising from their use of e-health innovations.
We, therefore, suggest that concerned regulatory bodies issue specific guidelines and enact appropriate statutes that align with the nature of the healthcare sector and offer legal protection to healthcare providers against unjustified litigation/liability arising from their use of e-health innovations.
At the same time, the state should, at a fee, provide adequate server spaces to ensure that sensitive data are encrypted in a centralized, government-controlled cloud space without breaching the ownership of data of each healthcare organization.
At the same time, the state should, at a fee, provide adequate server spaces to ensure that sensitive data are encrypted in a centralized, government-controlled cloud space without breaching the ownership of data of each healthcare organization.
Finally, because digital transformation is here to stay and facilitates cost-effective and time-efficient care, …
… healthcare organizations (large hospitals in particular) that are associated with medical colleges and nursing schools should make the necessary curricular changes …
… to ensure that all pre-service doctors, nurses, and other clinical staff receive mandatory training in technology use in the healthcare sector.
In addition, healthcare organizations introducing e-health innovations should pay particular attention to implementation so that they can
- successfully integrate their systems across all specialties and facilities
- while ensuring ease of authorized access,
- tailoring information input requirements to minimize the duplication of information, and
- allocating adequate resources to support uninterrupted usage.
… healthcare organizations (large hospitals in particular) that are associated with medical colleges and nursing schools should make the necessary curricular changes …
… In addition, healthcare organizations introducing e-health innovations should pay particular attention to implementation
At the same time, organizations should negotiate with firms providing e-health products/services to secure onsite personnel support and chat-based online support to address any challenges end-users (healthcare providers and patients) might face.
At the same time, organizations should negotiate with firms providing e-health products/services to secure onsite personnel support and chat-based online support to address any challenges end-users (healthcare providers and patients) might face.

6. Limitations and future research direction
Our study provides valuable insights that not only augment the accumulated literature but also offer actionable inputs for practice.
Despite its significant contributions, however, our study — like any academic inquiry — also entails certain limitations in its methodology and scope.
Acknowledging these limitations is a crucial prerequisite to proposing future research directions.
In terms of its methodological limitations, our study employed a mono-method approach to collect data via qualitative, open-ended essays.
Although qualitative studies are considered acceptable for exploratory studies and have been used by prior studies in the area (e.g., Cresswell et al., 2017, Plumb et al., 2017, Sarradon-Eck et al., 2021), mixed-method studies can yield more robust insights.
We thus suggest that future scholars utilize research designs that collect data from the target group via multiple methods.
Second, we conducted our study in a single developed country, the UK.
The barriers we identified thus may not be generalizable to countries in different parts of the world and at different stages of development.
Nevertheless, future researchers can easily remedy this limitation by using our qualitative study to collect data from other geographical locations.
Such efforts would also create scope for comparative studies into the ways in which the identified barriers vary across the stages of development.
With consumer behavior studies noting that individualistic versus collectivist cultures can impact consumer responses (e.g., Ferraris, del Giudice, Grandhi, & Cillo, 2020), scholars in this area might also examine the ways in which individual resistance toward e-health innovations varies across cultures.
The resulting granular insights would have the potential to help firms designing e-health innovations to provide more customized solutions and thereby pre-empt or at least mitigate some of the perceived barriers before rolling their products/services out to healthcare providers.
Finally, we collected qualitative data from only one end-user group — healthcare providers.
While we could have generated deeper insights by including patients as respondents, such an approach also could have diluted the specificity of inputs.
Future researchers should thus collect data from patients as end-users of e-health innovations and map the barriers specific to them.
Regarding its scope, our study has the limitation that we have not empirically tested the proposed conceptual model.
Although such empirical testing would have further strengthened the validity of our contribution, our model already has a robust foundation in qualitative data and the IRT framework and thus can guide future empirical studies.
References
See the original publication
About the authors & affiliations
Shilpa Iyanna a,b , Puneet Kaur c,d,* , Peter Ractham e , Shalini Talwarf , A.K.M. Najmul Islam g
a Newcastle Business School, Northumbria University, UK
b College of Business, Abu Dhabi University, UAE
c Department of Psychosocial Science, University of Bergen, Norway
d Optentia Research Focus Area, North-West University, Vanderbijlpark, South Africa
e Department of Management Information System, Thammasat Business School, Thammasat University, Thailand
f S.P. Jain Institute of Management and Research (SPJIMR), Mumbai, India
g LUT University, Lappeenranta, Finland
Shilpa Iyanna (PhD) has over 20 years of research and teaching experience. The recipient of several academic awards, including the highly competitive Nottingham University Business School Ph.D. Scholarship, she earned her Ph.D. in Marketing from Nottingham University Business School, University of Nottingham, UK. As well as being published in international journals and conferences, she is a reviewer and guest editor for the Renewable and Sustainable Energy Reviews special issue on ‘Sustainable Production and Consumption in the UAE.’ Dr. Iyanna’s research interests are in customer behavior in relation to customer value, value co-creation, consumer attitude and behavior, consumer satisfaction, and consumer goals. She is currently studying sustainable consumption related to lifestyles, attitudes towards changing consumption patterns, drivers of societal consumption patterns, and values attached to behavior and lifestyles that impact consumption patterns.
Puneet Kaur (DSc) is currently a postdoctoral researcher at Department of Psychosocial Science, University of Bergen, Norway. Her research appears in Journal of Retailing and Consumer Services, International Journal of Information Management, Computers in Human Behaviour, International Journal of Hospitality Management, Information Technology & People among others.
Peter Ractham (PhD) is an Associate Professor in the Department of MIS and a director of Center of Excellence in Operations and Information Management, Thammasat Business School, Thammasat University. His research focuses on ICT-enabled innovation, social media analytics and e-business. He holds a PhD in Information Systems & Technology from Claremont Graduate University, Claremont, USA.
Shalini Talwar (PhD) holds a PhD in Management Studies and MBA in Finance & Marketing. Currently, she is Associate Professor at S.P. Jain Institute of Management and Research (SPJIMR), Mumbai. She has published her work in high-ranked refereed journals, including Technovation, Technological Forecasting and Social Change, Psychology & Marketing, Journal of Business & Industrial Marketing, Journal of Sustainable Tourism, Business Strategy and the Environment, International Journal of Production Research, and Journal of Business Research, among others.
A.K.M. Najmul Islam is an Associate Professor at the LUT School of Engineering Science, LUT University, Finland. He also works as University Research Fellow at the Department of Future Technologies, University of Turku, Finland. Dr. Islam holds a PhD (Information Systems) from the University of Turku, Finland and an M. Sc. (Eng.) from Tampere University of Technology, Finland. His research has been published in top outlets such as IEEE Access, Information Systems Journal, Journal of Strategic Information Systems, European Journal of Information Systems, Technological Forecasting and Social Change, Computers in Human behaviour, Journal of Medical Internet Research, Internet Research, Computers & Education, Information Technology & People, Telematics & Informatics, Journal of Retailing and Consumer Services, Communications of the AIS, and Behaviour & Information Technology, amongst others.
Originally published at https://www.sciencedirect.com.