The Lancet, Case Study
Adriano Massuda
with Ana Maria Malik, Gabriela Lotta, Marina Siqueira, Renato Tasca, Rudi Rocha
WORKING PAPER 1
JANUARY 2022
CONDENSED VERSION
Edited by Joaquim Cardoso MSc.
The first part of this post contains a condensed version of the report, reproducing the content of four sections: (1) Executive Summary; (2) Introduction; (5) Discussion and (6) Conclusions.
The second part of this post contains the excerpts of the main sections of the original publication (the methodology for example, was not reproduced here, and can be found on the full version of the original publication)
Executive Summary
Since Brazil’s 1988 federal constitution approved guidelines to restore democracy, expand social rights and define health as a universal right and government responsibility, the country has undergone profound economic, social, demographic, and epidemiological transformations.
Throughout the 1990s, the Unified Health System (Sistema Único de Saúde — SUS) was implemented, decentralizing federal funds and responsibilities to municipalities and states.
In 1998, the Family Health Strategy (FHS), designed in 1994, was adopted as a national model to expand health services across the country.
Economic growth and the prioritization of social policies in the 2000s enabled FHS coverage to be scaled-up, improving access to health services and health outcomes. However, these achievements are currently under threat.
As part of the health system reforms in the 1990s, innovative financing arrangements for PHC were established to underpin the FHS scale-up.
A specific federal funding mechanism for PHC, the Floor for Basic Care (Piso da Atenção Básica — PAB), was created in 1996 and implemented in 1998.
Composed of a fixed per-capita component based on municipal population and a variable component linked to federal priorities, the PAB channelled monthly, regular, and automatic federal resources to all municipalities for delivering PHC services.
Improvements to PAB arrangements were made over time to encourage municipalities to adopt the FHS model, to enlarge the scope of PHC services delivered, and to address health inequalities.
A number of studies point to the effectiveness of the FHS in improving access to healthcare, reducing social inequalities and improving health outcomes including declines in infant mortality, preventable hospitalisations and avoidable mortality.
Recent studies also show the benefits of FHS in reducing racial inequalities and protecting against the effects of the latest economic crisis in 2015.
However, to support scaling up of the FHS, total government health expenditure increased, with the financial burden falling mainly on municipalities.
As municipalities took on regular payments for PHC services, without adequate support from state governments, imbalances in the allocation of resources were exacerbated, especially in the distribution of doctors.
These challenges have increased since the economic and political crisis began.
In 2016, austerity measures were introduced followed by restrictive reforms in PHC policies.
Risk-adjusted capitation was introduced to replace the PAB mechanism, which, despite its issues, had been fundamental for creating stability in PHC financing, threatening the achievements obtained.
Capitation can be a valuable enhancement of the financing mechanisms for PHC in Brazil if it is integrated with the successful PAB scheme in a blended model.
Introduction
Brazil has developed one of the largest and most innovative Primary Health Care (PHC) systems in the world. The Family Health Strategy (FHS), a community-based delivery model established through the Unified Health System (Sistema Único de Saúde — SUS), enabled the rapid scaling-up of PHC coverage in an upper middle-income country of continental size with widespread inequalities. Whilst the FHS has had positive effects on health outcomes, several problems remain unresolved. Understanding how health financing arrangements underpinned the successful expansion of FHS as an essential part of Brazil’s health system reform, and the challenges that they continue to face, can offer valuable lessons for other low- and middle-income countries (LMIC) which are aiming to move towards Universal Health Coverage (UHC).
Initially focused on deprived regions in the early 1990s, the Ministry of Health (MoH) decided in 1998 that the FHS should become the organisational model for expanding access to healthcare through the SUS for the whole country. Federal funds were created and channelled directly to municipalities to encourage the adoption of the FHS model, following arrangements to support health system decentralisation. Between 1998 and 2020, the number of FHS teams grew from 2,054 to 43,286, reaching an estimated 133.7 million people (63.6% of Brazilians). To support the expansion of health services delivery, including PHC, overall government spending has increased, with municipalities carrying the greatest share of the financial burden. By using multi-professional teams to provide a comprehensive range of services to populations in a defined geographic area, the FHS model contributed to a shift in how healthcare services are delivered in Brazil. Composed of a doctor, a nurse, one or two nurse assistants and up to twelve community health workers (CHW), the level of FHS coverage in municipalities was associated with positive effects: increased access to healthcare, improved health outcomes, and reduced social and racial health inequalities.
However, despite its role in improving health system performance, FHS still faces several challenges. Scaling-up of the FHS has been uneven among municipalities and, despite reaching more than 98% of all Brazilian municipalities in 2020 (5,485 out of 5,570), the level of FHS coverage varies widely across regions. Gaps in performing the PHC functions also remain, including difficulties in accessing services, the highly variable quality of care, and a lack of integration within health systems networks. Further, since the country entered a challenging economic and political crisis in 2015, significant barriers to expansion of FHS and improving its performance have arisen. In 2016, restrictive reforms in PHC policies were established in line with long-term fiscal austerity policies, threatening the achievements obtained.
In this study, we employed a mixed-method approach using document analysis and in-depth interviews with key informants, as well as quantitative analysis of government data, to explore how health financing arrangements created through the SUS underpinned the expansion of PHC in Brazil. We also discuss how challenges in health system financing, governance, resource allocation and in management capacities at the municipal level have shaped the PHC model across the country.
5. Discussion
To our knowledge, this is the first study that used a mixed-method approach, combining data analysis, interviews with key actors, and reviewing official documents to explore the historical development of the SUS financing arrangements and its effects on the FHS scaling up in Brazil.
Our analysis suggests new elements in understanding how government financing mechanisms underpinned the FHS expansion in Brazil, the progress achieved, and unresolved challenges.
Findings related to the research questions
The political context of strengthening democracy, economic development, and social progress in Brazil enabled the development of national policies to ensure a sustained advance towards UHC between 1990 and 2015.
Scaling-up of the FHS occurred in this environment with significant financial and political commitment from the federal government and implementation the responsibility of municipalities.
Our findings highlight that this lay at the core of the reform of Brazil’s health system.
Having a PHC model in place “shovel-ready” meant that the additional financing translated into rapid scaling-up of the FHS.
The fiscal space generated from economic growth at the time, as well as the politics, were both important factors behind the increase in PHC spending.
The population-based resource allocation mechanism, which provided financial incentives to encourage the adoption of the FHS, created an important financing arrangement for driving the change.
PAB replaced the fee-for-service reimbursement to providers, which had previously concentrated resources in wealthier regions, and spread federal resources to all municipalities to expand the provision of PHC services, with relatively greater benefits for those in deprived areas.
Additionally, our findings emphasise how driving federal funds to public managers underpinned an active role for municipal governments in managing the health system, which together with a steady flow of federal funds for PHC, created a resilient way of delivering community-based PHC services.
However, despite the successful scaling-up, fragilities in the financial arrangements and the unresolved problems of the SUS left inequalities largely unchanged.
Although the PAB variable component encouraged scaling-up of the FHS in regions where public need was greatest, this expansion was funded largely by rises in municipal own resources amid a chronic federal underfinancing of the SUS.
Our findings show that the rise in per-capita health expenditure overall was faster in wealthier municipalities.
Since municipal governments had to take on regular payments for PHC services, including medical staff, the financial inequalities between municipalities exacerbated imbalances in the allocation of resources, particularly doctors.
Our findings also show that despite the proportion of PAB-transfers reducing over time, correlations between PAB-transfers and input/outcome indicators are substantially stronger compared with correlations between municipal funding and the same indicators.
This fact highlights the crucial role of federal resources in encouraging the FHS model, which achieved remarkable results.
Overall, on average, federal transfers have been relatively less important as a source of funding for municipal health services, PHC included, but the marginal funding allocated through federal mechanisms has had the greatest impact.
