This is a republication of the paper “Patient-Centered Payment for Care of Chronic Conditions”, with the title above.
health and tech
institute
for continuous health transformation
Joaquim Cardoso MSc
Founder, Chief Research & Editor
February 12, 2023
SOURCE:
The Journal of Ambulatory Care Management
Miller, Harold D. MS
Center for Healthcare Quality & Payment Reform, Pittsburgh, Pennsylvania.
January 18, 2023
Abstract
Current payment systems make it difficult for both specialists and primary care practices to provide all of the services needed by patients with chronic conditions.
- “Value-based payment” programs have failed to solve these problems.
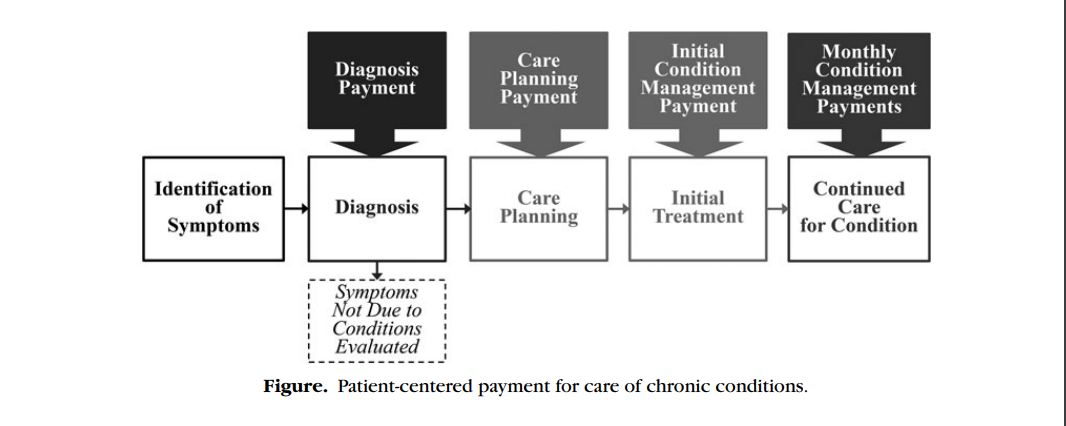
In a patient-centered payment system, there should be 4 separate payments designed specifically to support each of the phases of chronic condition care:
- (1) Diagnosis Payment,
- (2) Care Planning Payment,
- (3) Initial Condition Management Payment, and
- (4) Monthly Condition Management Payments.
- Physicians should be accountable for delivering evidence-based services to patients in each phase of care, and payment amounts should be higher for more complex patients.
THE MAJORITY of adults have a chronic condition such as arthritis, asthma, chronic obstructive pulmonary disease, diabetes, heart disease, or kidney disease, and more than one-fourth have 2 or more chronic conditions ( Boersma et al., 2020 ).
- More than one-sixth of children have a chronic health condition ( Rezaee & Pollock, 2015 ).
- On average, health care spending is 6 times as high for patients who have chronic conditions as for those who do not ( Buttorf et al., 2017 ),
- and a significant portion of this spending is used for treatment of the complications that arise from inadequate care ( Gregg et al., 2019 ).
- In addition, the cost of lost productivity for workers with chronic conditions and their employers exceeds the amount spent on their health care ( Goetzel et al., 2004 ; Loeppke et al., 2009 ).
Although many chronic conditions can be managed effectively by a primary care practice if the practice has adequate time and staff to do so, a subset of patients will need support from a specialist in addition to or instead of a primary care practice for 1 or more aspects of their care:
- Diagnosis: In some cases, it is difficult to determine whether a patient has a chronic disease without specialized training and experience. Many patients are misdiagnosed, particularly those with less common conditions and conditions with symptoms similar to other diseases (Committee on Diagnostic Error in Health Care, 2015 ).
- In addition, many patients receive unnecessary tests and/or unnecessarily expensive tests to rule out unlikely diagnoses (Mitchell, 2010 ).
- In some cases, these tests can lead to false-positive results that contribute to inaccurate diagnoses and unnecessary treatments.
- Treatment planning: There are generally multiple approaches to treating a diagnosed condition.
- There are tradeoffs between effectiveness, safety, side effects, and cost among different treatment options, and patients need information and assistance in determining which option is best for them.
