institute for
health transformation
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
January 31, 2023
EXECUTIVE SUMMARY
The AHRQ report on diagnostic errors in emergency departments (EDs) presents alarming findings
- The report states that with 130 million ED visits in the US, there could be more than 7 million diagnostic errors and 2.5 million related harms, including potentially preventable permanent disability or death.
- 350 000 patients suffering potentially preventable permanent disability or death.”
The authors of the article provide insight into the issue of diagnostic errors in EDs and explain why they occur more often when diagnosis is difficult.
To help with the transition from data to improvements, the authors offer 3 insights:
- 1.First, diagnostic errors are universal and implicate all specialties and areas of health care
- 2.Second, diagnostic errors are largely invisible and greater transparency is needed.
- 3.Third, the medical profession needs to take a systems approach to reduce diagnostic errors.
INFOGRAPHIC
DEEP DIVE
Misdiagnosis in the Emergency Department
JAMA Network
Jonathan A. Edlow, MD1; Peter J. Pronovost, MD, PhD2
January 27, 2023
The Agency for Healthcare Research and Quality (AHRQ) commissioned a systematic review of diagnostic errors in the emergency department (ED) that was conducted by the Johns Hopkins University Evidence-Based Practice Center and released on December 15, 2022.1
Few will read the entire 744-page document.
However, most will read the eye-catching finding:
- “With 130 million U.S. ED visits,
- estimated rates for diagnostic error (5.7%),
- misdiagnosis-related harms (2.0%), and
- serious misdiagnosis-related harms (0.3%)
- could translate to more than 7 million errors,
- 2.5 million harms, and
- 350 000 patients suffering potentially preventable permanent disability or death.”
Studies that report large numbers of medical harms often produce reactions of alarm from some and outrage from others.
The major US emergency medicine societies wrote a joint response to the AHRQ report that, based on serious methodological concerns, challenges the AHRQ report’s conclusions.2 Diagnostic errors are especially prone to raise concern among clinicians because they are associated with physicians’ self-identity and are often viewed as personal failings resulting in feelings of shame rather than as a signal to investigate the systems issues behind the problem. Because the underlying data are often imperfect, physicians often challenge their accuracy rather than interpret them as a call for improvement.

To help with the transition from data to improvements, we offer 3 insights.
- 1.First, diagnostic errors are universal and implicate all specialties and areas of health care
- 2.Second, diagnostic errors are largely invisible and greater transparency is needed.
- 3.Third, the medical profession needs to take a systems approach to reduce diagnostic errors.
1.First, diagnostic errors are universal and implicate all specialties and areas of health care.
The AHRQ report notes that diagnostic error rates estimated in the ED are remarkably similar to those in other areas of medicine. The report estimates a total ED diagnostic error rate of 5.7%1 and notes that other studies have found a 6.3% rate among primary care patients3 and roughly 8% in hospital autopsies.4 The AHRQ report estimates that serious harms occur in 0.3% of ED visits and notes other studies indicate a 0.1% rate in primary care and 0.4% in hospitalized patients.1 Even if the data from a heterogeneous group of studies analyzed in the report do not allow such precise point estimates of error, all agree that there is room for improvement in diagnostic accuracy in the ED.1,2 The error and harm rates cited for ED visits, primary care patients, and hospitalized patients are very similar, even though emergency clinicians see any and all patients, unscheduled, under great time pressure, often in an overcrowded, chaotic environment with frequent distractions. As the AHRQ report acknowledges, “The ED is one of the most challenging clinical settings to practice medicine.” That diagnostic errors are not higher in emergency medicine is, in the words of the report, “a testament to the skill and capability of practicing emergency physicians.”
Diagnosis is not always simple. Some diagnoses can be made accurately at a glance; others are difficult during the first hours; and some clinical problems are even undiagnosable early in their course. These diagnoses may be obvious days later, after more testing, more clinicians’ input, or simply more time, which can be the diagnostician’s friend. Studies that use a reference standard of the diagnosis at 30 days after an ED visit or at hospital discharge may classify a patient whose diagnosis changes with more data as a diagnostic error. They are diagnostic errors, but they are not necessarily preventable and may not cause the harm to the patient.
The factor of time is intrinsic to emergency medicine, where the goal is not necessarily to make a specific diagnosis every time, but rather, to make a safe disposition (treat time-dependent conditions, hospitalize some patients for further evaluation, or discharge others for further outpatient care). A safe disposition with an incomplete diagnosis is an acceptable outcome of ED care. Nevertheless, an incorrect diagnosis due to incomplete data resulting in harm should still be a target for system-based diagnostic quality improvement.
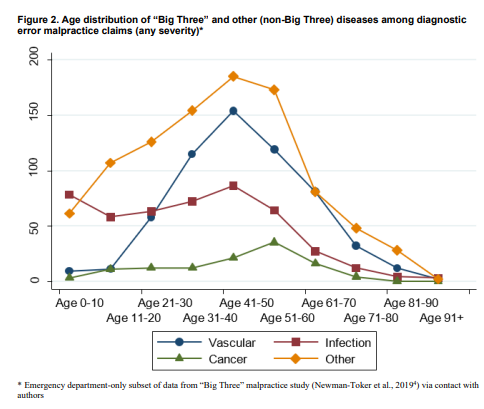
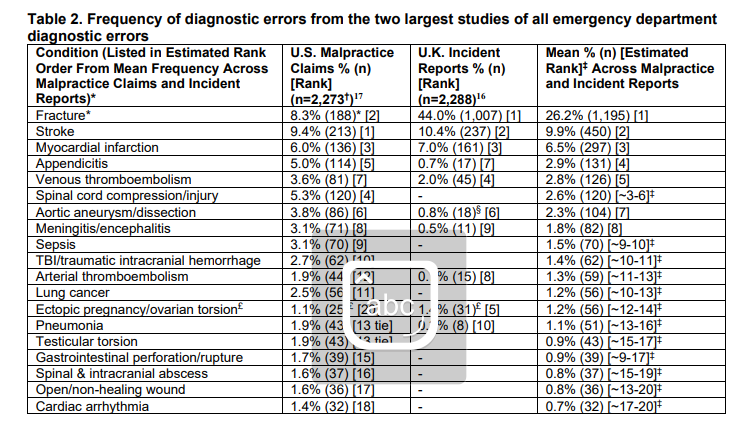
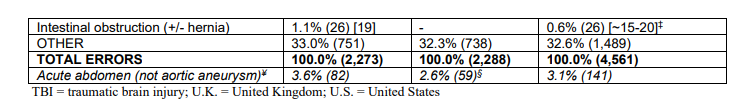
Diagnostic errors occur more often when diagnosis is difficult. We rarely misdiagnose strokes presenting with unilateral weakness, but diagnosing stroke in patients presenting with dizziness and vomiting is intrinsically trickier and misdiagnosis is frequent.5 The AHRQ report provides direction toward targeted solutions, a key insight being that just 15 clinical conditions accounted for 68% of diagnostic errors associated with high-severity harms, which makes the problem far more tractable. Most of these conditions belong to 3 disease categories — vascular events, infections, and cancer (the “big three”).6 These are top causes of disease and death across clinical settings, so they should be prime targets for interventions.
Reduction of diagnostic errors should be viewed as a system issue across all health care settings and specialties. Policy makers, the private sector, and physicians should all seek systems solutions. Simply doing more testing is neither an elegant solution nor an effective one. Wider availability and increasing use of abdominal computed tomographic scans in the 1990s did not lower the misdiagnosis rate of appendicitis or the proportion of cases of perforated appendicitis.7 Simply doing “more testing” could have other adverse effects such as worsened ED overcrowding, radiation exposure, higher costs, and a low-value cascade of follow-up tests for incidental findings that never needed to be found in the first place.