On the other hand, our findings evidence fragilities in the financing arrangements with tensions between decentralised responsibility and federal standards, which limited innovation and local responsiveness.
Aiming to increase PHC coverage rapidly with the same model, it reduced the flexibility of the composition of the FHS team, compromising its capacity to adapt to the wide diversity of social, cultural, epidemiological, and demographic realities, hindering quality assurance.
In addition, we observed that federal initiatives to address FHS challenges — management support, performance assessment, uneven distribution of doctors, and crucially, integration into regional networks — have had limited impact due to other health system fragilities.
Overall, the mix of financing arrangements, designed and channelled through federal transfers and directed to municipalities, has never targeted goals other than FHS scaling-up, and improvements in coverage and quality of services at the municipal level.
As a result, coordination of actions and policies between municipalities, within regions, and integration of PHC services into a more structured and coordinated grid of mid- and high-complexity services have been limited.
Finally, all these arrangements are currently under revision with likely adverse consequences.
Despite the need to improve financing arrangements to address PHC challenges, the substitution of PAB-transfers by capitation and performance assessment is risky for several reasons.
Firstly, in a widely unequal continental-size country, with a health system decentralised to the municipal level, the PAB arrangement was crucial for creating a stable source of funds for PHC and to drive the implementation of the FHS model. Losing it may provoke undesirable fluctuations in PHC financing.
Secondly, if not supported by the MoH, the registration of the population and assignment to FHS teams, as well as the recording of performance indicators, are not easy tasks. This is particularly worrisome among municipalities in deprived regions, which typically lack state capacity and rely relatively more on federal transfers. Its effects are likely to reverse gains in reducing health inequalities between municipalities that had been achieved by the expansion of FHS.
Thirdly, despite the eventual benefits of adopting capitation to encourage FHS teams to be held accountable by the people they assist, its implementation as a substitute for PAB, in a context of economic crisis and long-term austerity measures, may serve to limit the provision of PHC services by the constrained resources. As a result, the recent changes proposed in financing arrangements for PHC are likely to jeopardise the universal and comprehensive character of the FHS model, which ought to be the major impetus for the reform of Brazil’s health system.
Findings related to the existing literature
Our findings draw attention to how financial arrangements established to expand UHC in Brazil encouraged the scaling up of FHS, contributing to improvements in access and health outcomes, with relatively more benefits to those in deprived areas.
Positive effects of FHS were associated with a reduction in social inequalities, avoidable hospitalizations, infant- and amenable mortality causes (Hone et al., 2017[1]; Macinko et al., 2010[2]; Dourado et al., 2011[3]; Ceccon et al., 2014[4]; Macinko et al., 2006[5]; Aquino et al., 2009[6]; Rocha and Soares, 2010[7]; Rasella, 2013[8]; Macinko and Lima-Costa 2012[9]; Lima-Costa et al., 2013[10]; de Santiago et al., 2014[11]).
It is in line with the overall literature, which shows that the strengthening of PHC systems is associated with improvements in health outcomes and an equitable distribution of these better outcomes (Starfield et al., 2005[12], Macinko et al., 2009[13]; Kruk et al., 2010[14]; Bitton et al., 2019[15]).
However, PHC financial arrangements had limitations. The FHS was implemented in Brazil with substantive regional differences.
This contrasts with the experiences of PHC in high-income countries, developed as the effective basis for health systems (Friedberg et al., 2010[16]; Starfield, 2010[17]; Kringos, 2013[18]).
Persistent health inequalities in Brazil, enhanced by a dual public-private health system, was a critical obstacle not only to FHS expansion, but also for undermining the PHC functions in the SUS, such as coordination of access to the health system (Andrade et al., (a) 2018[19]; Andrade et al., (b) 2018)[20].
Our study also highlights some consequences of the recent economic and political crisis and fiscal austerity measures, aggravating the chronic federal underfunding of SUS, and changing PHC financing arrangements.
The literature describes a cascade of events triggered by restrictive fiscal policies that weakened PHC systems and led to citizens foregoing healthcare.
Consequently, there is an increase in unmet health needs, in the use of emergency services, and in preventable hospitalization and avoidable mortality (Karanikolos et al., 2013)[21].
The restriction of federal health funds and the deregulation of PHC policies are rapidly deteriorating the role of PHC in the health system in Brazil.
As reported by the literature, progress achieved by the FHS expansion is under threat (Camargo et al., 2020[22]; Vieira, 2020[23]; Melo et al., 2020[24]; Melo, Mendonça and Teixeira, 2019[25]; Melo et al., 2018[26]).
Finally, in a review of PHC financing arrangements in Brazil, the obstacles reported in the scant literature (Silva, 2017)[27] agree overall with the challenges that emerged from our in-depth interviews with key informants.
It is worth mentioning that the national and international literature includes few studies describing the complexity of challenges, factors, and implications of implementing financing mechanisms and policies to strengthen PHC (Angell, 2019[28], Goodyear-Smith et al., 2019[29]; Silva, 2017[30]).
There is little country-specific evidence of PHC financing in low- and middle-income countries (Goodyear-Smith et al., 2019)[31].
Aspects relevant to other settings
Brazil’s experience with financing PHC can offer valuable lessons for other LMIC settings.
The political will to provide universal and comprehensive healthcare was a major driver for creating financial arrangements for scaling up a resilient FHS model.
In contrast with many other LMIC, PHC in Brazil, inspired by the UK’s National Health Service, was developed to be the basis of health system and not a vertical or separate programme.
Establishing financial transfer to local managers closer to where people live and targeted at PHC, was a successful strategy for fostering political commitment to spreading the delivery of PHC services.
Population-based mechanisms were essential for creating stability and predictability for public managers to invest in PHC, while financial inducements directed the implementation of the FHS.
In this decentralized system, the MoH played a vital role in coordinating national policy and municipalities were crucial for delivery.
The deficiencies of the arrangement also can provide lessons.
Federal health budget constraints led to a disproportional increase in municipal health financing, which created further inequalities in the allocation of resources, such as doctors. This situation was aggravated by the lack of participation by state governments in PHC management, as well as poor health system regional governance.
Attempts to create financial incentives to improve FHS performance and to integrate PHC into health networks both failed. If such attempts only redirect resources, without adding new funds, not only are they unlikely solve the problems, but they can also create other problems. This serves as a warning to the current government about its initiative of replacing the PAB with risk-adjusted capitation.
Limitations
Our study has some limitations. First is the time frame. The decision to look at the period 1990–2015 limits the analysis of factors that preceded the changes and what occurred after 2015. Although some of these previous elements were covered in the interviews, the decision to analyse the restricted period is justified because this was the moment of greatest change to the SUS. It is also justified by the availability of data.
Second is the limited scope of the collected data. The interviews were conducted with only 13 respondents. However, to reduce the problems with data bias, we made the interviews as representative as we could. In addition, the data were all triangulated between document analysis, interviews, and quantitative data. Third, our quantitative results also face limitations. Coefficient estimates of linear regressions should not be interpreted as causal but reveal correlational patterns between municipality spending, its baseline determinants, and their potential consequences in terms of PHC coverage, access to health services, and health outcomes. Besides, we used administrative data in our analysis, which might have been under-reported, potentially leading to attenuation bias in our estimates.
6. Conclusion
Implementing a universal and comprehensive health system in a country with widespread inequality was a major achievement in Brazil.
Influenced by the political impetus to restabilize democracy and increase social rights, and inspired by creative municipal experiences in different regions of the country which sought to overcome adversity, the Family Health Strategy was applied nationwide.
The FHS used financing arrangements that combine federal incentives, composed of fixed and variable components, with municipal resources.
The model showed an efficient and effective way to improve access and health outcomes, especially for the poor, serving as an example of innovation for Latin American and other low-income countries.
However, unresolved structural problems in Brazil, which remains one of the most unequal democracies in the world, and the fragilities of the health system have limited the reach of the FHS.