- Because primary care physicians treat a wide range of different conditions, it is difficult for them to stay current on treatment options and tradeoffs, particularly for less common conditions.
- Care for severe, complex, and uncommon conditions: Patients who have severe conditions, uncommon conditions, and multiple chronic conditions, and patients for whom standard treatments are not effective or have problematic side effects may need specialized services or expertise that a primary care practice cannot provide.
Conclusion
Health insurance will never be affordable unless the cost of health care is reduced.
- Current approaches to value-based payment have shown little benefit in terms of either reducing costs or improving quality, while creating heavy administrative burdens for providers and undesirable incentives to reduce or delay the care patients need.
- Patient-centered payment for care of chronic conditions can address the weaknesses in current fee-for-service payment systems while avoiding the serious problems created by “risk-based” payment models.
- Patient-centered payment would support patient-centered care, which is what patients want to receive and what physicians and other providers want to deliver.
- Successful implementation will also require a change in the top-down, payer-driven approach that has been used in the past to change payment systems.
Payers must collaborate with providers to design and implement payments that will support high-value care, and all payers must implement similar approaches to payment in order for providers to transform the way they deliver services.
- With a collaborative, multipayer approach to implementation, patient-centered payment can enable higher-quality care, less avoidable spending,
- … and more financially sustainable physician practices-a win-win-win for patients, payers, and providers.
Health insurance will never be affordable unless the cost of health care is reduced.
DEEP DIVE
THE PROBLEMS WITH CURRENT PAYMENT SYSTEMS
Current payment systems make it difficult for specialists as well as primary care practices to provide all of the services needed by patients with chronic conditions:
- Inadequate time for accurate diagnosis and successful treatment planning: The amounts paid for office visits are often not large enough to allow a physician to spend the time necessary to accurately diagnose complex symptoms and to work with the patient to develop a treatment plan that is appropriate and feasible for that patient.
- Lack of payment or inadequate payment for high-value services: There is often no payment at all for many of the high-value services physician practices should deliver to help patients with chronic conditions, such as phone calls to monitor a patient’s condition in order to respond quickly when problems arise, education from nurses or other practice staff about how to successfully manage their condition, and palliative care services for a patient with an advanced illness. Even when fees for these services are available, some patients who need them are ineligible or the fee amounts are lower than the cost of delivering the services appropriately.
- Financial penalties for successful treatment: Specialists who treat patients with chronic conditions are typically paid on the basis of the number of times the patient comes to the physician’s office and the number of treatments the physician practice provides. As a result, the specialty practice is penalized financially if it helps the patients avoid exacerbations or slow the progression of their condition.
Typical “value-based payment” programs, such as pay-for-performance, shared savings, and accountable care organizations, have done little to support higher-quality care for patients with chronic conditions because there are no new or different payments for the services that are not adequately supported by existing fees ( Miller, 2017 ).
If a specialist helps an accountable care organization receive a shared savings bonus, there is no assurance that any portion of that bonus will go to the specialist or that the amount they receive will cover the costs or offset the losses they incurred. Even if a health system or accountable care organization is receiving a “population-based payment” for all services (ie, a fixed capitation payment for each patient), specialists will usually continue to receive standard fee-for-service payments because no alternative approach to paying for their specific services has been developed. In addition, most value-based payment programs focus primarily on reducing spending, not on improving the quality of care, and they do not adjust measures of spending or quality for differences in patient needs. This can penalize specialists for delivering care to the patients who most need their expertise and make it harder for complex patients to access effective care.

PATIENT-CENTERED PAYMENT FOR CARE OF CHRONIC CONDITIONS
A different method of paying for care of chronic conditions is needed that will solve the problems with current fee-for-service payment systems without placing physicians at risk for costs they cannot control or penalizing them for treating patients who have greater needs as current value-based payment systems do.
In a patient-centered payment system for care of chronic conditions
- a patient with a chronic condition should be able to receive the services that will best address his or her specific needs;
- a patient with a chronic condition should be assured of receiving appropriate, evidence-based care;
- payments for services should be adequate to cover the cost of delivering those services in a high-quality manner, particularly for patients with complex needs; and
- a patient with a chronic condition should be able to select which physician practice or provider will deliver care for the condition based on the quality and cost of the services he or she will receive.
