Forbes
William A. Haseltine
October, 6th, 2021
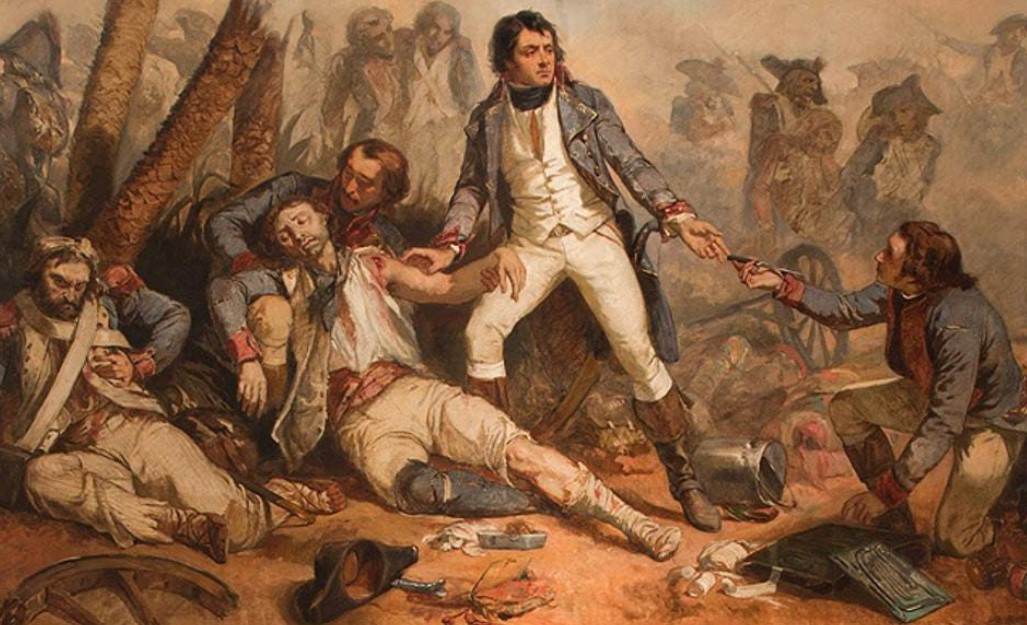
Painting by Charles-Louis Muller, showing famed French military doctor and surgeon, Dominique … [+].Académie Nationale de Médicine, Paris
American hospitals are once again at a breaking point, overwhelmed by Covid and forced to invoke crisis standards of care, where life-saving resources are rationed and distributed based not on need but on the likelihood of survival.
While this may seem, on paper, as a necessary evil, it is in reality the stuff of nightmares with life after life unnecessarily lost: A man in Alabama who died after bng turned away by 43 hospitals while in the midst of a cardiac emergency; a veteran in Houston who passed away because of a gallstone issue after waiting seven hours for an ICU bed; an Alaskan patient taken off dialysis and left to die because there weren’t any nurses available to staff the dialysis machines.
In practice, crisis standards of care are invoked only in times of overwhelming demand to help doctors and nurses prioritize care.
Typically, hospitals treat all patients on a first come, first served basis, with some minor arrangements made based on the severity of a patient’s illness and the urgency of their need — if you come to a hospital with a broken finger, you may wait longer than the patient in the midst of a heart attack, but eventually you and everyone else around you will be treated.
When there is a spike in demand for emergency care due to a crisis, providers have to triage patients and make tougher choices about who should receive life-saving care first.
All hospitals develop their own objective triage protocols, so that nurses and doctors don’t have to make the decision based on their own personal opinions.
The protocol differs from hospital to hospital, but most rely on a scoring system that assesses the performance of a patient’s key organ systems — neurologic, blood, liver, kidney — and the health of major organs like the brain or the heart to determine the likelihood of a patient’s survival.
If a major catastrophic event like a building collapse sends dozens of critical care patients to a hospital with only one operating room, the scoring systems can help providers determine who to send to the operating room first.
Let’s say two patients arrive at the same time, one who is clinically brain dead and has a less than 5% chance of survival, and the other with a fully functioning brain and a 30% chance of survival.
The scoring system can help doctors and nurses decide where to focus resources to save the most lives possible. Not an easy decision, but a critical one in moments of crises.
What makes the Covid-19 crisis unique is its scope and durability.
Most crises are acute, the result of a single, catastrophic event like a tornado, hurricane or major explosion.
A hospital by hospital protocol may indeed be sufficient in moments like those, when the scope of the crisis is relatively limited.
