the health strategist
institute of research and strategy
for continuous health transformation
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
August 14, 2023
What is the message?
Researchers from MIT and Dana-Farber Cancer Institute have developed the OncoNPC AI model, which accurately predicts the origin of tumors in patients with cancers of unknown primary (CUP).
By analyzing genetic sequences of about 400 genes, the model could potentially guide clinicians towards personalized treatments, increasing eligibility for targeted therapies and improving patient outcomes.
The original paper, “Machine learning for genetics-based classification and treatment response prediction in cancer of unknown primary”, has been published by Nature Medicine.
One page summary:
- Cancers of unknown primary (CUP) present a significant challenge in clinical oncology, as identifying the origin of these tumors is crucial for effective treatment selection.
- These cases, accounting for 3 to 5 percent of cancer patients, lack clear origin information, hindering precise treatment strategies that are typically tailored to specific cancer types.
- Addressing this issue, researchers from MIT and Dana-Farber Cancer Institute have developed an AI-powered computational model named OncoNPC, which utilizes machine learning to predict the origin of tumors by analyzing the genetic sequences of around 400 genes.
Key Findings:
- The OncoNPC model demonstrated the capability to accurately classify at least 40 percent of tumors of unknown origin within a dataset of approximately 900 patients.
- This classification provided a 2.2-fold increase in the number of patients who could potentially benefit from genomically guided, targeted treatments based on tumor origin.
- Successful predictions from the model could lead to the selection of precision treatments for patients with cancers of unknown primary origin, significantly improving patient outcomes.
Methodology:
- The researchers trained the model using genetic data from nearly 30,000 patients diagnosed with 22 known cancer types, sourced from institutions including Memorial Sloan Kettering Cancer Center, Vanderbilt-Ingram Cancer Center, and Dana-Farber.
- The model was tested on about 7,000 tumors with known origins and achieved a prediction accuracy of approximately 80 percent. For high-confidence predictions, accuracy rose to around 95 percent.
- For a set of about 900 CUP tumors, the model predicted high-confidence origins for 40 percent of cases.
- Comparison of the model’s predictions with germline mutations data revealed a strong alignment between the predicted cancer type and the type suggested by germline mutations, reinforcing the validity of the model’s predictions.
Clinical Implications:
- Survival time analysis of CUP patients supported the model’s predictions; patients with poor-prognosis cancer types had shorter survival times, while those with better-prognosis types exhibited longer survival times.
- Comparing treatment outcomes for patients who received targeted treatments based on oncologists’ assessments with the model’s predictions showed that treatments aligned with the model’s predictions led to better patient outcomes.
- The OncoNPC model identified an additional 15 percent of patients who could have received existing targeted treatments if their cancer type had been known, potentially expanding treatment options without requiring new drug approvals.
- The model’s predictions provide actionable insights for clinicians, guiding the selection of precision treatments that already exist and have proven efficacy.
Future Directions:
- The researchers aim to enhance the model’s prediction capabilities by incorporating other types of data, such as pathology images and radiology images, to provide a more comprehensive perspective of tumors.
- Integrating multiple data modalities could enable the model not only to predict tumor types and patient outcomes but also to recommend optimal treatment strategies.
- The research findings suggest the potential for significant advancements in personalized cancer treatment strategies, leveraging AI-driven models to guide clinicians in making informed and effective decisions.
DEEP DIVE

AI model can help determine where a patient’s cancer arose
Predictions from the OncoNPC model could enable doctors to choose targeted treatments for difficult-to-treat tumors
Anne Trafton | MIT News
August 7, 2023
Using machine learning, researchers at MIT and Dana-Farber Cancer Institute created a computational model that can analyze the sequence of about 400 genes and use that information to predict where a given tumor originated in the body (Image: iStock, MIT News)
For a small percentage of cancer patients, doctors are unable to determine where their cancer originated. This makes it much more difficult to choose a treatment for those patients, because many cancer drugs are typically developed for specific cancer types.
A new approach developed by researchers at MIT and Dana-Farber Cancer Institute may make it easier to identify the sites of origin for those enigmatic cancers. Using machine learning, the researchers created a computational model that can analyze the sequence of about 400 genes and use that information to predict where a given tumor originated in the body.
Using this model, the researchers showed that they could accurately classify at least 40 percent of tumors of unknown origin with high confidence, in a dataset of about 900 patients. This approach enabled a 2.2-fold increase in the number of patients who could have been eligible for a genomically guided, targeted treatment, based on where their cancer originated.
“That was the most important finding in our paper, that this model could be potentially used to aid treatment decisions, guiding doctors toward personalized treatments for patients with cancers of unknown primary origin,” says Intae Moon, an MIT graduate student in electrical engineering and computer science who is the lead author of the new study.
Alexander Gusev, an associate professor of medicine at Harvard Medical School and Dana-Farber Cancer Institute, is the senior author of the paper, which appears today in Nature Medicine.
