Mayo Clinic
Aug. 12, 2022
Site editor:
Joaquim Cardoso MSc.
Health Transformation Institute
AI Health Care Review
September 5, 2022
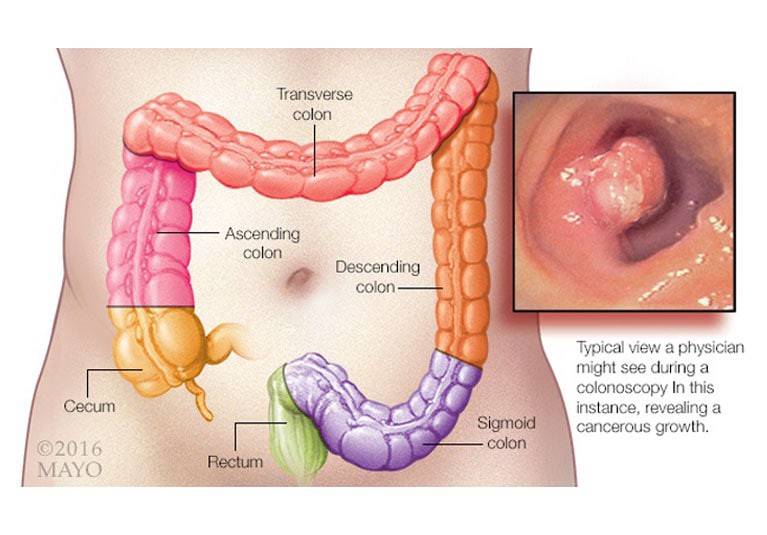
The most relevant cause of post-colonoscopy colorectal cancer (CRC) is the miss rate of colorectal neoplasia — the rate at which neoplastic lesions are not detected in a screening or surveillance colonoscopy.
Some studies suggest that 52% to 57% of post-colonoscopy CRC cases are due to missed lesions at patients’ colonoscopies. It’s estimated that 25% of neoplastic lesions are missed following screening colonoscopy.
Mayo Clinic Gastroenterology and Hepatology, in collaboration with colleagues from around the world, found that using artificial intelligence (AI) in colorectal cancer screening produced a 50% reduction in the miss rate for colorectal neoplasia.
Results of the study were published in the July 2022 edition of Gastroenterology.
“Colorectal cancer is almost entirely preventable with proper screening,” says senior author Michael B. Wallace, M.D., division chair of Gastroenterology and Hepatology at Sheikh Shakhbout Medical City in Abu Dhabi, United Arab Emirates, and the Fred C. Andersen Professor at Mayo Clinic in Jacksonville, Florida.
“The substantial decrease in miss rate using AI reassures health care providers on the decreased risk of perceptual errors.”
“Colorectal cancer is almost entirely preventable with proper screening,” …
“The substantial decrease in miss rate using AI reassures health care providers on the decreased risk of perceptual errors.”
A multicenter, multicountry study
This randomized control trial analyzed screenings of 230 patients, both men and women, with average risk for CRC.
All participants underwent screening or surveillance colonoscopies at one of eight facilities in three countries: Italy, the United Kingdom and the U.S.
Each participant underwent two same-day, back-to-back colonoscopies. One screening was conducted with and one without AI.
Patients were randomized into one of two arms.
The test arm received a colonoscopy assisted by AI first, followed by a colonoscopy without AI.
The control arm received a colonoscopy without AI first, followed by a colonoscopy assisted by AI.
Investigators conducting the screenings had a minimum of 1,000 completed colonoscopies and had an adenoma detection rate (ADR) between 20% and 40% or a polyp detection rate (PDR) between 30% and 70%.
A maximum of three endoscopists per study site participated, and each investigator had a maximum of 90 randomized patients to screen.
Miss rate reduced using AI
Adenoma miss rate (AMR) reflected the number of histologically verified lesions detected at the second colonoscopy divided by the total number of lesions detected at both colonoscopies combined.
In the test arm, the arm with AI first, AMR was 15.5%.
In the control arm, AMR was 32.4%.
The polyp miss rate (PMR) was 16.9% and 31.1% for the test group and control group, respectively.
When compared with the control arm, the test arm reported lower AMR for nonpolypoid lesions (16.8% for test arm and 45.8% for control arm) and lesions less than or equal to 5 millimeters (15.9% for test arm and 35.8% for control arm).
