the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
November , 2023
This is an Executive Summary of the report “Advancing the frontier of health and technology integration”, published by the Economist Impact”, on November 2023, and authored by Maryanne Sakai.
The 2023 Digital Health Barometer [1]
Economist Impact, Supported by Roche
About this report
Advancing the frontier of health and technology integration: the 2023 Digital Health Barometer is a report by Economist Impact. It describes attitudes and research on digital health across ten countries: Australia, Brazil, France, Germany, Japan, Mexico, South Korea, Spain, the UK (insights from UK consider England, unless stated otherwise) and the US.
A literature search was performed to assess the landscape and to complement a search of grey literature that assesses governance structures and frameworks. In addition, a range of experts were interviewed, including policymakers, clinicians, academics and industry experts, and a field survey was conducted through Computer-Assisted Telephone Interview (CATI) and online among 100 patient consumers in each country. Respondents had all accessed healthcare services outside of primary care within the previous 12 months.
The research for this report was led by Maryanne Sakai, with research conducted by Anelia Boshnakova, Alcir Santos Neto and Ari Smith, and with contributions by Michael Guterbock and Amanda Stucke. This report was written by Adam Green and edited by Maria Carter.
Executive summary
Health systems around the world are embracing digital technology at every point in the patient journey, from consultation and diagnosis to treatment and monitoring, thanks to rapid improvements in capabilities such as artificial intelligence, connected devices, data analytics and digital therapeutics.
Such tools are promising given the rising burden of chronic diseases that healthcare systems are struggling to respond to in a cost-effective, equitable and sustainable way.
Disease management, continuous monitoring and tracking and behavioural interventions are critical interventions for conditions like heart disease, diabetes and cancer, in contrast to infectious diseases and acute emergencies, but modern health systems have not been built to handle the numbers of patients with these chronic conditions, according to Elgar Fleisch, professor of Information and Technology Management at ETH Zurich and the University of St Gallen.
Digital health technologies demonstrate value, but integrating them into health systems is challenging. Solutions are not always designed with the needs of clinicians and patients in mind, and the data and technology environment can become increasingly complex and fragmented.
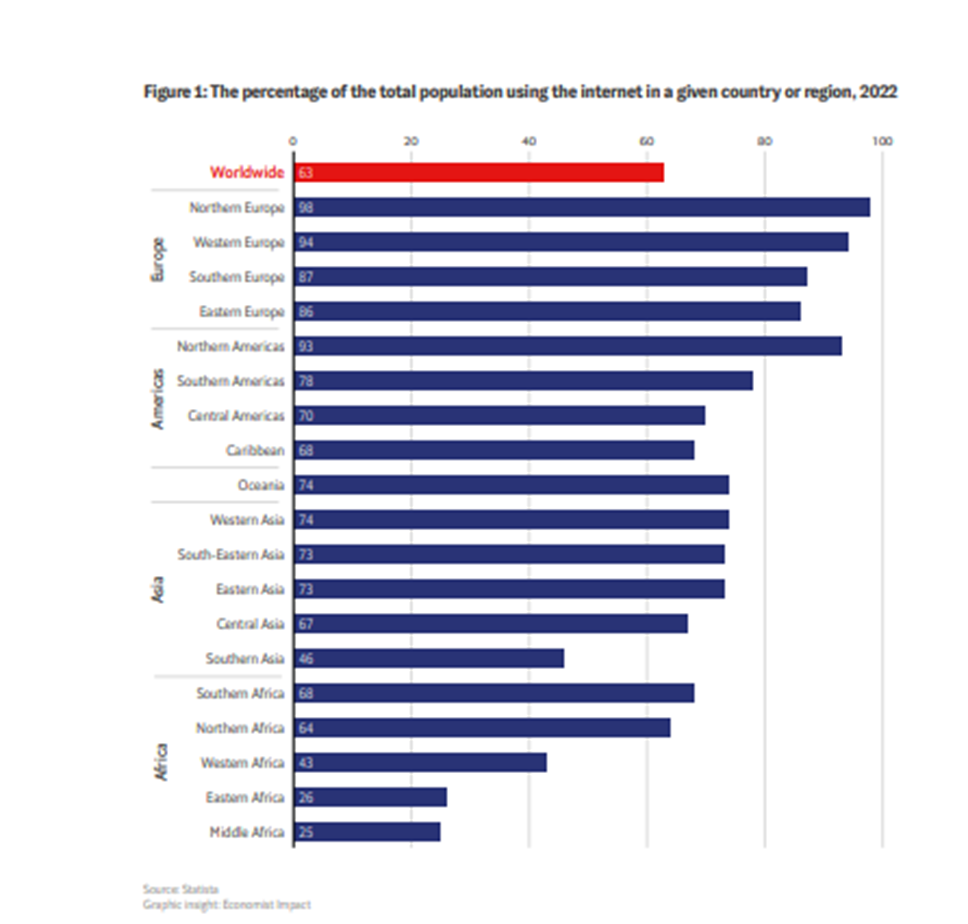
New approaches to clinical validation and regulatory approval are required, but these take time to develop. Socioeconomic inequalities, such as unequal internet access and varying levels of digital literacy, can mean that such disparities widen in the rush to roll out digital health solutions.