Financing arrangements were not robust enough to face challenges such as imbalances in the allocation of health professionals, the poor quality of some PHC provision, the need to introduce innovative health technologies and to integrate better with health networks.
Looking ahead, as a prolonged economic and political crisis unfolds in the country, dramatically exacerbated by the COVID-19 pandemic, replacing the successful PHC financing model by simply redirecting the existing resources according to new criteria, is foolhardy.
The PAB was an arrangement that, despite its issues, was fundamental for creating stability in PHC financing.
In moments of crisis, such as the current COVID-19 pandemic, the need for a consistent financing scheme for PHC is crucial.
Capitation can be a valuable enhancement of the financing mechanisms for PHC in Brazil if it is integrated with the successful PAB scheme in a blended model.
Health inequalities are already increasing rapidly, mainly affecting that part of the Brazilian population which benefited most from the Family Health Strategy over the past two decades. These setbacks should not be ignored but reversed, in order to continue to support the fabric of society.
ORIGINAL PUBLICATION (Excerpted version)

Brazil’s Primary Health Care Financing — Case Study @ The Lancet
The Lancet, Case Study
Adriano Massuda
with Ana Maria Malik, Gabriela Lotta, Marina Siqueira, Renato Tasca, Rudi Rocha
WORKING PAPER 1
JANUARY 2022
Table of contents (TOC)
- Introduction
- Background
- Methods
- Findings
- Discussion
- Conclusion
References
1.Introduction
Brazil has developed one of the largest and most innovative Primary Health Care (PHC) systems in the world. The Family Health Strategy (FHS), a community-based delivery model established through the Unified Health System (Sistema Único de Saúde — SUS), enabled the rapid scaling-up of PHC coverage in an upper middle-income country of continental size with widespread inequalities. Whilst the FHS has had positive effects on health outcomes, several problems remain unresolved. Understanding how health financing arrangements underpinned the successful expansion of FHS as an essential part of Brazil’s health system reform, and the challenges that they continue to face, can offer valuable lessons for other low- and middle-income countries (LMIC) which are aiming to move towards Universal Health Coverage (UHC).
Initially focused on deprived regions in the early 1990s, the Ministry of Health (MoH) decided in 1998 that the FHS should become the organisational model for expanding access to healthcare through the SUS for the whole country. Federal funds were created and channelled directly to municipalities to encourage the adoption of the FHS model, following arrangements to support health system decentralisation. Between 1998 and 2020, the number of FHS teams grew from 2,054 to 43,286, reaching an estimated 133.7 million people (63.6% of Brazilians). To support the expansion of health services delivery, including PHC, overall government spending has increased, with municipalities carrying the greatest share of the financial burden. By using multi-professional teams to provide a comprehensive range of services to populations in a defined geographic area, the FHS model contributed to a shift in how healthcare services are delivered in Brazil. Composed of a doctor, a nurse, one or two nurse assistants and up to twelve community health workers (CHW), the level of FHS coverage in municipalities was associated with positive effects: increased access to healthcare, improved health outcomes, and reduced social and racial health inequalities.
However, despite its role in improving health system performance, FHS still faces several challenges. Scaling-up of the FHS has been uneven among municipalities and, despite reaching more than 98% of all Brazilian municipalities in 2020 (5,485 out of 5,570), the level of FHS coverage varies widely across regions. Gaps in performing the PHC functions also remain, including difficulties in accessing services, the highly variable quality of care, and a lack of integration within health systems networks. Further, since the country entered a challenging economic and political crisis in 2015, significant barriers to expansion of FHS and improving its performance have arisen. In 2016, restrictive reforms in PHC policies were established in line with long-term fiscal austerity policies, threatening the achievements obtained.
In this study, we employed a mixed-method approach using document analysis and in-depth interviews with key informants, as well as quantitative analysis of government data, to explore how health financing arrangements created through the SUS underpinned the expansion of PHC in Brazil. We also discuss how challenges in health system financing, governance, resource allocation and in management capacities at the municipal level have shaped the PHC model across the country.

2. Background
Innovative financing arrangements for PHC were established following health system reforms in 1998. The FHS was adopted as the organisational model for achieving UHC through the SUS across the country (Melamed & Costa, 2003[1]; Marques & Mendes, 2003[2]; Macinko & Harris, 2015[3]; Amorim & Mendes, 2020[4]). Extensive literature has shown that FHS expansion positively affected health system performance (Dmytraczenko & Couttolenc, 2013[5]; Barreto et al., 2014[6]; Bastos et al., 2017[7]; Macinko & Mendonça, 2018[8]). There is a need to investigate how SUS financing arrangements underpinned scaling up of the FHS, as well as how weaknesses in the arrangements and unresolved problems in the health system might affect further development of FHS and threaten its sustainability (Giovanella et al. 2009[9]; Paim et al., 2011[10]; Gragnolati, M. et al., 2012[11]; Cecilio & Reis, 2018[12]; Castro et al., 2019[13]).
In a political context of restoring democracy and civil rights after two decades of military dictatorship, the new health system principles designed by the Health Reform Movement (Escorel, 1999)[14] were approved during the VIII National Health Conference, held in 1986 and endorsed by the 1988 Constitution (Brazil, 1988)[15]. Health was established as a citizen’s right and government responsibility forming the basis for a universal, comprehensive, and decentralised health system, open to community participation and to private sector initiatives (Paim et al., 2011)[16]. After 30 years of SUS implementation, the scaling-up of the FHS contributed to Brazil achieving nearly universal access to healthcare services for the population (Castro et al., 2019)[17]. The increase in FHS coverage was associated with improving access to healthcare and reducing social inequalities (Macinko & Lima-Costa 2012[18]; Lima-Costa et al. 2013[19]; de Santiago et al. 2014[20]; Andrade et al. 2015[21]). It was also associated with significant declines in infant mortality (Macinko et al. 2006[22]; Aquino et al. 2009[23]; Rocha and Soares, 2010[24]; Rasella et al., 2013[25]), in avoidable hospitalisations (Macinko et al. 2010[26]; Dourado et al. 2011[27]; Ceccon et al. 2014[28]), and in amenable mortality, which is avoidable with timely and effective health care (Hone et al. 2017)[29]. Recent studies also show the benefits of FHS in reducing racial inequalities in healthcare (Hone et al., 2017[30]) and protecting against the effects of the latest economic crisis in Brazil (Hone et al., 2019[31]).
Despite the positive results of the FHS, many challenges remain, mainly due to the unresolved structural and organisational problems of Brazil’s health system. The political context that enabled the approval of SUS principles in the late 1980s changed rapidly in the early 1990s (Santos, 2018)[32]. The lack of political consensus to establish sufficient source of funds for the SUS led to chronic federal underfunding and unequal use of available resources (Arretche, 2003[33]; Uga & Santos, 2007[34]; Funcia, 2019[35]).
The fiscal space generated from sustained economic growth during the 2000s enabled an increase in health expenditure: from 2000 to 2018, total health expenditure grew from 8.3% to 9.5% of GDP and health expenditure per capita rose from U$ 321,50 to U$ 848,40. However, during this time, more than 58% of total health spending remained as private expenditure, concentrated among less than 25% of the population, and less than 42% was public funds to finance the SUS. Between 1990 and 2017, the share of total government health expenditure by municipalities increased from 12% to 31.1%, while the federal share decreased from 73% to 43.2%, and the states increased from 15% to 25.7% (Table 1).