The test arm also had lower AMR for the proximal and distal colon than the control arm. False-negative rates were 6.8% in the test arm and 29.6% in the control arm.
“This computer-aided detection is highly accurate,” says Dr. Wallace. “With decreased miss rates, we can ultimately increase our detection rates, detect colorectal cancer more accurately and save more lives.”
“This computer-aided detection is highly accurate,” … “With decreased miss rates, we can ultimately increase our detection rates, detect colorectal cancer more accurately and save more lives.”
The AI device used in this study had shown a substantial increase in ADR in two previous randomized control studies.
This study indirectly validates that the ADR increase previously seen is specifically driven by reducing the miss rate risk.
Larger studies are needed to assess the possible decrease of AMR for advanced adenomas.
For more information
Wallace M, et al. Impact of artificial intelligence on miss rate of colorectal neoplasia. Gastroenterology. 2022;163:295
Gastroenterology and Hepatology. Sheikh Shakhbout Medical City. Mayo Clinic.
Originally published at https://www.mayoclinic.org.
ORIGINAL PUBLICATION (reference)
Impact of Artificial Intelligence on Miss Rate of Colorectal Neoplasia
Gastroenterology
Michael B. Wallace,1,2 Prateek Sharma,3 Pradeep Bhandari,4 James East,5 Giulio Antonelli,6,7,8 Roberto Lorenzetti,6 Micheal Vieth,9 Ilaria Speranza,10 Marco Spadaccini,6 Madhav Desai,4 Frank J. Lukens,1 Genci Babameto,11 Daisy Batista,11 Davinder Singh,11 William Palmer,1 Francisco Ramirez,12 Rebecca Palmer,5 Tisha Lunsford,12 Kevin Ruff,12 Elizabeth Bird-Liebermann,5 Victor Ciofoaia,11 Sophie Arndtz,4 David Cangemi,1 Kirsty Puddick,4 Gregory Derfus,13 Amitpal S. Johal,14 Mohammed Barawi,15 Luigi Longo,16 Luigi Moro,16 Alessandro Repici,17,18 and Cesare Hassan17,18
Received 14 January 2022, Accepted 4 March 2022, Available online 15 March 2022, Version of Record 20 June 2022.
1Division of Gastroenterology and Hepatology, Mayo Clinic Jacksonville, Florida
2Division of Gastroenterology, Sheikh Shakhbout Medical City (SSMC), Abu Dhabi, UAE
3Department of Gastroenterology and Hepatology, University of Kansas Medical Center, Kansas City, Kansas
4Division of Gastroenterology, Queen Alexandra Hospital, Portsmouth, UK
5Translational Gastroenterology Unit, John Radcliffe Hospital, Oxford, UK
6Gastroenterology Unit, Nuovo Regina Margherita Hospital, Rome, Italy
7Department of Anatomical, Histological, Forensic Medicine and Orthopedics Sciences, “Sapienza” University of Rome, Italy
8Gastroenterology and Digestive Endoscopy Unit, Ospedale dei Castelli Hospital, Ariccia, Rome, Italy
9Institut für Pathologie Klinikum Bayreuth GmbH, Bayreuth, Germany
10Cros NT, Verona, Italy
11Division of Gastroenterology and Hepatology, Mayo Clinic LaCrosse, LaCrosse, Wisconsin
12Division of Gastroenterology and Hepatology, Mayo Clinic Scottsdale, Scottsdale, Arizona
13Division of Gastroenterology and Hepatology, Mayo Clinic Eau Claire, Eau Claire, Wisconsin
14Division of Gastroenterology, Geisinger Medical Center, Danville, Pennsylvania
15Gastroenterology & Digestive Health, Ascension St. John Hospital, Detroit, Michigan
16Cosmo Artificial Intelligence-AI Ltd, Dublin, Ireland
17Department of Biomedical Sciences, Humanitas University, Rozzano, Milan, Italy
18Endoscopy Unit, Humanitas Clinical and Research Center IRCCS, Rozzano, Milan, Italy
Originally published at https://www.sciencedirect.com
Names mentioned:
Michael B. Wallace, M.D., division chair of Gastroenterology and Hepatology at Sheikh Shakhbout Medical City in Abu Dhabi, United Arab Emirates, and the Fred C. Andersen Professor at Mayo Clinic in Jacksonville, Florida.