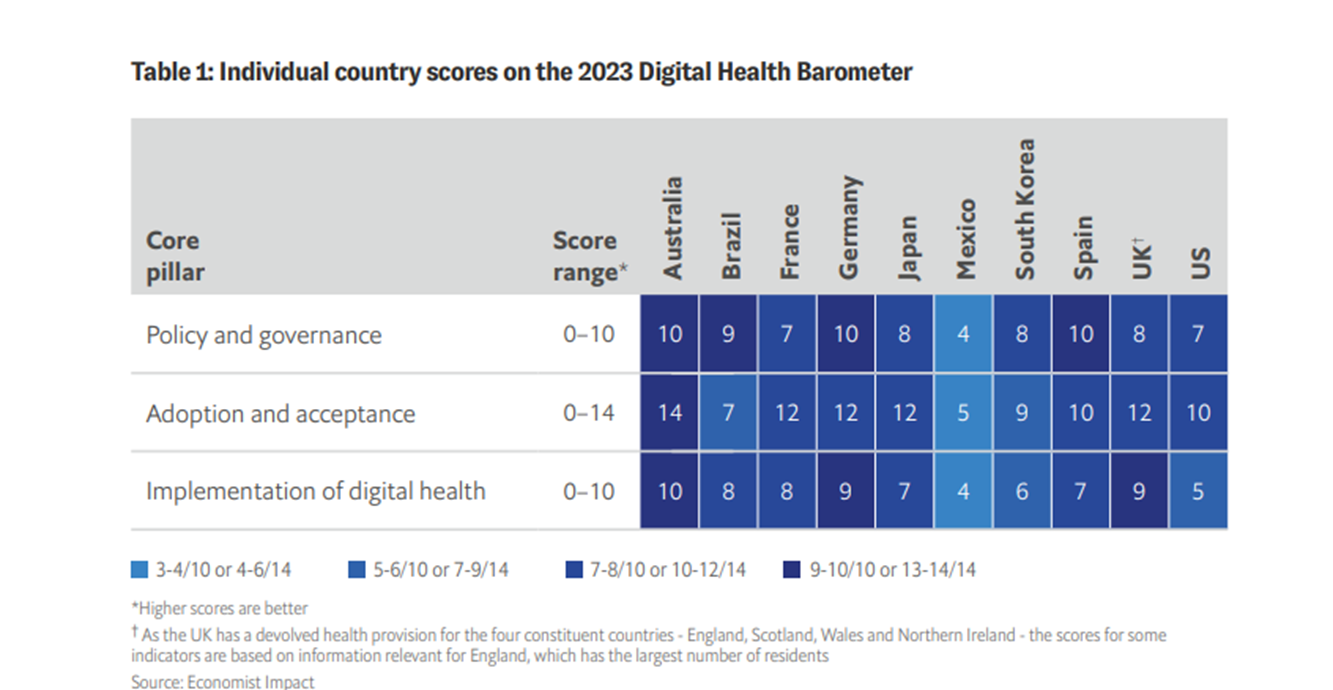
This Economist Impact white paper combined a ten-country barometer covering Australia, Brazil, France, Germany, Japan, Mexico, South Korea, Spain, UK and the US with a wide-ranging expert-interview programme to assess the enabling environment for digital health across economic, demographic and cultural contexts.
This barometer assesses national performance in the provision of key regulatory, institutional, policy and capability enablers for successfully adopting and deploying health technologies at scale.
Key findings from the research include [key points]:
- 1.Interoperability standards are in place across all but one of the ten countries,
- but only half of the countries have national-level electronic health record (EHR) systems.
- 2.All ten countries have regulatory foundations for enabling digital health,
- but do not comprehensively have robust assessments of digital health tools in place.