The care needed for most chronic conditions can be divided into 4 distinct phases:
- diagnosis,
- care planning,
- initial treatment, and
- continued care for the condition.
The types of services needed in each phase are different from those in other phases, and the quality of care delivered in each phase has a significant impact on the outcomes patients experience and the cost of care they receive, not only during that phase but also in subsequent phases.
For example, an inaccurate diagnosis can lead to unnecessary or ineffective treatment, and failure to choose a plan of care that is feasible for the patient or failure to assist the patient in implementing the plan correctly during the initial months of care could result in unnecessary use of more expensive treatments or progression of disease in the future.
Some patients will be able to receive adequate services in each phase from their primary care practice. Other patients will need services from 1 or more specialty care providers in 1, some, or all of the phases. The only way to ensure that each patient can get appropriate specialty services for his or her specific needs and the only way to ensure that each specialist is paid appropriately for the services he or she provides is to create separate payments specifically designed to support each phase of care ( Figure).
Payment for diagnosis
Although there are thousands of different billing codes and associated fees used to pay physicians for performing individual procedures and tests, there are no billing codes or fees specifically designed to pay a physician to determine the cause of a patient’s symptoms or to determine whether a patient has a specific chronic disease.
Current payments are based on the number and length of office visits with the patient, not the time and resources required to determine an accurate diagnosis. A Diagnosis Payment is needed that is designed to support an accurate evaluation of the patient’s symptoms, regardless of how many visits the patient makes with the physician.
In addition, many unnecessary referrals from primary care practices to specialists could be avoided if the primary care physician was able to receive assistance from a specialist in making a diagnosis and/or determining whether a referral is appropriate.
A small Diagnostic Assistance Payment is needed to enable the specialist to provide this assistance.
Payment for care planning
There are typically multiple approaches to treating and managing a chronic condition.
The choices and the tradeoffs evolve continuously as new therapies are created and as new evidence emerges about the relative effects of treatments.
The expertise of a specialist will often be needed to identify the best alternatives, to educate the patient about the choices, and to assist the patient in deciding which to pursue.
The physician who prepares the care plan may be different from the physician who diagnoses the condition and/or the physician who will actually manage the patient’s care on an ongoing basis.
In a patient-centered payment system, a Care Planning Payment is needed that is specifically designed to support this phase of care.
In some cases, rather than referring the patient to a specialist for the full care planning process, a primary care physician may be able to prepare an appropriate care plan if he or she receives assistance from a specialist.
A small Care Planning Assistance Payment is needed to enable the specialist to provide this assistance.
Payment for initial condition management
Development of a care plan will trigger the beginning of what will usually be a lifetime of activities needed to manage the chronic disease, including both treatments and lifestyle changes designed to reduce the severity of symptoms caused by the chronic condition, to prevent exacerbations of the condition and associated complications, and ideally to slow the progression of the disease.
The most intensive efforts will generally be needed during the initial months of treatment.
A physician practice will need to spend a significant amount of time providing education and assistance to the patient in order to successfully implement a newly developed care plan and making revisions to the care plan based on
(1) any problems the patient experiences in implementing the plan, and
(2) whether the care succeeds in addressing the patient’s needs.
Failure to do this could lead patients to abandon treatment prematurely or to switch to unnecessarily expensive or ineffective treatments.
An Initial Condition Management Payment is needed to ensure that the physician practice has adequate time and resources for the important work during the initial month of care.
For some chronic conditions, and for patients with complex needs, the Initial Condition Management Payment may need to continue for several months to allow adequate time for the care plan to be fully implemented (eg, if medications or dosages need to be phased in), to assess the efficacy of the treatment(s), to identify any adverse side effects, and, if necessary, to make modifications to the care plan and test their feasibility and effectiveness.
An additional Initial Condition Management Payment can be paid each month for those patients who require a longer period of time to finalize an effective treatment and management plan.
Payment for continued condition management
When a care plan has been successfully implemented and is expected to continue for an extended period of time, the Initial Condition Management Payments can end.
In some cases, a patient may have needed to receive care only from a specialist during the initial treatment period and then his or her primary care practice can take over ongoing management.