Table 1: Trends in health expenditure in Brazil, 1990 to 2018
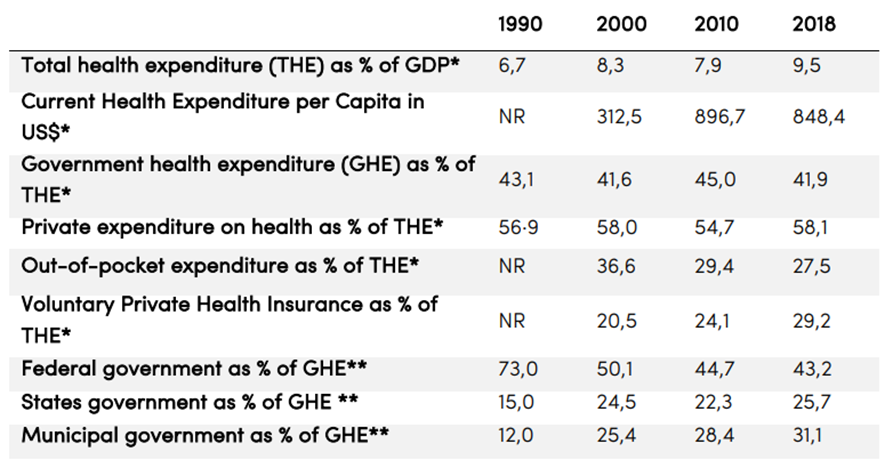
Sources: *WHO’s Global Health Expenditure Database that uses National Health Accounts (NHA) categories; **1990 from Medici & Marques, 1994; 2000=2003, 2018=2017 — from Piola, Benevides & Vieria, 2017.
In parallel with SUS implementation, voluntary private health insurance (VPHI) was developed to circumvent bottlenecks in access to specialized outpatient and hospital care, resulting in dual coverage (Almeida et al., 2000)[36]. Between 2000 and 2015, when the country was experiencing economic growth, the population with private health insurance grew from 30 million to 50 million, reaching about 24% of Brazilians. However, since 2015 three million people lost their insurance when unemployment increased during the economic crisis. About 70% of beneficiaries receive private health insurance as an employment benefit. Thus, the population covered by VPHI is mainly concentrated in larger municipalities and wealthier regions, while small and poor regions have almost no coverage (Massuda et al., 2020)[37].
Despite a lack of new sources of federal funding to enable universal access to health care, the MoH initiated the SUS implementation and created financing arrangements to support decentralisation in the early 1990s. Organisational rules were established to transfer federal funds to state and municipal governments who were given the responsibility of managing service provision (Viana et al., 2002)[38]. This process created a new set of relationships between government levels. While federal funding encouraged municipalities to take responsibility for managing the provision of services, the federal government also undertook an active and regulatory role by establishing funding for specific programmes linked to evaluation and control mechanisms (Levcovitz et al. 2001[39]; Castro & Machado, 2010[40]).
As part of health system decentralisation, a specific federal fund for PHC called PAB (Piso da Atenção Básica — Floor of Basic Care) was implemented in 1998. The PAB replaced the existing fee-for-service reimbursement mechanism for walk-in procedures performed at the PHC level, which had led to the concentration of federal funding for health in the wealthiest regions. Composed of a fixed per-capita component based on the municipal population, and a variable component linked to federal priorities, the PAB channelled monthly, regular, and automatic federal resources to all municipalities for delivering PHC services. Therefore, the provision of services gradually increased over the whole country. Municipalities in deprived regions, which had previously lacked health infrastructure to receive federal resources through reimbursement, benefited the most (Vianna et al. 2002[41]; Costa & Pinto 2002[42]).
The variable PAB component also played a fundamental role in encouraging municipalities to adopt the FHS model with funding linked to the number of FHS teams implemented in each municipality (Mendes & Marques, 2014[43]; Pinto, 2018[44]). When FHS scale-up began in 1998 there were differences in geographic coverage. Andrade et al. (2018)[45] show that the size of the municipal population had an inverse correlation with initial FHS coverage and expansion over time: municipalities with a smaller population reached a higher level of coverage faster than more populous ones. Given the FHS design, each FHS team should cover up to 4,000 people. According to IBGE, in 2020, 22.5% of Brazilian municipalities had less than 5,000 inhabitants (1,253 out of 5,570), and 68.1% had less than 20,000 inhabitants (3,786 out of 5,570), requiring one to five FHS teams to reach 100% of FHS coverage respectively.
On the other hand, FHS incentives were less attractive in more populous municipalities as they required municipalities to hire a much larger number of professionals and there were alternative models of PHC services, with a higher percentage of the population covered by private health insurance. According to Andrade et al. (2018)[46], the dual health system in Brazil is an important obstacle to FHS expansion and undermines its role in the SUS. In larger cities, middle- and high-income classes use the private sector to access a larger network of services, while low-income groups may also have access to private insurance through employment benefits.
Although PAB transfers played a crucial role in driving the scale-up of the FHS model, municipalities were responsible for co-financing PHC services, for providing the infrastructure and medical products, as well as for contracting professionals. According to a national SUS accounts study (2018), between 2010 and 2014, municipalities accounted for the largest proportion of PHC funding (61% of total), followed by the federal level (33% of total) and the states (6% of total).
However, given the high inequalities across the country, the significant increase in municipal health expenditure required to compensate the federal underfinancing had implications for the health system development. Municipalities had wide disparities in financial, administrative, and technical capacities to manage the SUS and provide PHC services. Wealthier municipalities were able to attract qualified health staff by offering better salaries and working conditions, while the poorest and the rural areas had more difficulty in attracting and retaining qualified health professionals, especially doctors, which became one of the hardest challenges for expanding the FHS (Lucchese, 2003[47]; Girardi et al. 2011[48]; Duncan & Targa, 2014[49]).
Changes were implemented in PHC policies and auxiliary programmes were created by the MoH in an attempt to address some of these FHS challenges. Implemented in 2006, the National Policy for PHC (Política Nacional de Atenção Básica — PNAB) was revised in 2011, introducing new compositions of FHS teams for targeting specific population groups. Different per-capita values for calculating the fixed PAB component were also implemented, based on socioeconomic vulnerability of municipalities (Gomes et al., 2020)[50]. However, the difference in per-capita amount ranged only from R$ 18.00 to R$ 23.00 when implemented, with only limited increases in the actual amount of money transferred to the poorest regions.
Also created in 2011, the Program for Access and Quality Improvement (Programa de Melhoria do Acesso e da Qualidade da Atenção Básica — PMAQ) aimed to evaluate and reward the good performances of FHS teams. Even though the programme contributed to a reduction in socioeconomic inequalities through improved performance of PHC providers, large disparities persisted (Kovacs et al, 2021)[51]. Created in 2013 to tackle the imbalance in the distribution of doctors, the More Doctors Programme (Programa Mais Médicos) placed 18,240 doctors in 4,058 municipalities. Although substitution for existing PHC doctors was observed (Hone et al., 2020)[52], the programme led to a reduction in preventable mortality, with greater benefits in municipalities prioritised where doctor density was low before the programme was implemented (Özçelik et al., 2020)[53].
In these challenging times, PHC is at a crossroads in Brazil (Massuda et al., 2018)[54]. Since 2015, SUS structural weaknesses have been aggravated by changes in the country’s economic and political context. In 2016, in response to the economic downturn, the government in place after Dilma Rousseff’s impeachment implemented severe fiscal austerity policies. Constitutional Amendment 95, passed by the Congress, froze federal spending for the next 20 years, limiting the increase in government spending on health and others social policies (Souza et al., 2018[55]; Rocha et al., 2021[56]).
In this context of austerity, the PNAB was reviewed in 2017 introducing new compositions of FHS teams and reducing the number and weekly workload of health professionals (Melo et al., 2018[57]; Gomes et al., 2020[58]). In 2019, a new policy for financing PHC in the SUS, Prevent Brazil (Previne Brasil), replaced the PAB arrangement. The payment was based on the number of citizens registered for FHS teams, adjusted by a criteria for socioeconomic vulnerability. Financial incentives were also created based on payment-for-performance for the teams. Some stakeholders and researchers have expressed concern about its restrictive purpose (Massuda et al., 2020[59]; Melo et al., 2020[60]) and the potential effects of increasing inequality, supported by detailed forecasts at a time of health budget cuts (Rasella et al., 2018[61]; Castro et al., 2019[62]). Due to the COVID-19 pandemic, the implementation of Prevent Brazil, which was planned for 2020, has been postponed.