- 3.Digital health solutions are not always user-friendly or accessible for either clinicians or patients.
- 4.Digital health initiatives may widen social inequality.
- 5.Widening access to telehealth services, particularly in remote areas, should be a priority.
Infographic


Deep dive
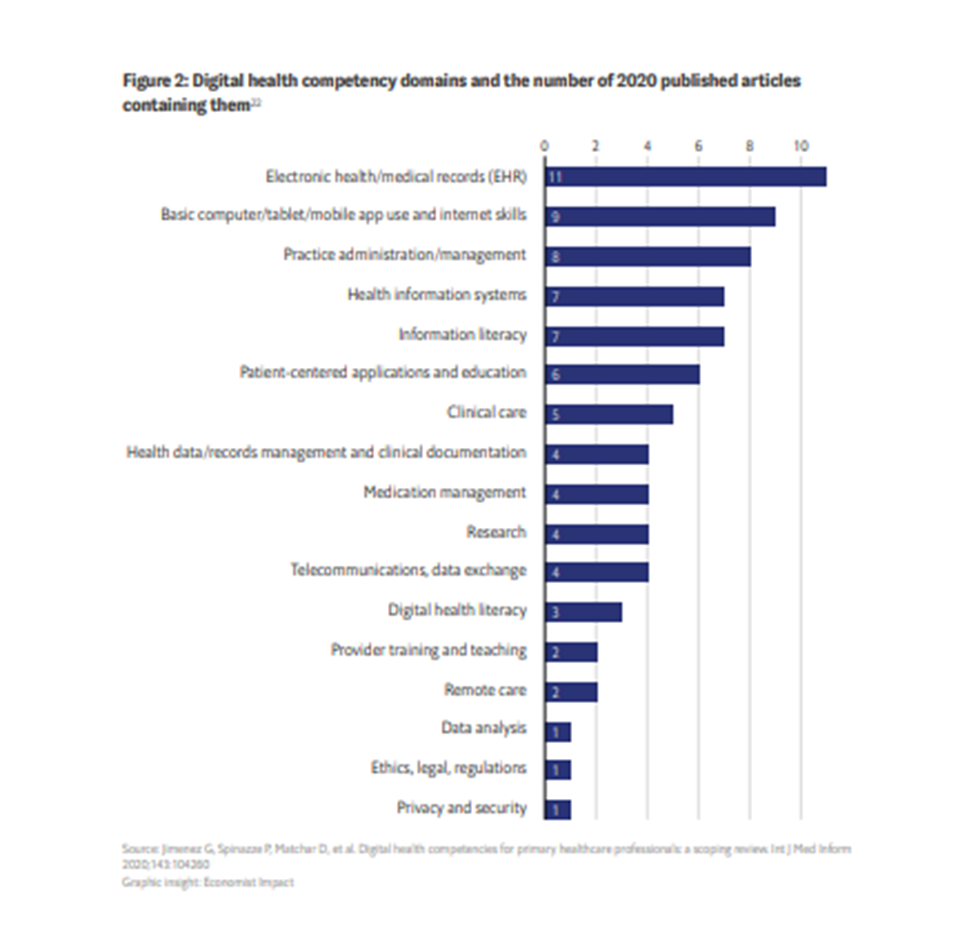
1.Inter operability standards are in place across all but one of the ten countries, but only half of the countries have national-level electronic health record (EHR) systems.
There has been strong progress in creating interoperability standards, but only half the countries score in the highest tier for EHRs, meaning that integration at a national level might be missing or fragmented.
Fragmented EHRs lead to greater inefficiency, complexity and costs and the increased potential for errors.
Further investment in EHRs will improve patient care and the productivity of healthcare providers, whereby medical professionals can access all of a patient’s important information to allow them to provide effective treatment in a timely manner.
