the health strategist
research and strategy institute
Joaquim Cardoso MSc
Chief Research & Strategy Officer (CRSO),
Chief Editor and Senior Advisor
ONE PAGE SUMMARY
Central Message
While improved diagnostic capabilities and increased awareness of autism are factors contributing to the rise in autism diagnosis rates, there are also genetic and possibly environmental factors at play.
- The significant increase in autism rates is not solely due to better identification but could be influenced by a combination of genetic predisposition, changing demographics (such as older parental age), and potential environmental factors.
- There are also persistent challenges of racial disparities in autism diagnoses and the need for broader and more consistent screening for autism among young children.

Key Points
What is the problem?
- Autism rates have tripled among children in the New York and New Jersey metropolitan area from 2000 to 2016.
- Nationally, autism rates have also risen significantly, with 1 in 54 children diagnosed with autism by age 8 in 2016, compared to 1 in 150 in 2000.
What are the drivers?
- Advances in diagnostic capabilities and increased understanding of autism are driving the increase in diagnosis rates.
- Autism rates have risen more among children without intellectual disabilities compared to those with intellectual disabilities, indicating improved identification of cases with average or above-average IQs.
What are the issues?
- Racial disparities in autism diagnoses have narrowed, but persist. Black children without intellectual disabilities are 30% less likely to be diagnosed with autism compared to white children.
What are the causes?
- Around 83% of autism risk comes from inherited genetic factors, with approximately 2,000 to 3,000 genes contributing to autism.
- Older parents carry a higher risk of having children with autism.
- Environmental factors like exposure to air pollution are unlikely significant contributors but could exacerbate genetic risks.
- Emerging research suggests potential risk factors such as viral infections, vitamin D deficiencies, gut inflammation, and exposure to toxic chemicals, but solid evidence is lacking.
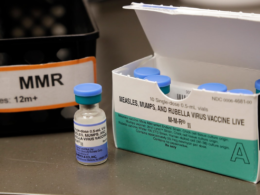
- Precisely what those other factors are is still unknown, but researchers are at least clear on one fact: Autism has nothing to do with vaccines.
What is the source?
- The findings were published in a study published Thursday in the journal Pediatrics.
What are the recommendations?
- Recommendations have been made to screen all toddlers for autism during routine checkups at pediatricians, though current screening rates are estimated to be around 50%.
- Broader screening criteria and improved diagnostics might contribute to increased opportunities for misdiagnoses.
This is a One Page Summary of the article “Autism rates have tripled. Is it more common or are we just better at diagnosis?”, written by By Aria Bendix, and published on NBC News,on Jan. 26, 2023.
To read the original publication https://www.nbcnews.com on January 26, 2023.
REFERENCE PULICATION

Pediatrics
Prevalence and Disparities in the Detection of Autism Without Intellectual Disability
ARTICLES| JANUARY 26 2023
Josephine Shenouda, DrPH, MS; Emily Barrett, PhD; Amy L. Davidow, PhD; Kate Sidwell, BA; Cara Lescott, BA; William Halperin, MD, DrPH, MPH; Vincent M. B. Silenzio, MD, MPH; Walter Zahorodny, PhD
BACKGROUND
- Intellectual ability predicts functional outcomes for children with autism spectrum disorder (ASD).
- It is essential to classify ASD children with and without intellectual disability (ID) to aid etiological research, provide services, and inform evidence-based educational and health planning.
METHODS
- Using a cross-sectional study design, data from 2000 to 2016 active ASD surveillance among 8-year-olds residing in the New York-New Jersey Metropolitan Area were analyzed to determine ASD prevalence with and without ID. Multivariable Poisson regression models were used to identify trends for ASD with ID (ASD-I) and without ID (ASD-N).
RESULTS
- Overall, 4661 8-year-olds were identified with ASD. Those that were ASI-I were 1505 (32.3%) and 2764 (59.3%) were ASD-N. Males were 3794 (81.4%), 946 (20.3%) were non-Hispanic Black (Black), 1230 (26.4%) were Hispanic, and 2114 (45.4%) were non-Hispanic white (white).
- We observed 2-fold and 5-fold increases in the prevalence of ASD-I and ASD-N, respectively, from 2000–2016.
- Black children were 30% less likely to be identified with ASD-N compared with white children.
- Children residing in affluent areas were 80% more likely to be identified with ASD-N compared with children in underserved areas.
- A greater proportion of children with ASD-I resided in vulnerable areas compared with children with ASD-N.
- Males had higher prevalence compared with females regardless of ID status; however, male-to-female ratios were slightly lower among ASD-I compared with ASD-N cases.
CONCLUSIONS
- One-in-3 children with ASD had ID. Disparities in the identification of ASD without ID were observed among Black and Hispanic children as well as among children residing in underserved areas.