3. Methods
See the original publication!

4. Findings
Based on the concept of restoring democracy and expanding civil and social rights, the 1988 Federal Constitution approved the SUS’s organisational guidelines and established a new set of relationships between the three levels of government in Brazil. Decentralization of health system management responsibilities, from federal to municipal governments, was supported by the creation of innovative funding transfer mechanisms, which encouraged municipalities to expand PHC services and adopt the FHS. As a result, municipalities have not only assumed a leading role in expanding provision of PHC services across the country, but also increased their participation in financing the health system. Figure 1 provides analysis of key policies, programmes and instruments, and their implications for the health system and for PHC.
Figure 1: Key policies, programmes and instruments and implications for the SUS and PHC
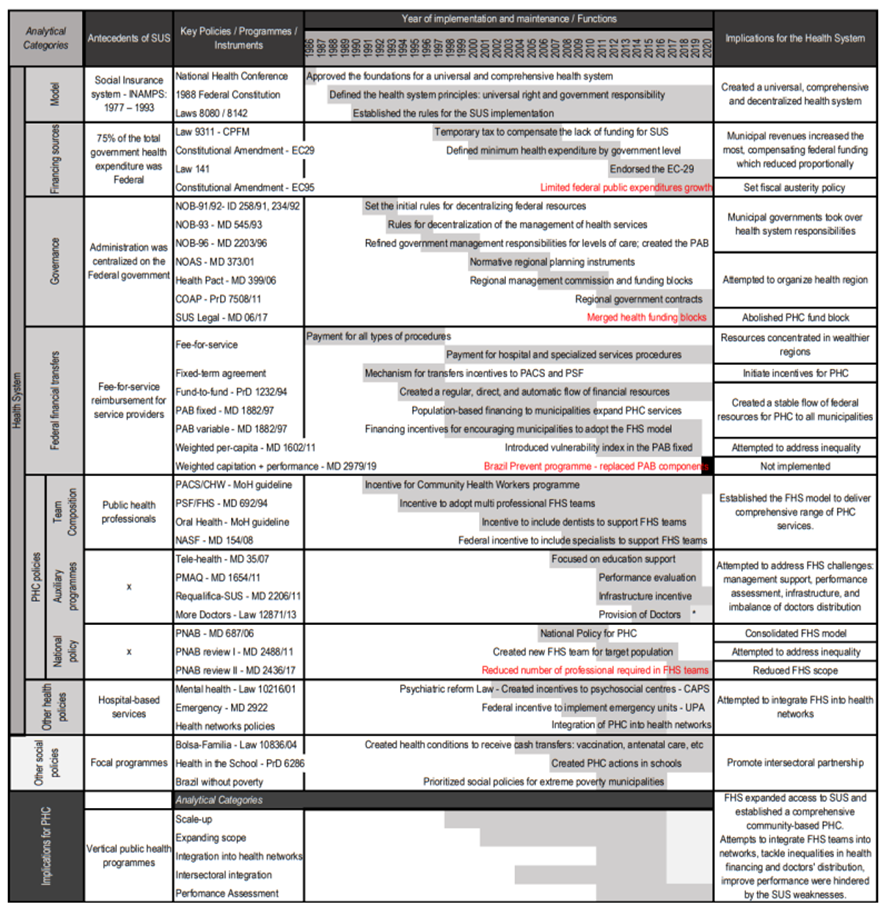
Source: Authors´ own work Notes 1: ID = INAMPS Decree; MD = MoH decree; PrD = Presidential decree; IMD = interministerial decree; * Notes 2: Measures implemented under fiscal austerity context marked in red.
Antecedents
Before SUS, the public social insurance system (INAMPS — Instituto Nacional de Assistência Médica da Previdência Social), which was centrally coordinated by the Federal government, offered emergency, specialized outpatient and hospital services to workers in the formal economy — an estimated of 34.2 million people (22.8% of the population) in 1988 (Cardoso, 2006)[1]. The payment mechanism from the federal government to providers linked to INAMPS was mainly through fee-for-service reimbursement, resulting in a concentration of financial resources in wealthier regions that had more capacity to provide health services. The uninsured population, and those with no resources to pay for medical services out-of-pocket, were treated as destitute in charity hospitals. Municipalities played a minor role in the health system, with a focus on offering vertical public health programmes, mainly targeting infectious diseases and mother-and-child care.
Between the 1960s and the 1980s, the Federal government established public health initiatives to provide healthcare services to impoverished communities in rural areas, including the public health visitors programme (visitadores sanitários) provided by the Special Public Health Service (Serviço Especial de Saúde Pública — SESP). The programme began to offer simple primary care for the population of a geographic area, influencing the Health Reform Movement, as mentioned by one interviewee:
[I9] Although there were management issues, the public health workers’ visits and guidance to families were of a high standard. This and other public health interventions, developed during the military dictatorship, gave the health sector a new dynamic, whose motto was to offer a simpler primary care closer to the population. These experiences were decisive for the health reform movement and the VIII National Health Conference in 1986.
On the other hand, community health experiences that were developed by some municipalities during the end of the 1970s and 1980s and influenced by concepts of Community Medicine, enabled the creation of new models of care and a new organization of teams in PHC settings, in a context of increasing politicization in society. This is described by one interviewee:
[I12] PHC, called Basic Health Care, was the setting for rethinking the biomedical dominance of the health model and an instrument for increasing the social and political consciousness of health workers and communities.
[I12] We had the autonomy to organise multi-professional teams, mixing the clinical and public health perspectives. The programmatic model of public health proposed by Johns Hopkins was combined with the community medicine perspective and actions for community education, inspired by Paulo Freire’s theory.
[I12] Many health professionals, including health visitors and nurses, came from the Liberation theology movement.
Experiences in the public health programmes, the first municipal attempts at PHC developed in partnership with universities, and the Alma-Ata declaration, all influenced the National Commission for Health Reform. The Commission discussed the need for a national institution to organize decentralized health networks. Primary Health Care was named Basic Health Care (Atenção Básica em Saúde) by the Health Reform movement, to emphasize the concept of being the basis of a universal and comprehensive health system.
However, PHC financing mechanisms lagged behind. The reform of the health system in Brazil was designed by a social movement and approved in the Constitution as part of major political changes in the country. Despite some members of the reform movement being MoH staff (Davidian, 2021)[2], the full implementation of SUS never became a major government priority. This explains the gap between the concept of the reform and the lack of federal funding for the SUS, and consequently for PHC, as mentioned by one interviewee:
[I2] It took a long time to have more substantial financial support for PHC, despite its presence in the governmental discourse since the national 1988 Constitution.
The SUS implementation
Decentralization of funds and responsibilities
After the 1988 Constitution approved the new health system principles, laws 8.080 and 8.142 established the organisational rules for implementing the SUS in 1990. More details about the main policies, programmes, and instruments of the health system and PHC development, the context of their implementation, and implications for FHS design are in Appendices 2 and 3.
In a context of scarce federal funding for the SUS, Ministerial decrees (Normas Operacionais Básicas — NOB) from 1991 to 1996 regulated the decentralization of federal transfers and health system responsibilities mainly to the municipalities and to the states. Initiating the decentralization in 1991, the NOB-91 created categories for municipalities to undertake health system management responsibilities with the role of service providers to the federal government. However, it caused confusion and was widely criticized by local managers, as mentioned by one of the interviewees:
[I6] NOB 91 positioned states and municipalities as service providers to the federal government and created prerequisites for municipalization. The categories created were poorly understood by local managers.
In 1993, the NOB-93 abolished these categories, turning all municipal governments into managers of the provision of services. This measure was important to encourage the participation of municipalities beyond the perspective of being simply providers.