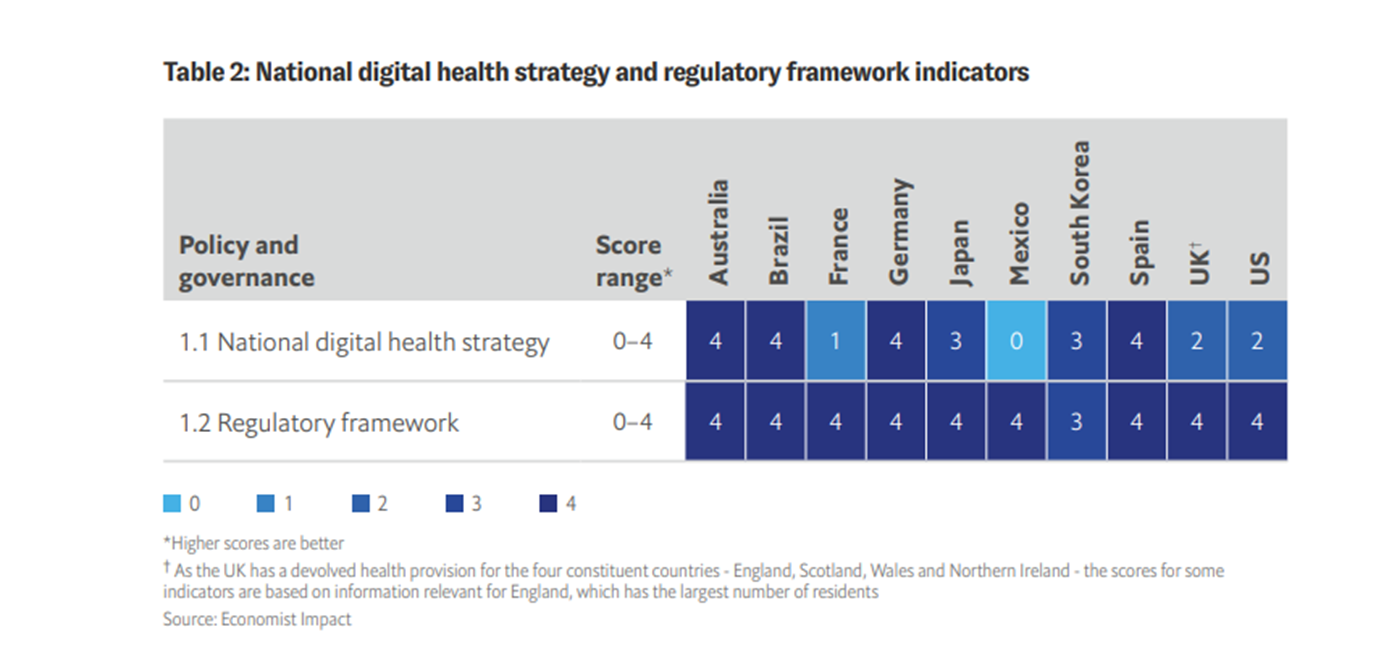
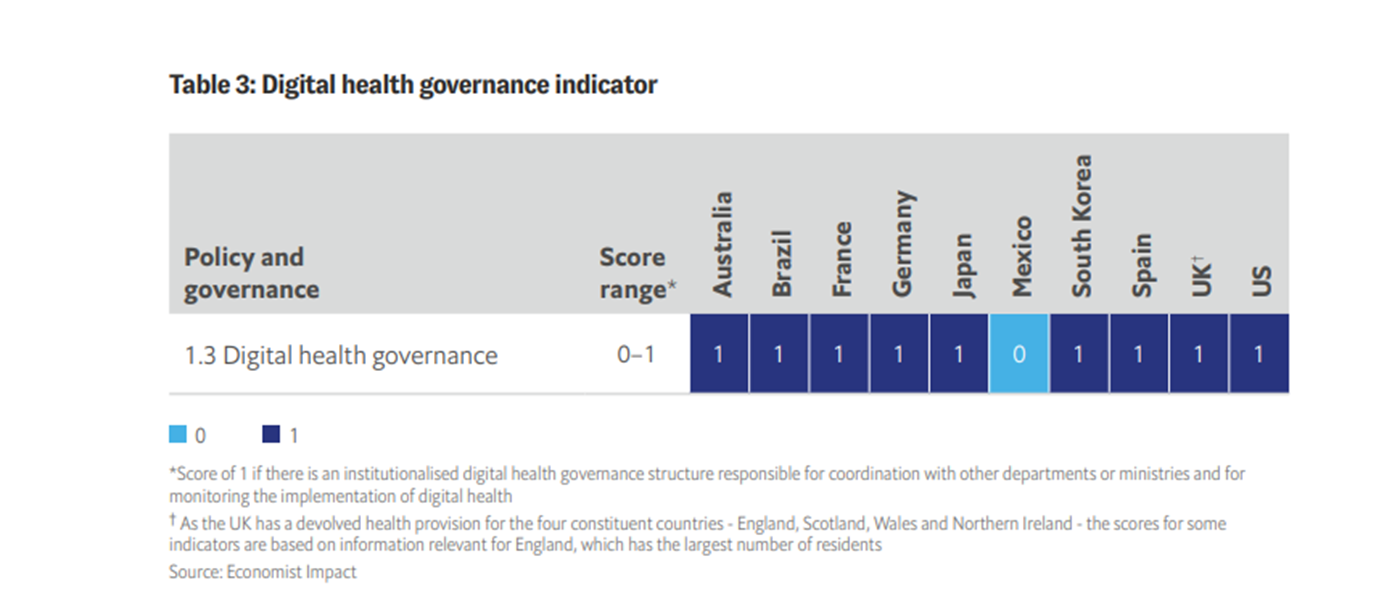
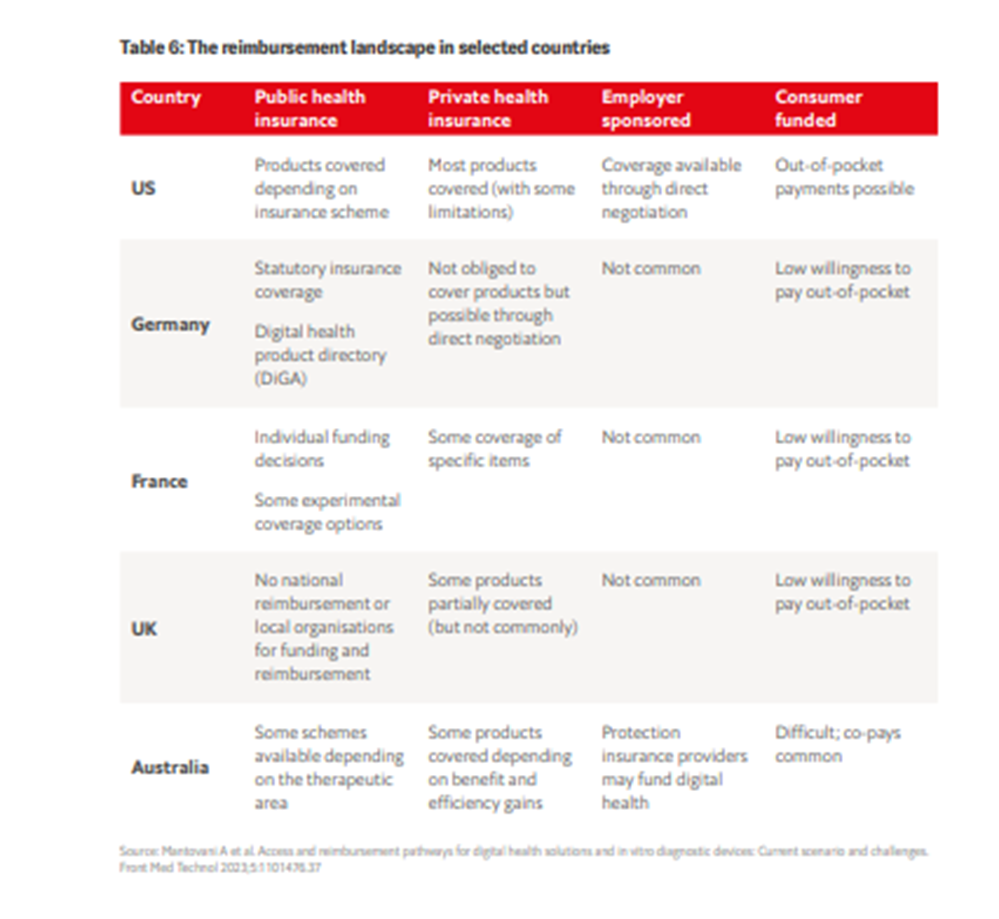
2.All ten countries have regulatory foundations for enabling digital health, but do not comprehensively have robust assessments of digital health tools in place.
As digital technologies proliferate, it is essential to have regulatory guidance and systems for upholding healthcare safety and quality.
On a positive note, the regulatory framework for digital health was the highest scoring indicator overall for the ten countries, showing the existence of comprehensive legislation for allowing electronic access to health data, governing the sharing of data, and protecting privacy.
However, four of the countries lack an established technology assessment mechanism for digital tools.
Modernised and adapted health technology assessments (HTAs) are essential for equipping consumers, practitioners and patients with the correct information to determine which tools are validated and proven.
3.Digital health solutions are not always user-friendly or accessible for either clinicians or patients.
Digital health tools must be aligned with the skills and training of the healthcare workforce, including cross-generational cohorts, and should be accessible to patients.