In other cases, a specialty practice may need to continue providing services indefinitely, such as for patients who have complex conditions and patients who need to receive medications that can have dangerous side effects, multiple treatments that must be carefully sequenced or timed, or treatments that are difficult to use correctly.
Ongoing care management services cannot be delivered effectively solely through office visits with the physician; patients need to be contacted between visits in order to prevent problems from occurring and to respond quickly when problems occur.
Moreover, it is problematic to pay for office visits when exacerbations occur (as is the case in current payment systems), because the practice is then penalized financially when it is able to prevent exacerbations from occurring.
In addition, although adjustments to a treatment plan for a chronic condition must generally be done by a physician or other clinician, services such as education, assistance, and monitoring can usually be performed primarily by nurses or other types of staff in the physician practice.
The most appropriate way to pay for this type of proactive, team-based care is through a Monthly Condition Management Payment for each patient that gives the physician practice flexibility to provide the combination of services that will be most effective and efficient for that patient.
This payment should be only for chronic condition management, however, not for any specific drugs, procedures, or tests the patient needs as part of his or her care plan; these other services should be paid for through service-specific fees designed to cover the costs of those services.

ACCOUNTABILITY FOR QUALITY AND UTILIZATION OF SERVICES
A patient-centered payment system also needs effective mechanisms for ensuring that each patient receives the most appropriate services for his or her specific health condition, that patients do not receive inappropriate or unnecessary services, and that services are delivered in the most effective way possible.
In theory, it would be desirable for physicians to receive “outcome-based payments,” but in practice, this is infeasible because most important outcomes are affected by patient-specific factors that cannot be controlled by physicians, and many important outcomes occur long after the physician’s services are delivered.
Bonuses or penalties based on quality or outcome measures are also problematic because the measures that are typically used do not measure the true quality of care and they can penalize physicians who care for higher-need patients ( Center for Healthcare Quality & Payment Reform, 2022 ).
A simple and effective approach to accountability is for the physician practice to bill the payer for one of the patient-centered payments if and only if
(1) the practice has delivered evidence-based services that are consistent with a Clinical Practice Guideline (CPG) applicable to the relevant phase of care, or
(2) the practice deviated from the guidelines for necessary, patient-specific reasons that are documented in the patient’s clinical record (eg, the patient was unwilling or unable to use the evidence-based treatment).
Evidence-based CPGs exist for diagnosis and treatment of most common chronic diseases and also for many less common conditions.
Encouraging use of the guidelines, while allowing deviations from them when necessary, enables the development of improved evidence about how to provide effective care for all patients ( Sox & Stewart, 2015 ).
Although most of the quality measures currently being used in value-based payment systems are based on CPGs, the guidelines are more comprehensive and nuanced than the quality measures.
In addition, since CPGs define which tests and procedures are appropriate and inappropriate in various situations, they can reduce use of unnecessary services in a more patient-centered way than the burdensome and problematic prior authorization processes typically used by health insurance plans.
In addition to delivering evidence-based services to the patient, a physician practice that is delivering condition management services should proactively monitor the patient’s condition to identify any problems the patient is experiencing and to assess the outcomes of the services delivered.
A Standardized Assessment, Information, and Networking Technology (SAINT) provides a systematic way for patients to provide the physician practice with actionable information about any physical and/or emotional problems they are having and whether the services the practice is providing to the patient are addressing the issues that are of most concern to that patient ( Wasson, 2020 ).
In contrast to current value-based payment systems that measure only the average quality of care for groups of patients, this approach ensures that each individual patient is receiving the most appropriate, high-quality care for his or her individual needs.
It also eliminates the need for burdensome systems of reporting large numbers of simplistic quality measures that impose significant administrative costs on both providers and payers.

ADEQUACY OF PAYMENT
No matter what method is used to pay for diagnosis, care planning, or treatment, if the payment amount is not sufficient to cover the time and cost involved in delivering high-quality care, the patient may be given an inaccurate diagnosis, receive unnecessary or unnecessarily expensive services, or experience avoidable complications.
Consequently, the payment amounts should be based on what it costs for a physician practice to deliver high-quality care.
Payments should not be based on what a health plan has paid in the past or the amount of savings the physician practice is expected to produce, because that will not ensure that the physician practice has sufficient time and resources to deliver high-quality, evidence-based care.