And in order to support health system decentralization, in 1994 the Decree 1.232 established an innovative fund-to-fund mechanism for the Federal Government to transfer resources regularly and automatically from the national health fund to state and municipal funds. It made federal transfers more agile and sustainable over time.
As part of the health system municipalization, in 1996 the NOB-96 refined financing arrangements and management responsibilities for the three government levels for different levels of care, including PHC. It also established the first source of financing for PHC, the PAB (Piso da Atenção Básica — Basic Care Floor).
Funds for expanding service delivery
The creation of the PAB
Composed of fixed and variable components, the PAB was a source of financing established by the MoH specifically for PHC for municipalities. As mentioned by an interviewee, the central idea of the PAB was to engage municipalities in assuming responsibilities for expanding health coverage, despite knowing that some of them could not provide healthcare at that time:
[I2] To engage municipalities in health — a sector that brings many challenges and disproportional [lesser] electoral recognition — it was also necessary to assign more resources directly to the public manager. Therefore, despite the complex implementation of the NOB-96, it aimed to strengthen the financing of the municipal public manager.
[I2] Looking at the available infrastructure of the public system, the conclusion was that the most effective way to expand and direct resources and to engage states and municipalities across the country in health would be through PHC.
[I2] The flow of resources to all municipalities, including those without the ability to address problems, was the price to pay to engage all public managers at the municipal level with the SUS — enabling significant expansion of PHC coverage and population access.
Due to the lack of political consensus, both in the federal government and with the representatives of state and municipal health secretaries (CONASS and CONASEMS) regarding the per-capita value of its fixed component, the PAB was only implemented in 1998. Table 4 shows the values used to calculate the PAB fixed and variable components from 1998 to 2020.
Table 4: Values for PAB fixed and variable components: 1998–2020
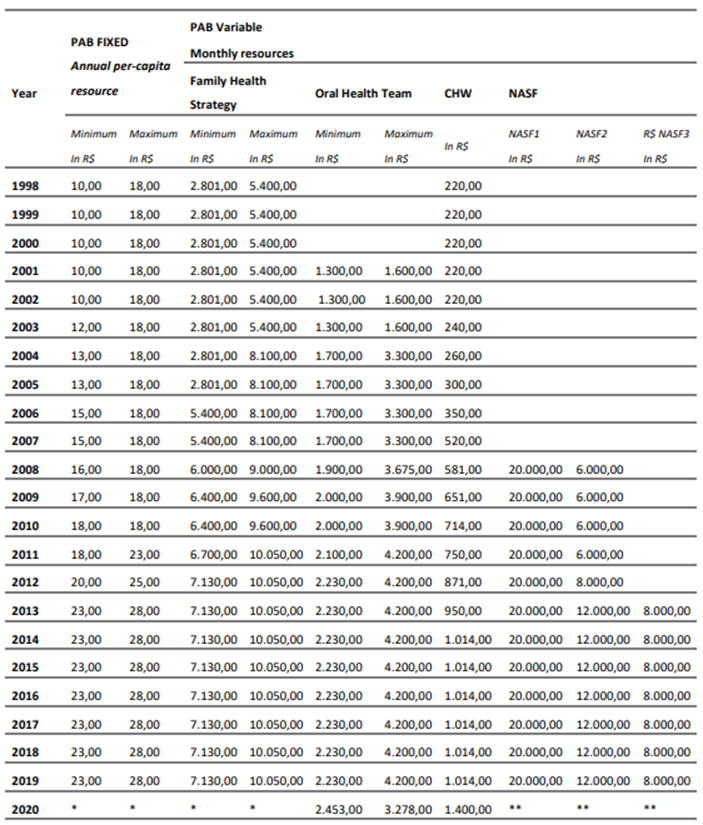
Note 1: Data adapted from Klitzke, 2021. Not adjusted for inflation. Note 2: A small group of municipalities which had a historical series of higher delivery of PHC procedures than was defined by the per-capita amount, and would consequently lose resources, as compensation a higher per-capita of R$ 18.00 was adopted. This value, however, was not increased, so that by 2010 it was equal to the minimum value. Note 3: *Replaced by the Prevent Brazil Programme; ** Abolished by the Prevent Brazil Programme.
Table 5 shows the values and percentage of PAB-transfers as part of the federal fund-to-fund transfers from 2000 to 2018. During this period, federal fund-to-fund transfers to states and municipalities grew from R$ 23.4 billion to R$ 82.2 billion, at 2018 values. Of those, 71.2% were transferred to municipalities. The percentage of PAB-transfers was 24.3% of the total federal fund-to-fund transfers and corresponded to 34.2% of the federal fund-to-fund transfers received by municipalities.
Table 5: Federal fund-to-fund transfers and percentage of PAB: 2000–2018
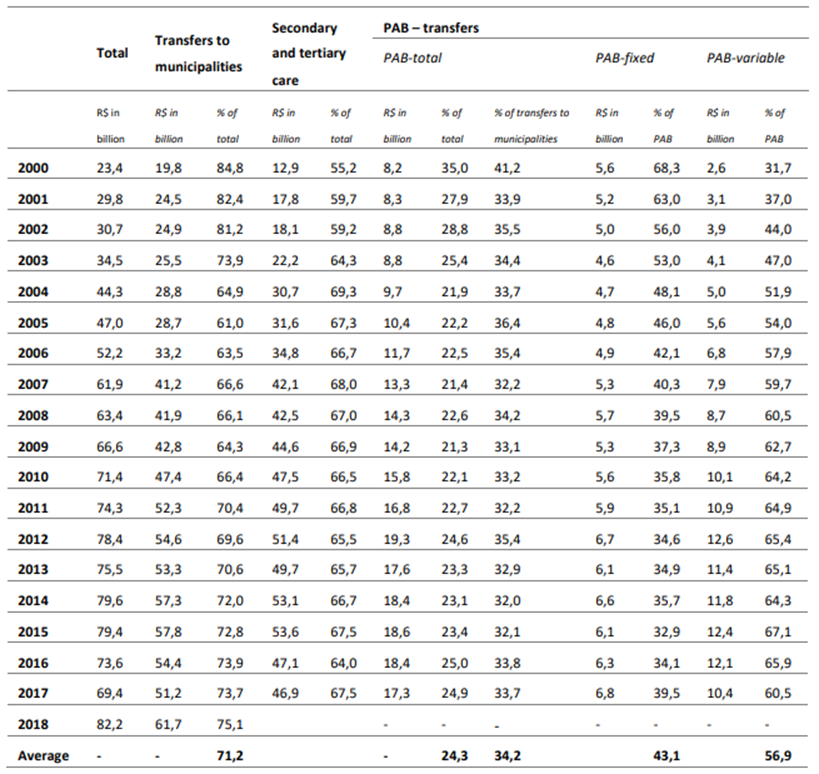
Note: data originally from National Health Fund/MoH at 2018 values (IPCA rate). The fund-to-fund transfers correspond to about 70% of the MoH’s budget. They are composed of resources for PHC, secondary and tertiary care, among others, channelled directly to states and municipalities. Given changes in the rules of federal transfers, the PAB values were not specified by the National Health Fund database in 2018.
A stable source of funds for PHC: PAB-fixed component
The population-based component of the PAB was drawn from federal resources and channelled to municipalities for the exclusive purpose of delivering PHC services. The per capita amount was initially set at R$ 10.00/year, based on the average previously paid through reimbursement for walk-in procedures in PHC services. The amount transferred to municipalities was calculated by multiplying the per-capita value by the population of each municipality and was paid monthly to the health fund of municipal governments.