According to the expert interviewees, this is too often not the case; the onus should be on developers to ensure interfaces and tools can be used by everyone, including people with impairments.
Human factors must also be part of product design; rather than relying on technologies and algorithms alone, clinical judgement is required, based on human understanding.
Similarly, technologies should be tailored to the ecosystem that patients are familiar with.
4.Digital health initiatives may widen social inequality.
The use of digital technologies may, in the short term, increase inequalities associated with older age and lower educational attainment and socioeconomic levels. Health literacy is critical for tackling this divergence.
Only four out of the ten countries have digital health literacy programmes for patients and the general population or a national action plan or strategy on health literacy.
In Japan, for example, 71% of the surveyed population are not regular digital healthcare users, but about a third of them seem comfortable using technology to interact with health services.
The Japanese government delivers several activities for raising the public’s awareness and use of digital health; they provide a public relations flyer for patients and the general public describing how to use telemedicine services and explaining their advantages.
Japan also developed a specialised website with videos that promote the integration of health services. Internet access is constrained at a national level in Japan, as well as within other specific countries.
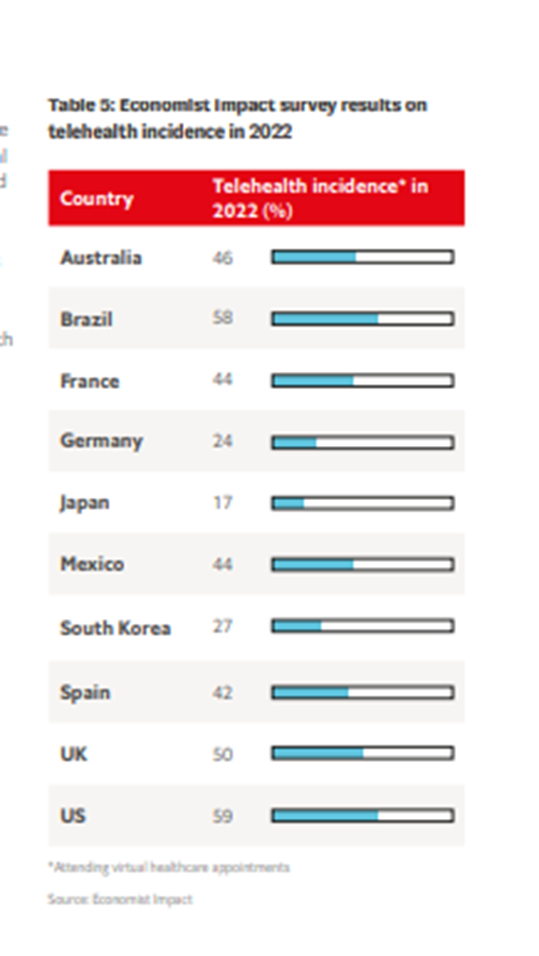
5.Widening access to telehealth services, particularly in remote areas, should be a priority.
Since the beginning of the covid-19 pandemic, national telehealth programmes have expanded, allowing patients to control more of their healthcare needs in a more flexible way.
Most of the countries have telehealth programmes for remote patient monitoring, but only four (Australia, France, Germany and UK) have implementation monitoring systems.
England, for example, has a programme for creating a commissioning environment that supports the use of technology to improve health outcomes and deliver more cost-effective services.
In addition to its focus on implementation, the NHS England Technology Enabled Care Services (TECS) measures and evaluates the service.
In Australia, priority has been given to widening access to health services in rural and remote areas, and the planning and evaluation of a permanent telehealth system is under development.
Contents of the report
· About this report
· Executive summary
· Chapter I: Digital health: a systems perspective
· Chapter II: Digital health: the road ahead
Names mentioned:
The research for this report was led by Maryanne Sakai, with research conducted by Anelia Boshnakova, Alcir Santos Neto and Ari Smith, and with contributions by Michael Guterbock and Amanda Stucke. This report was written by Adam Green and edited by Maria Carter.
We would particularly like to thank the following experts, listed in alphabetical order by country, who contributed through these interviews, in Brazil and in other countries.
Brazil
· Cesar Filho, co-founder and CEO of WeCancer
· Thiago Julio, medical director at Memed and director of technology at the Paulista Society of Radiology
[1] “Roche: Economist Impact report, Advancing the Frontier of Health and Technology Integration — The 2023 Digital Health Barometer highlights opportunities in digitalisation of healthcare.”