When crisis standards of care are invoked statewide, as they are today, it is a grim admission that the entire health system is overwhelmed.
When the system is overwhelmed in its entirety for so long, new challenges emerge:
- At what point should statewide crisis standards of care be invoked?
- Once invoked, how can you provide care equitably across the system, when some populations in poorer, under-resourced neighborhoods bear a disproportionate burden of disease?
- How can you be sure that patients across the system are being treated equally across all hospitals, instead of having each hospital triage care based on different standards or scoring systems?
- How can hospitals across a state share resources and the burden of care most effectively, to at least mitigate the effects of the surge?
This is the first article in a series that will discuss each of these questions in detail.
As we explore possible solutions, it’s important to remember that while hospitals and healthcare providers have long had to make tough decisions about how to prioritize care in the face of disasters, the idea of standardizing these protocols is very new.
- In the United States, it was only formally considered by the federal government in 2009, as another virus, H1N1, was threatening to spread across the country.
The Department of Health and Human Services asked the Institute of Medicine to develop guidelines for allocating medical resources in times of crisis and scarcity.
Their report, published later that year, included guidance for state and local public health officials to develop comprehensive policies and protocols for standards of care.
It laid out a vision of crisis standards of care that was based on fairness, equitable processes, community and provider engagement, and the rule of law.
… the vision of crisis standards of care … is … based on fairness, equitable processes, community and provider engagement, and the rule of law.
- In the years that followed, other organizations like the American College of Chest Physicians published additional recommendations based on their understanding of crisis standards applied in practice.
- But it wasn’t until Covid-19 that the cracks in these crisis standards really emerged, exposing how extensively some states had failed to implement the guidance and laying bare the structural inequities in our healthcare system.
Instead of implementing a structured and steady response in the face of the alarmingly high Covid-19 surge in demand, many hospitals and statewide healthcare systems were thrown into chaos, scrounging for much needed equipment, forced to turn parking lots into patient treatment centers, and asking doctors and nurses to work around the clock to manage the surge, leaving many of them “ depressed, disheartened, and tired to the bone “.
- The National Academy of Medicine recently released a new set of recommendations for implementing crisis standards of care, just as Idaho was considering invoking them statewide.
As we dive into the recommendations in more detail throughout this series, there is one critical lesson that rises to the fore: we never should have let it come to this.
Just last summer we were writing and talking about all these same challenges, as Arizona became the first in the pandemic to invoke the crisis standards statewide.
When SARS-CoV-2 first emerged, it naturally took all of us here in the United States and around the world by surprise.
Few among us had a sense of what we were up against, though there were a select few scientists — myself among them — who raised early warnings about the type of damage coronaviruses in general and this one in particular could cause. Still, it is at least understandable why the size of those early waves of infection took us by surprise.
These more recent waves that are now submerging states like Alaska and Idaho can be blamed on no one but ourselves, and our failure to implement the strategies — mandated vaccines, masking, testing, tracing and quarantine — that we know already can slow the pandemic and reduce cases to manageable levels.
That we have failed to do so is a mark of shame on all of us.
As we explore ways to prepare our hospitals to manage the surge in demand, we must also do better to improve our own individual approaches to this pandemic. In the end, it is not just the doctors and nurses who are choosing between who will live and who will die, but rather each of us.
About the author

In Dr. Haseltine’s career at the forefront of medical research and application, he has educated a generation of doctors at Harvard Medical School, designed the strategy to develop the first treatment for HIV/AIDS, is well known for his groundbreaking work on cancer, and led the team that pioneered the development of new drugs based on information from the human genome. His relentless focus on delivering world-changing results led TIME magazine to name him one of the “25 Most Influential Global Business Executives.”
Today, as the Chair and President of ACCESS Health International and an internationally recognized expert on the COVID-19 pandemic, Dr. Haseltine is dedicated to ensuring that quantum advancements in medical technology translate to improved health outcomes around the world.
Dr. Haseltine has founded more than a dozen biotechnology companies, including Human Genome Sciences, Inc. Eight pharmaceutical products from companies he founded are currently approved by U.S. and international regulatory agencies. He is the author of more than two hundred peer reviewed manuscripts and eleven books, including two books on COVID: A Family Guide to Covid and A Covid Back to School Guide. His most recent book, My Lifelong Fight Against Disease: From Polio and AIDS to COVID-19, was published in October 2020. He is currently chair and president of the global health think tank ACCESS Health International.
Originally published at https://www.forbes.com.