the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
September 12, 2023
What is the message?
Geographic disparities in life expectancy among counties in the United States are substantial and have been growing over the past three decades.
These disparities are influenced by a combination of socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors.
To reduce these disparities and increase overall longevity, policy actions targeting socioeconomic and behavioral factors are crucial.

Key takeaways:
What is the main question addressed in the article?
- The main question addressed in the article is whether inequalities in life expectancy among counties in the United States are growing or diminishing, and what factors can explain the differences in life expectancy among counties.
What are the key findings of the study?
- Inequalities in life expectancy among US counties are large and increasing.
- Life expectancy at birth varies significantly between counties, with a gap of more than 20 years between the counties with the lowest and highest life expectancy.
- Absolute geographic inequality in life expectancy increased between 1980 and 2014, with the gap between the lowest and highest life expectancy widening.
- Absolute geographic inequality in the risk of death decreased among children and adolescents but increased among older adults.
- Socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors collectively explain 74% of the variation in life expectancy among counties.
- Most of the association between socioeconomic and race/ethnicity factors and life expectancy is mediated through behavioral and metabolic risk factors.
What are the implications of the study’s findings?
The study’s findings have important policy implications:
- Geographic disparities in life expectancy in the US are significant and worsening.
- Policies and programs targeting behavioral and metabolic risk factors have the potential to improve health and reduce geographic disparities.
- Addressing socioeconomic factors is also essential, but many of these disparities are mediated through behavioral and metabolic risk factors.
- Interventions should focus on age-specific trends in mortality, especially among older adults, to effectively reduce disparities.
- Policies aimed at reducing health inequalities can also contribute to addressing socioeconomic disparities in the long run.
What are some of the strengths of this study?
- The study used advanced small area models for estimating life expectancy and age-specific mortality rates, resulting in more precise estimates.
- It included all counties and considered age-specific mortality risks, providing a more comprehensive analysis of geographic inequalities.
- The study systematically explored the extent to which various factors contribute to variations in life expectancy among counties, shedding light on potential intervention strategies.
What are the limitations of this study?
- The data used for estimating life expectancy and related factors are subject to measurement error.
- The study did not assess whether increasing geographic inequality is due to changes in individual-level disparities or differential migration patterns.
- The analysis focused on cross-sectional associations, limiting its ability to establish causality or assess changes over time.
- Some relevant factors outside the categories considered in the analysis may contribute to geographic disparities but were not examined.
DEEP DIVE

Inequalities in Life Expectancy Among US Counties, 1980 to 2014Temporal – Trends and Key Drivers [excerpt]
JAMA Network
Laura Dwyer-Lindgren, MPH1; Amelia Bertozzi-Villa, MPH1; Rebecca W. Stubbs, BA1; et al Chloe Morozoff, MPH1; Johan P. Mackenbach, MD, PhD2; Frank J. van Lenthe, PhD2; Ali H. Mokdad, PhD1; Christopher J. L. Murray, MD, DPhil1
July 2017
Key Points
Question Are inequalities in life expectancy among counties in the United States growing or diminishing, and what factors can explain differences in life expectancy among counties?
Findings In this population-based analysis, inequalities in life expectancy among counties are large and growing, and much of the variation in life expectancy can be explained by differences in socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors.
Meaning Policy action targeting socioeconomic factors and behavioral and metabolic risk factors may help reverse the trend of increasing disparities in life expectancy in the United States.
Abstract
Importance Examining life expectancy by county allows for tracking geographic disparities over time and assessing factors related to these disparities. This information is potentially useful for policy makers, clinicians, and researchers seeking to reduce disparities and increase longevity.
Objective To estimate annual life tables by county from 1980 to 2014; describe trends in geographic inequalities in life expectancy and age-specific risk of death; and assess the proportion of variation in life expectancy explained by variation in socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors.
Design, Setting, and Participants Annual county-level life tables were constructed using small area estimation methods from deidentified death records from the National Center for Health Statistics (NCHS), and population counts from the US Census Bureau, NCHS, and the Human Mortality Database. Measures of geographic inequality in life expectancy and age-specific mortality risk were calculated. Principal component analysis and ordinary least squares regression were used to examine the county-level association between life expectancy and socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors.
Exposures County of residence.
Main Outcomes and Measures Life expectancy at birth and age-specific mortality risk.
