the health strategist
institute of research and strategy
for health transformation and digital health
Joaquim Cardoso MSc
Chief Researcher & Editor of the Site
April 11, 2023
ONE PAGE SUMMARY
The World Health Organization (WHO) has faced many challenges in its 75-year history, including conflicts between major powers and a lack of focus on universal health care.
- The WHO is regarded as the go-to organization for setting global standards for vaccines and medicines, and it has been instrumental in alerting the world to new infectious diseases.
- However, boosting innovation and competitiveness has come at the expense of knowledge sharing, and COVAX, a scheme designed to provide vulnerable populations with COVID-19 vaccines, has struggled due to over-ordering by a small number of high-income countries.
- The WHO has created a facility that offers the technology for messenger RNA vaccines to low-income countries, but many argue that strengthening health systems, sharing knowledge, and preventing and controlling diseases are the responsibilities of governments, with the WHO taking a supporting role.
Despite the challenges, the WHO remains a trusted organization, and in many parts of the world, it is the primary healthcare provider.
In the aftermath of COVID-19, the WHO must prioritize universal health care to meet the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.
DEEP DIVE

The WHO at 75: what doesn’t kill you makes you stronger
Nature
Editorial
05 April 2023
The World Health Organization is emerging from the peak of the pandemic bruised. Its member states must get back to prioritizing universal health care.
There were times during the first year of the COVID-19 pandemic when the World Health Organization (WHO) must have felt as if it had been plunged into the middle of a heavyweight boxing match between China and the United States. China stopped its virologists and epidemiologists collaborating with their international colleagues just as researchers needed to share what they knew to understand the new virus. The United States, under then-president Donald Trump, blamed the WHO for being too close to China and attempted to punish the agency by announcing plans to withdraw funding (later reversed by the administration of current President Joe Biden).
But the WHO is no stranger to big power conflicts. Throughout its 75-year existence, it has been surrounded by international tensions, most notably the cold war between the United States and the Soviet Union ( E. Fee et al. Am. J. Public Health 106, 1912–1917; 2016). The US Congress approved US membership of the WHO on the condition that it could withdraw with a year’s notice. The Soviet Union did pull away between 1949 and 1955.
When thinking about the WHO’s 75 years, it’s worth remembering the time and circumstances of its creation. In the aftermath of the Second World War, the newly established United Nations and its specialized agencies, including the WHO, were designed to future-proof the world from another global conflict. Around 80 million people died during the two world wars, many from famine or disease.