The federal transfer through the PAB to municipalities enabled the maintenance of regular spending by the MoH on PHC, which ensured the continuity of PHC service delivery, even with fluctuations in political priorities at the local level. Although it was the same amount for the whole country, the PAB-fixed component produced relatively greater benefit for the smaller cities and in the poorest regions, which did not previously have health infrastructure to deliver services and receive reimbursement and, consequently, had little access to federal funds for healthcare. Further, the cost of providing PHC services, which is mainly composed of the salaries of health professionals, is usually less expensive in small municipalities, except for doctors, meaning that the same amount of funding has a greater impact in these areas (Sampaio & Lima, 2002)[3].
After the introduction of the PAB, the health sector took up the greatest share of many municipalities’ funds originating from federal sources. The widespread distribution of federal resources to municipalities enabled the rapid extension of PHC coverage throughout the country. Some interviewees explained this process:
[I1] The model was essential to reduce health inequalities and to engage municipal managers, integrating all municipalities into SUS and making it possible to have PHC services throughout the country.
[I3] The population-based financing mechanism led to a significant injection of resources in the municipalities, especially in the smaller ones, and a rapid extension of PHC coverage.
[I8] For many small municipalities, the fixed PAB component represented more than the FPM (municipal participation fund). Especially in the North and Northeast regions, many municipalities had never received federal health funds, which usually paid for the provision of secondary and tertiary care services.
According to the Ministerial decree which established the PAB-fixed component, the per capita value should have been readjusted based on the same increase in fees for the SUS national list of outpatient procedures (tabela SUS). From 1998 to 2019, the PAB-fixed per capita amount increased from R$ 10.00 to a maximum of R$ 28.00. If adjusted for the IPCA inflation rate in the period, the maximum in 2019 would have been approximately R$ 35.50. In 2020, the PAB components were replaced by risk adjusted capitation as part of the implementation of the Prevent Brazil programme.
Incentives for adopting the FHS model: the PAB-variable component
The variable component of the PAB was designed to encourage municipalities to implement federal priority programmes for PHC that were linked to receiving the federal funds. Based on experiences in the Northeast region, the Community Health Workers (Programa Agente Comunitário de Saúde — PACS) and Family Health (Programa Saúde da Família — PSF) programmes had a limited expansion immediately after being established in 1991 and 1994 respectively. At that time, the policy focused on deprived regions of the country, and to receive federal funding, municipal governments needed to sign fixed-term renewable annual contracts with the MoH.
After 1998, to receive funds via the PAB-variable mechanism, municipalities had to submit a request to the MoH to adopt the programme. Following the MoH’s approval, they needed to maintain an updated record of the professionals working in FHS teams in the National Register of Health Facilities System (SCNES). In addition, they had to inform the MoH of the monthly production of these teams. Irregularities in information could cause suspension of the PAB transfers to the municipality.
Although initially for a lower amount, the PAB variable-component grew over time, corresponding to 56.9% of the total PAB-transfers from 2000 to 2018, as shown in Table 3. This demonstrates the MoH strategy for encouraging municipalities to adopt the FHS model and other national priorities, rather than increasing the PAB-fixed amount. Nevertheless, municipal health secretaries’ representatives regularly requested to use the PHC funds more freely, as pointed out by one of the interviewees.
[I8] While the public manager can invest the fixed PAB more freely, the variable PAB financing — linked to FHS teams — sought to extend PHC coverage and the provision of professionals.
Initially restricted to subsidising basic FHS teams and CHWs, the PAB-variable element was expanded over time, covering a broad range of other incentives for PHC. They included other specialized professionals to support FHS teams — Oral Health and NASF (Nucleo de Apoio ao Saúde da Família) — and models of FHS teams for specific populations, such as the Riverine, Indigenous, and homeless people. The PAB variable mechanism was also used to transfer financial incentives for auxiliary and strategic programmes for PHC, such as the Programme for Improving Access and Quality of Primary Care (PMAQ), Health Gym Programme, Health at School, and others showed in Table 6.
Table 6: Incentives covered by the PAB-variable component
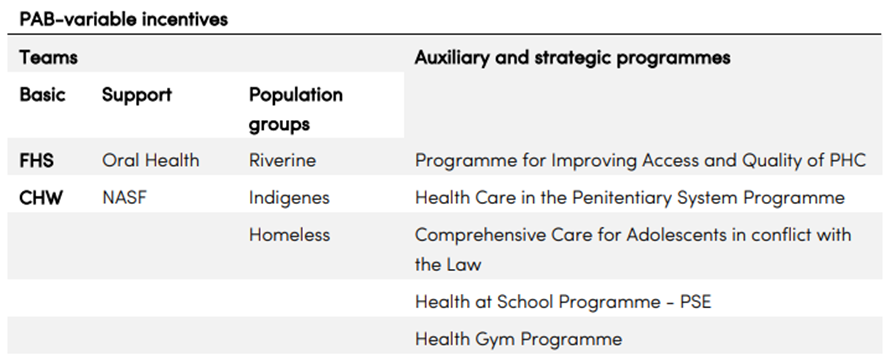
Source: Authors´ own work based on MoH report
Achievements in expanding PHC services delivery
The scaling-up of FHS
The combination of the PAB fixed- and variable-components simultaneously encouraged the expansion of FHS coverage and shifted the model of care provided in Brazil. The number of FHS teams grew from 2,054 to 43,286 between 1998 and 2020, covering 133.7 million people, 63.3% of Brazilians. However, there were differences between regions in implementation and in the speed of increase of coverage, as shown in Figure 2. In 2020, the variation in FHS coverage between states ranged from 40.7% in the state of São Paulo to 99.7% in the state of Piaui.
Figure 2: Number of FHS teams and percentage of population covered
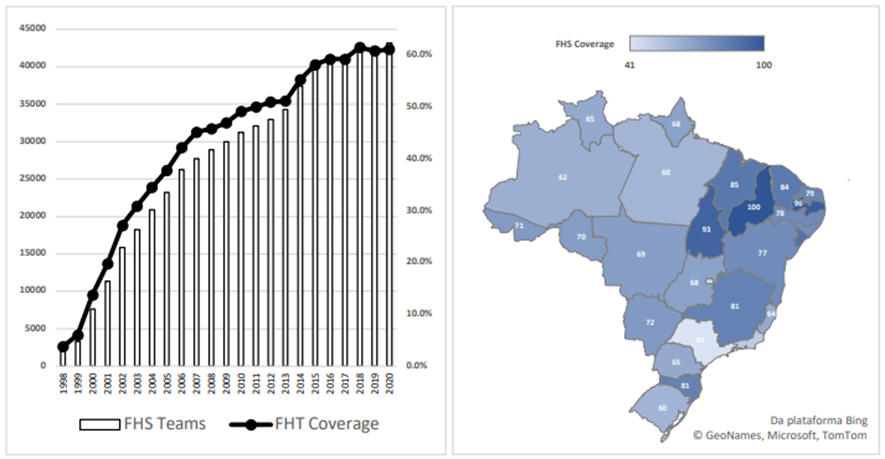
Notes: data originally from MoH — PHC indicator panel. For the map, we used data on coverage as of January of 2020.
As an initial strategy to foster an increase in FHS coverage, from 1998 to 2003 the MoH paid higher amounts for each FHS team to municipalities that had achieved a higher overall level of FHS coverage. The amount nearly doubled in value in that time.
To foster the expansion of the FHS in municipalities with more than 100,000 inhabitants, where over 60 percent of Brazil’s population resided and where the level of FHS coverage was lower, the federal government sought funding from the World Bank, creating the Family Health Extension Programme (PROESF — Programa de Expansão e Consolidação do Saúde da Família) in 2002. Designed as a U$ 550 million seven-year programme — 50% financed by the World Bank with 50% matched funding from the federal government — a U$ 68 million loan in support of the first phase of the program was approved in 2003. There was another U$ 83.45 million loan in 2008 for its second phase, of which U$ 34.7 million was spent. The third phase was not carried out, reportedly because the interest rate was too high. As an outcome of the programme, FHS coverage in 184 municipalities included in PROESF increased only from 25.7% to 39.5% between 2003 and 2011 (Coutolenc and Dmytraczenko, 2013)[4], remaining at a much lower level than the coverage of small municipalities.