Results Counties were combined as needed to create stable units of analysis over the period 1980 to 2014, reducing the number of areas analyzed from 3142 to 3110. In 2014, life expectancy at birth for both sexes combined was 79.1 (95% uncertainty interval [UI], 79.0-79.1) years overall, but differed by 20.1 (95% UI, 19.1-21.3) years between the counties with the lowest and highest life expectancy. Absolute geographic inequality in life expectancy increased between 1980 and 2014. Over the same period, absolute geographic inequality in the risk of death decreased among children and adolescents, but increased among older adults. Socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors explained 60%, 74%, and 27% of county-level variation in life expectancy, respectively. Combined, these factors explained 74% of this variation. Most of the association between socioeconomic and race/ethnicity factors and life expectancy was mediated through behavioral and metabolic risk factors.
Conclusions and Relevance Geographic disparities in life expectancy among US counties are large and increasing. Much of the variation in life expectancy among counties can be explained by a combination of socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors. Policy action targeting socioeconomic factors and behavioral and metabolic risk factors may help reverse the trend of increasing disparities in life expectancy in the United States.
Introduction
Studies have routinely shown that life expectancy in the United States varies geographically, in some cases dramatically.1–3 Counties are the smallest administrative unit routinely available in death registration data and represent an opportunity to explore the extent of geographic inequalities in the United States. In particular, tracking inequality at the county level over time is an important means of assessing progress toward the goal of more equitable health outcomes, as enshrined in the Healthy People 2020 objective: “Achieve health equity, eliminate disparities, and improve the health of all groups.”4 Moreover, county-level information on basic health outcomes is essential for appropriately targeting resources and designing and implementing health and social welfare policy at both the federal and state level.
Previous analyses of life expectancy at the county level have found large2,5 and increasing3 geographic disparities. However, these analyses either excluded or combined a large number of smaller counties, likely leading to an underestimation of geographic inequality. Moreover, recent research has highlighted the need to consider age-specific metrics of survival in addition to life expectancy overall. Case and Deaton6 identified differential trends in mortality rates among age groups, with middle age mortality rates stagnating or even increasing for certain populations, while mortality rates among older individuals continued to decline. Similarly, Currie and Schwandt7 identified differential trends in income-based inequalities by age, with inequalities generally declining among children and adolescents and increasing for older ages. To our knowledge, age-specific trends in geographic inequalities have not been previously described at the county level in the United States.
Beyond describing geographic variation in life expectancy, exploring what factors explain this variation might provide import insights into how to reduce inequalities and achieve more equitable health outcomes. Several previous analyses5,8,9 have used local data on all-cause mortality to explore this question and have identified a large number of socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors that are correlated with survival. However, these analyses have not systematically explored the extent to which county-level variation in life expectancy can be explained by the larger social and economic context of a county, the behavioral and metabolic risk profile of county residents, or the availability and quality of health care.
This analysis has 3 specific aims. First, to generate annual estimates of life expectancy and age-specific mortality risk for each county from 1980 to 2014. Second, to quantify geographic inequalities in life expectancy and age-specific mortality risks and to examine trends in geographic inequality over time. Third, to assess the extent to which variation in life expectancy is explained by variation in socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care access and quality.

Methods
Small Area Models for Estimating Life Expectancy and Age-Specific Mortality Risks
Unit of Analysis
All analyses were carried out at the county level. Counties were combined as needed to create stable units of analysis over the period 1980 to 2014, reducing the number of areas analyzed from 3142 to 3110 (eTable 1 in the Supplement). For simplicity, these units are referred to as “counties” throughout.
Data
Deidentified death records from the National Center for Health Statistics (NCHS)10 and population counts from the census bureau,11 NCHS,12–14 and the Human Mortality Database15 were used in this analysis. Deaths and population were tabulated by county, age group (0, 1-4, 5-9, …, 80-84, and ≥85), sex, and year. County-level information on levels of education, income, race/ethnicity, Native American reservations, and population density derived from data provided by the census bureau and NCHS was also incorporated (eTable 2 in the Supplement).
Small Area Model
Previously described and validated Bayesian small area models for estimating age-specific mortality rates by county were used in this analysis.16 These models incorporated 7 covariates (the proportion of the adult population who graduated high school; the proportion of the population that is Hispanic; the proportion of the population that is black; the proportion of the population that is a race other than black or white; the proportion of a county that is contained within a state or federal Native American reservation; the median household income; and the population density) and smooth mortality rates over space, time, and age to produce more stable estimates of the mortality rate in each county, year, and age group. Models were fit using the Template Model Builder Package17 in R version 3.2.4 (R Foundation).18 County-level estimates were scaled to ensure consistency with existing national-level estimates from the Global Burden of Disease study.19
Life Table Construction and Metrics
The method described by Wang et al20 was used to extrapolate mortality rates to older ages (5-year age groups up to age 110 years). Standard demographic methods were used to construct period life tables for each county and year from the age-specific mortality rates estimated by the small area model.21 Life expectancy at birth (e0) and the probability of death for 5 age groups—0 to 5 (5q0); 5 to 25 (20q5), 25 to 45 (20q25), 45 to 65 (20q45), and 65 to 85 (20q65)—were extracted from these life tables.