2.Second, diagnostic errors are largely invisible and greater transparency is needed.
The medical profession needs to apply standardized definitions, and establish routine, operational metrics to consistently assess rates of error and their underlying causes. The authors of the AHRQ systematic review made exhaustive efforts to minimize bias. As they wrote, the data on diagnostic error are messy, and health care professionals have not yet adopted routine use of valid and practical ways to monitor diagnostic errors. Policy makers should accelerate investments in practical value-added ways to define and measure diagnostic errors in real time, such as the Symptom-Disease Pair Analysis of Diagnostic Error (SPADE) method that leverages administrative data to identify misdiagnosis-related harms at scale and could be applied as a national benchmark.8

3.Third, the medical profession needs to take a systems approach to reduce diagnostic errors.
Because of the perception of personal culpability associated with diagnostic errors, their invisibility, and the lack of technologies to reduce them, health care professionals have relied on the heroism of individual clinicians rather than the design of safe systems to prevent diagnostic errors. Given the cognitive burden of remembering the typical and atypical presentations of thousands of diseases and the extreme time pressures — ED overcrowding, patchy access to specialty consultation or technology such as magnetic resonance imaging — the health care system is “perfectly designed” to produce the sorts of significant harm to which the report calls attention.
The health care profession needs to accept that physicians, being human, are fallible — systems of care to reduce diagnostic errors to a minimum must be designed. ED overcrowding is not an emergency medicine problem. It is a system problem and requires a system-level solution. Specific diagnosis-focused solutions might include checklists or cognitive aids that are pushed real time to clinicians, capturing, correcting, and preventing diagnostic errors in a timely and blame-free way. Machine learning, better access to advanced imaging and specialist consultation, development of reliable diagnostic biomarkers, improvements in health information technology, and clinical decision support need to be studied and employed as parts of the solution. Training modules that target the big 3 disease entities need to be developed at the medical school, residency, and practicing physician levels for all specialties involved in diagnosing those patients. The AHRQ report documents that investments of these types that have been made for diagnosis of myocardial infarction can yield important dividends, the misdiagnosis rate for myocardial infarction being only about 1.5%, compared with 10% to 56% for the other serious medical conditions.2 Of course, because myocardial infarction is so common, even this small percentage represents an area for improvement. The health care profession needs to make concerted efforts to redesign systems of care to prevent harm from the other common conditions.
The media reaction to the AHRQ report will temporarily make diagnostic errors publicly visible, but without durable system-wide measures and interventions, they will soon receive less attention and the harms to patients will continue. The AHRQ report should serve as a call to action. Policy makers should aim for and invest in a 50% reduction in diagnostic deaths and permanent disabilities within 5 years. The engineering to accomplish this goal exists.9 It has been used for more than 30 years in other industries (eg, the airline industry) and in medicine (eg, reductions in infections from central venous and urinary bladder catheters). The paradigm of how we interpret diagnostic errors must shift from trying to “fix” individual clinicians to creating systems-level solutions to reverse system errors. To err may be human, but that does not mean that all medical errors have human causes or that we should accept diagnostic errors as an inevitable cost of doing business.
References
See the original publication https://jamanetwork.com