Mysterious origins
In 3 to 5 percent of cancer patients, particularly in cases where tumors have metastasized throughout the body, oncologists don’t have an easy way to determine where the cancer originated. These tumors are classified as cancers of unknown primary (CUP).
This lack of knowledge often prevents doctors from being able to give patients “precision” drugs, which are typically approved for specific cancer types where they are known to work. These targeted treatments tend to be more effective and have fewer side effects than treatments that are used for a broad spectrum of cancers, which are commonly prescribed to CUP patients.
“A sizeable number of individuals develop these cancers of unknown primary every year, and because most therapies are approved in a site-specific way, where you have to know the primary site to deploy them, they have very limited treatment options,” Gusev says.
Moon, an affiliate of the Computer Science and Artificial Intelligence Laboratory who is co-advised by Gusev, decided to analyze genetic data that is routinely collected at Dana-Farber to see if it could be used to predict cancer type. The data consist of genetic sequences for about 400 genes that are often mutated in cancer. The researchers trained a machine-learning model on data from nearly 30,000 patients who had been diagnosed with one of 22 known cancer types. That set of data included patients from Memorial Sloan Kettering Cancer Center and Vanderbilt-Ingram Cancer Center, as well as Dana-Farber.
The researchers then tested the resulting model on about 7,000 tumors that it hadn’t seen before, but whose site of origin was known. The model, which the researchers named OncoNPC, was able to predict their origins with about 80 percent accuracy. For tumors with high-confidence predictions, which constituted about 65 percent of the total, its accuracy rose to roughly 95 percent.
After those encouraging results, the researchers used the model to analyze a set of about 900 tumors from patients with CUP, which were all from Dana-Farber. They found that for 40 percent of these tumors, the model was able to make high-confidence predictions.
The researchers then compared the model’s predictions with an analysis of the germline, or inherited, mutations in a subset of tumors with available data, which can reveal whether the patients have a genetic predisposition to develop a particular type of cancer. The researchers found that the model’s predictions were much more likely to match the type of cancer most strongly predicted by the germline mutations than any other type of cancer.
Guiding drug decisions
To further validate the model’s predictions, the researchers compared data on the CUP patients’ survival time with the typical prognosis for the type of cancer that the model predicted. They found that CUP patients who were predicted to have cancer with a poor prognosis, such as pancreatic cancer, showed correspondingly shorter survival times. Meanwhile, CUP patients who were predicted to have cancers that typically have better prognoses, such as neuroendocrine tumors, had longer survival times.
Another indication that the model’s predictions could be useful came from looking at the types of treatments that CUP patients analyzed in the study had received. About 10 percent of these patients had received a targeted treatment, based on their oncologists’ best guess about where their cancer had originated. Among those patients, those who received a treatment consistent with the type of cancer that the model predicted for them fared better than patients who received a treatment typically given for a different type of cancer than what the model predicted for them.
Using this model, the researchers also identified an additional 15 percent of patients (2.2-fold increase) who could have received an existing targeted treatment, if their cancer type had been known. Instead, those patients ended up receiving more general chemotherapy drugs.
“That potentially makes these findings more clinically actionable because we’re not requiring a new drug to be approved. What we’re saying is that this population can now be eligible for precision treatments that already exist,” Gusev says.
The researchers now hope to expand their model to include other types of data, such as pathology images and radiology images, to provide a more comprehensive prediction using multiple data modalities. This would also provide the model with a comprehensive perspective of tumors, enabling it to predict not just the type of tumor and patient outcome, but potentially even the optimal treatment.
The research was funded by the National Institutes of Health, the Louis B. Mayer Foundation, the Doris Duke Charitable Foundation, the Phi Beta Psi Sorority, and the Emerson Collective.
Article originally published at https://news.mit.edu
Original Publication
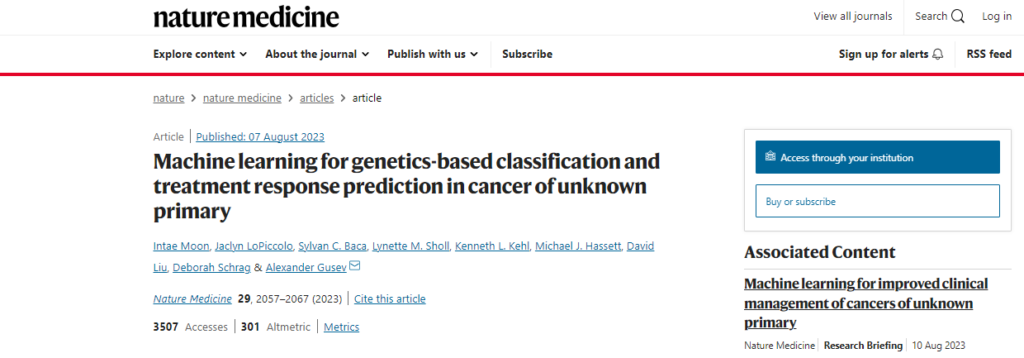
To access the original paper, published by Nature Medicine, access https://www.nature.com/articles/s41591-023-02482-6