For each measure, absolute geographic inequality was quantified as the difference between the 99th and 1st percentile level, and relative geographic inequality was quantified as the ratio of the 99th to 1st percentile level. The corresponding measures using the 90th and 10th percentile were calculated as well.
Analysis of County-Level Variation in Life Expectancy
Data
A cross-sectional data set was constructed of variables correlated with life expectancy at the county level. To maximize the number of variables included, 2009, the year with the best data coverage, was used. Three groups of variables were considered. For the first group, variables related to the broader social, economic, and demographic context of a county were identified. Specifically: the poverty rate, median household income, proportion of the adult population who graduated high school, proportion of the adult population who graduated college, the unemployment rate, proportion of the population that are black, proportion of the population that are native American, and proportion of the population that are Hispanic. For the second group, behavioral and metabolic risk factors with high attributable burden in the United States22 for which reliable estimates were available at the county level were identified. The prevalence of obesity, leisure–time physical inactivity, cigarette smoking, hypertension, and diabetes were included. For the third group, variables related to access to health care and health care quality were identified. Three variables were ultimately included: the percentage of the population younger than 65 years who are insured, a quality index that is a composite of variables related to primary care access and quality based on Medicare data analyzed by the Dartmouth Atlas project,23 and the number of physicians per capita. eTable 3 in the Supplement provides details about the data sources for each of these variables.
Regression Models
A series of bivariate ordinary least squares regression models were fitted with life expectancy at birth in 2009 as the dependent variable and each of the variables listed above as independent variables to assess the independent relationship between each of these variables and life expectancy.
Many of the variables considered were highly correlated (eFigure 1 in the Supplement), making multivariate models including all of these factors challenging to interpret due to collinearity. Therefore, a principal component analysis24 was conducted on each group of variables and the first principal component from each (rescaled to run from 0 to 1) was used as a composite index representing the socioeconomic and race/ethnicity, behavioral and metabolic risk, and health care characteristics, respectively, of each county. A series of ordinary least squares regression models were fitted with life expectancy at birth as the dependent variable and each of these indices separately, and then in combination, as the independent variable(s). For all models, the estimated model coefficients and the adjusted and unadjusted R2 were extracted. As a sensitivity analysis, the full multivariate regression models using all of the factors separately were also fitted.
Results
Inequalities in Life Expectancy and Age-Specific Mortality Risk
There was considerable variation in mortality risk and life expectancy at the county level in all years. In 2014, life expectancy at birth for both sexes combined at the national level was 79.1 (95% uncertainty interval [UI], 79.0-79.1) years (76.7 [95% UI, 76.7-76.8] years for men, and 81.5 [95% UI, 81.4-81.5] years for women), but there was a 6.2-year gap (95% UI, 6.1-6.2) between the 10th and 90th percentile, a 10.7-year gap (95% UI, 10.5-11.0) between the 1st and 99th percentile, and a 20.1-year gap (95% UI, 19.1-21.3) between the lowest and highest life expectancy among all counties. Several counties in South and North Dakota (typically those with Native American reservations) had the lowest life expectancy, and counties along the lower half of the Mississippi and in eastern Kentucky and southwestern West Virginia also had very low life expectancy compared with the rest of the country. In contrast, counties in central Colorado had the highest life expectancies (Figure 1). Geographical patterns in mortality risk for each age group were similar, but not identical (eFigures 2-6 in the Supplement). Results by sex and for all counties and years are available in an online visualization tool.