In each phase of care, the payment amount should be higher for subgroups of patients who have greater needs in order to support the additional time that the physician practice would need to spend with these patients.
Current systems of “risk-adjusting” payments do a poor job of this; they ignore differences in patients other than diagnosed chronic diseases, and the risk scores are designed to predict the payer’s future spending on a patient and not the time required for a physician practice to provide evidence-based care.
A better approach is for the physician managing the patient’s care to assign the patient to 1 of 2 or 3 predefined complexity levels based on the characteristics of patients that affect the amount of time the physician practice will need to spend delivering services during that phase of care.
The physician practice should then receive higher payments for patients in the higher complexity levels.
For example, there should be higher Monthly Condition Management Payment amounts for patients receiving complex treatments and patients who have characteristics that make them more susceptible to serious exacerbations or complications.

PATIENT ACCESS AND CHOICE
A patient with a chronic condition should be able to choose the physician practice or other provider he or she believes will deliver services that meet his or her needs.
Some patients will want their primary care practice to do this, while other patients will want or need to have a specialist practice to do so, even if they continue to receive wellness care and occasional acute care from a primary care practice.
The patient should make his or her choice explicit by enrolling with the physician practice the patient wants to deliver the services.
That physician practice can then bill the patient’s health insurance plan for the appropriate patient-centered payments.
This eliminates the need for the complex, burdensome, and inaccurate systems payers currently use for retrospectively “attributing” patients to physician practices without any input from either the patient or the practice.
In addition to paying physician practices adequately for evidence-based chronic condition management services, payers need to minimize or eliminate cost-sharing requirements (ie, copayments, coinsurance, and deductibles) that prevent or discourage patients from receiving those services.
Effective chronic condition management will prevent exacerbations of the chronic condition from occurring, and the savings to a health insurance plan from not having to pay for hospital treatment of exacerbations will likely exceed any savings achieved by requiring high levels of cost-sharing for physician services.

COSTS AND BENEFITS OF PATIENT-CENTERED PAYMENT
The patient-centered payments described previously can be easily implemented in existing physician practice billing systems and health plan claims payment systems by creating new billing codes for each of the payments and assigning adequate payment amounts to each.
This is far less burdensome and expensive than the complex systems of patient attribution, risk adjustment, and quality measurement used in most value-based payment systems.
Although spending on the services delivered by physician practices would likely increase when patient-centered payments are used, particularly for patients who have complex conditions or who face social barriers in maintaining and improving their health, delivery of evidence-based services should also result in offsetting savings from fewer inaccurate diagnoses, fewer unnecessary tests and treatments, and fewer exacerbations and complications of treatment.
The physician practice’s payments should not be contingent on whether total spending decreases, however, since that would create perverse incentives to undertreat patients in ways that produce short-term savings but result in higher spending in the long run.
In addition, the value of better care for working-age patients with chronic conditions is reflected in their productivity as workers, not just in the amount spent on their health care.
Higher worker productivity has a direct economic benefit for employers that can offset higher amounts spent to support high-quality chronic condition care for their employees and families.

ACHIEVING A WIN-WIN-WIN FOR PATIENTS, PAYERS, AND PROVIDERS
Health insurance will never be affordable unless the cost of health care is reduced.
Current approaches to value-based payment have shown little benefit in terms of either reducing costs or improving quality, while creating heavy administrative burdens for providers and undesirable incentives to reduce or delay the care patients need.
Patient-centered payment for care of chronic conditions can address the weaknesses in current fee-for-service payment systems while avoiding the serious problems created by “risk-based” payment models.
Patient-centered payment would support patient-centered care, which is what patients want to receive and what physicians and other providers want to deliver.
Successful implementation will also require a change in the top-down, payer-driven approach that has been used in the past to change payment systems.
Payers must collaborate with providers to design and implement payments that will support high-value care, and all payers must implement similar approaches to payment in order for providers to transform the way they deliver services.
With a collaborative, multipayer approach to implementation, patient-centered payment can enable higher-quality care, less avoidable spending, and more financially sustainable physician practices-a win-win-win for patients, payers, and providers.
Health insurance will never be affordable unless the cost of health care is reduced.
Originally published at https://journals.lww.com.