The WHO’s founding constitution states unequivocally: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.”
And yet, the agency’s creators chose not to prioritize robust systems of universal health care that would meet these goals.
This absent focus is one factor in why infectious diseases continue to impact populations in low- and middle-income countries.
The eradication of smallpox in 1980 was a big win.
But for other diseases, the agency and its donors have been unable to reach targets, including in the elimination of HIV and AIDS, malaria and tuberculosis.
The WHO does, however, have a consistent record for establishing itself as the go-to organization for setting global standards for the efficacy, safety and quality of vaccines and medicines. As we have seen during the pandemic, the agency is central to alerting the world to new infectious diseases, helped in no small measure by the revolution in biomedicine and health data, especially genomics.
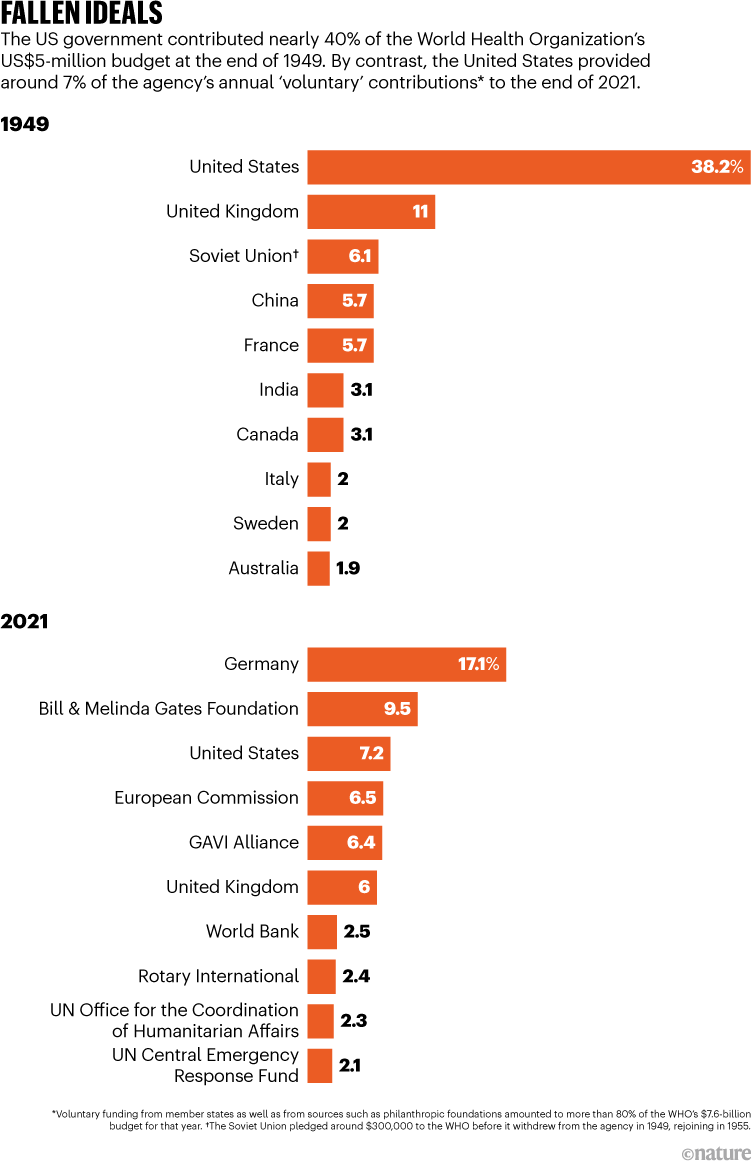
How the WHO operates and sets its priorities is also influenced by the economic-policy priorities of its member states. The agency was created by a handful of powers, many of which are still significant donors (see ‘Fallen ideals’). Contributions from the United States (including the Bill & Melinda Gates Foundation in Seattle, Washington) and European nations accounted for more than half of the agency’s US$7.6-billion income in 2021.
Boosting innovation and competitiveness has been a big priority, and this has come at the expense of knowledge sharing. In 1980, the United States enacted the Bayh-Dole Act allowing universities to commercialize inventions from federally funded research. This led to restrictions on what researchers could and couldn’t share. In 1995, the World Trade Organization established rules on intellectual property that have also made it difficult to share the knowledge needed to develop COVID-19 vaccines and therapies quickly and at scale. India and South Africa mounted a brave campaign ( Nature was among its supporters) to have COVID-19-related intellectual-property rights temporarily waived; but the odds were stacked against them.
The failure of COVAX, a scheme to provide vulnerable populations with COVID-19 vaccines, also prompted reflection on what is wrong with the architecture of global public health. COVAX struggled because governments in a small number of high-income countries over-ordered (and overpaid for) vaccines, leaving little for the rest of the world.

But the tide could be turning. African countries are determined to establish vaccine manufacturing on the continent. Knowledge sharing and vaccine equity are also at the heart of the draft text for a pandemic treaty that is currently being negotiated at the WHO.
In the face of scepticism from some of the WHO’s biggest donors, in 2021, the organization created a facility that offers the technology for messenger RNA vaccines to low-income countries, through an initiative created by former chief scientist Soumya Swaminathan and backed by director-general Tedros Adhanom Ghebreyesus.

Many continue to argue that strengthening health systems, sharing knowledge, and preventing and controlling diseases is principally the job of governments.
The corollary is that the WHO should take part, but not lead this work. But it shouldn’t be a case of having to choose. In some of the poorest parts of the world, the WHO is a second health ministry, running (or funding) primary-care clinics, delivering vaccinations and collecting data. In conflict zones, it is one of the few trusted organizations that can do all of these, as the world saw recently in northwest Syria.
Today, the WHO faces enormous challenges. Health systems are reeling amid the pandemic.
COVID-19 has not only killed nearly seven million people, but also set back global-health targets — from reducing global maternal mortality to achieving universal health coverage.
The WHO has come through the past few years bruised, but stronger and wiser.
Member states must get back to prioritizing universal health and supporting nations less able to achieve this on their own.
They must prioritize equity, access to knowledge and rediscovering their founding ideals, so the world is better prepared for the next emergency.
Member states must get back to prioritizing universal health and supporting nations less able to achieve this on their own.
They must prioritize equity, access to knowledge and rediscovering their founding ideals, so the world is better prepared for the next emergency.
Originally published at https://www.nature.com on April 5, 2023.