Between 1980 and 2014, life expectancy at birth for both sexes combined in the United States increased by 5.3 (95% UI, 5.3-5.4) years, from 73.8 (95% UI, 73.7-73.8) to 79.1 (95% UI, 79.0-79.1) years (6.7 [95% UI, 6.7-6.8]) years, from 70.0 [95% UI, 70.0-70.0] to 76.7 [95% UI, 76.7-76.8] for men; 3.9 [95% UI, 3.9-4.0] years, from 77.5 [95% UI, 77.5-77.6] to 81.5 [95% UI, 81.4-81.5] for women). This masks massive variation at the county level; however, counties in central Colorado, Alaska, and along both coasts experienced much larger increases, while some southern counties in states stretching from Oklahoma to West Virginia saw little, if any, improvement over this same period (Figure 2). Similarly, there was considerable variation among counties in the percent decline in the mortality risk within each age group (eFigure 7 in the Supplement). While all counties experienced declines in mortality risk for children (ages 0 to 5 years) and nearly all counties (>98%) experienced declines in the mortality risk for adolescents (ages 5 to 25 years) and older adults (ages 45 to 65 and 65 to 85 years), a significant minority of counties (11.5%) experienced increases in the risk of death between ages 25 and 45 years.
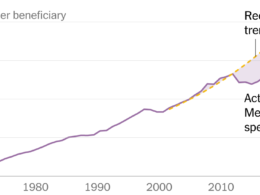
Absolute geographic inequality in life expectancy at birth increased between 1980 and 2014, with the gap between the 1st and 99th percentile increasing by 2.4 (95% UI, 2.1-2.7) years (Figure 3). However, for mortality risks, this pattern varied by age: the difference between the 1st and 99th among counties declined by 42.9% (95% UI, 40.4%-45.1%) among children (ages 0 to 5 years), by 18.9% (95% UI, 15.2%-22.7%) for adolescents (ages 5 to 25years), and increased by 10.1% (95% UI, 6.4%-14.1%), 15.0% (95% UI, 11.6%-18.4%), and 48.2% (95% UI, 42.7%-53.7%) for age groups 25 to 45 years, 45 to 65 years, and 65 to 85 years, respectively. Relative inequality rose for all age groups, likely due to the overall decrease in mortality risk over this period. Similar trends were observed when comparing the 10th and 90th percentiles (eFigure 8 in the Supplement).
Factors Related to Variation in Life Expectancy
Table 1 provides summary statistics for each of the variables included in the analysis of factors related to variation in life expectancy as well as the bivariate regression results. Statistically significant relationships with life expectancy were found for each variable. Detailed results of the principal component analysis are given in eTables 4 through 6 and eFigure 9 in the Supplement. The first principal component explained 42%, 79%, and 56% of the total variation in socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors, respectively. Table 2 lists the regression results based on these three indices. Socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors, when considered independently, explained 60%, 74%, and 27%, respectively, of the county-level variation in life expectancy. In combination, these 3 factors explained 74% of the variation. The effect size for the behavioral and metabolic risk factors index is similar in the combined model (Model 4) as in the model with just risk factors as a predictor (Model 2). In contrast, the effect size for socioeconomic and race/ethnicity factors is much reduced in the combined model (Model 4) compared with the model with just socioeconomic and race/ethnicity factors (Model 1), and is no longer statistically significant. The effect size for health care factors is also reduced in the combined model (Model 4) compared with the model with just health care factors (Model 3), but the effect is still statistically significant.
The corresponding results from the regressions using all variables separately are presented in eTable 7 in the Supplement. The overall amount of variation explained by each group of factors, both separately and in combination, is somewhat higher, but with the same ordering among the different groups of factors: 69% for socioeconomic and race/ethnicity factors, 77% for behavioral and metabolic risk factors, 31% for health care factors, and 82% for all factors combined.

Discussion
This study found large—and increasing—geographic disparities among counties in life expectancy over the past 35 years. The magnitude of these disparities demands action, all the more urgently because inequalities will only increase further if recent trends are allowed to continue uncontested.
This is an excerpt of the original article.
Limitations
This is an excerpt of the original article.
Conclusions
Geographic disparities in life expectancy among counties are large and increasing. Much of the variation in life expectancy among counties can be explained by a combination of socioeconomic and race/ethnicity factors, behavioral and metabolic risk factors, and health care factors. Policy action targeting socioeconomic factors and behavioral and metabolic risk factors may help reverse the trend of increasing disparities in life expectancy in the United States.
References
This is an excerpt of the original article.
Authors and Affiliations
Laura Dwyer-Lindgren, MPH1; Amelia Bertozzi-Villa, MPH1; Rebecca W. Stubbs, BA1; Chloe Morozoff, MPH1; Johan P. Mackenbach, MD, PhD2; Frank J. van Lenthe, PhD2; Ali H. Mokdad, PhD1; Christopher J. L. Murray, MD, DPhil1
1Institute for Health Metrics and Evaluation, University of Washington, Seattle
2Department of Public Health, Erasmus MC, Rotterdam, Netherlands
Originally published at https://jamanetwork.com