To implement more equitable financing in 2004, the MoH changed its method for calculating the incentive amount for each team. An additional 50% was included for FHS and Oral Health teams for municipalities with less than 30,000 inhabitants (less than 50,000 inhabitants in the Amazon region), with a Human Development Index (HDI) less than or equal to 0.7, and with “quilombola” settlements. For the first time, indicators of social conditions were used as criteria to differentiate federal transfers to municipalities for SUS financing (Solla et. Al, 2007)[5].
The FHS coverage grew progressively from 1999 to 2007. The fiscal space, generated from sustained economic growth during the 2000s, was also an important factor behind the increase in PHC spending. However, from 2007 to 2013, there was a slowdown in the growth of FHS teams. This change can be attributed a federal government initiative to invest in Emergency Care Units (Unidade de Pronto Atendimento — UPA), which are not part of PHC teams, and the increase in private health insurance coverage following growth in formal employment in the country. These factors may have made it more difficult for municipalities to hire health professionals, especially doctors, explained by interviewees.
[I11] With the economic growth and full employment in Brazil, there was an increase in the population coverage by private health insurance, demanding more doctors in the sector, which aggravated the difficulty for municipalities to hire these professionals.
[I13]. Between 2007–2010 there was a stagnation in FHS growth and a greater focus on the expansion of UPAS (simple emergency care units, similar to walk-in clinics) — since urgency/emergency services are more attractive as a political proposal, which converts into votes.
Finally, the federal government reduced the flexibility of the composition of the FHS team to increase PHC coverage rapidly. In a country of continental dimensions with significant regional differences, it is challenging to have a single way of working that adapts to the diversity of social, cultural, epidemiological, and demographic characteristics, as mentioned by the interviewees:
[I4] The FHS team’s model and composition should be more flexible, to accommodate local needs (e.g., poverty, geography, epidemiological and health conditions, consumption profile, and demand for health services).
[I8] If municipalities made other measurable performance commitments for their FHS teams (e.g., description and accountability for users within their territory), the FHS team organization format would not be the only way to obtain financing from the MoH. This would enable the inclusion of municipalities that had already adopted other formats of PHC teams.
[I13] It is not enough to provide general guidelines and quality indicators, it is necessary to assure mechanisms to increase the management capability of the municipalities (for example, institutional support for personnel management, continuing education, and quality improvement processes).
Enlarging the scope of FHS
Besides scaling-up coverage, national policies for PHC sought to enlarge the scope of actions carried out by FHS teams over time. The handbook for the FHS was published in 1998, defining the concept of PHC, responsibilities of municipal managers, lists of actions, activities, and guidelines for the transfer and use of funds, and mechanisms for monitoring and controlling the financial resources earmarked for the PAB. The PHC information system (SIAB — Sistema de Informação da Atenção Básica) was also created for municipalities to register the FHS team production and for the MoH to monitor it.
In 2006, the FHS was consolidated as the priority organisational model for PHC in the SUS by the National Primary Health Care Policy (Política Nacional de Atenção Básica — PNAB). The policy reinforced a broad concept of health and emphasized that the FHS is the basis for health system organisation, underpinning first contact, whole-of-life care, comprehensiveness, coordination, community orientation, the centrality of the family, and community cultural awareness. However, no additional financial incentive was allocated to PHC through the PNAB.
One way to raise the priority of PHC in the federal government and increase funds to expand the coverage of the FHS was through integration with other social policies, such as Bolsa-Familia. Created in 2004, this programme was the highest government priority, transferring cash from the federal government to poor households. According to one interviewee:
[I8] Intersectoral cooperation was a way for the MoH to obtain more resources for PHC making itself available to work with and make joint policies with other ministries. To that end, political will and technical knowledge are necessary to explain the functioning and relevance of PHC with the help of evidence-based arguments.Linked to Bolsa Familia, a national registry of low-income households was developed targeting social programmes — CADUNICO. Although the Bolsa Familia programme has conditions linked to health, there is no formal linkage between the programme and health care provision within the SUS. However, the families enrolled in programme are identified in the MoH information system only within the scope of the health services, which are a condition for cash transfers under Bolsa Familia, such as vaccination of children under age 7, growth-monitoring, child health visits, pre- and postnatal visits, and breastfeeding and nutrition activities (Coutolenc and Dmytraczenko, 2013)[6].
The association between FHS and Bolsa-Familia programmes led to substantial increases in immunisation, and reductions in child malnutrition and in under-5 mortality, especially for deaths attributable to poverty-related causes, such as malnutrition and diarrhoea (Rasella et al. 2013)[7]. However, according to one of the interviewees, the cooperation between the Bolsa-Familia programme and the FHS teams could have been developed even further to improve the performance of PHC services, as stated:
[I4] Just having PHC professionals — without monitoring their performance — is not enough. To do so we need to be more rigorous in the registration of users, given that the appropriate technology was already available, for example, CADUNICO has a set of information about Brazilian families in poverty and extreme poverty, and the Bolsa Familia registration systems are much better than those of the SUS.
New federal financial incentives were created to increase the scope of PHC services, by including other professionals in FHS teams, such as dentists in 2001, and other specialists to support FHS through the NASF (Núcleo do Apoio ao Saúde da Família) in 2008. The federal incentive was set higher for NASF than for the FHS teams, aiming to encourage municipalities to accept responsibility for expanding PHC coverage and the scope of services provided, according to one interviewee:
[I8] Created in 2008, NASF had a much higher financing per team than the FHS team — and this encouraged municipalities to accept responsibility for greater PHC coverage. Due to the composition of NASF, the provision of professionals in the municipalities became easier.
Challenges for scaling up the FHS
Health system financing
The expansion of service provision in the SUS during the 1990s was not covered by a new and stable source of funding and the government failed to implement the health system financing proposal to use resources from the federal social security budget, as set out in the 1988 Constitution. In 1997, a temporary tax on financial transactions (CPMF — Contribuição Provisória sobre Movimentação Financeira) was established to cover funding shortfalls. Although the entire tax revenue was initially allocated to the health sector, only about 30% of the CPMF income ended up in the sector, with the rest allocated to other areas, in particular towards paying the administrative costs of the federal government. This temporary tax was not renewed after 2007, further aggravating the federal underfunding of health.
To address underfunding of the health system, a political movement composed of mayors, SUS managers, and civil society gathered to demand the approval of a source of funds for the SUS. As a result, the Constitutional Amendment 29 (EC-29) was approved in 2000 by Congress, defining a minimum amount of health funding by each government level. It stated that state governments had to spend at least 12% of their total revenues on health, while municipalities had to apply a minimum of 15% of their total revenues, as reported by an interviewee:
[I1] The ‘EC 29’ standardized the transfers by the federal, state, and municipal governments and represented an attempt to establish a health commitment among them.
However, contribution from the federal government was not indexed to a specific amount but was, instead, based on the amount spent in the previous year adjusted for GDP variation, as stipulated by the Ministry of Economy. The challenge of increasing federal funding for health is explained by an interviewee:
[I9] It’s not easy to discuss health budgets with the government economic team — the health sector is seen as a ‘wasteful’ area.
The minimum values defined by the EC-29 were later endorsed by Federal Law 141 in 2012. However, the formula for calculating the federal government contribution changed several times. It was last redefined in 2018 under recent fiscal austerity measures as the amount committed in the previous year, limiting the growth to the variation in inflation.
Although federal transfers were decisive for encouraging municipalities to take responsibility for managing the health system, and resources from PAB fixed- and variable components underpinned the configuration of the PHC based on the FHS model nationally, municipalities became ultimately responsible for paying the costs of these services. As the federal transfers decreased relatively over time, it was the municipalities’ own contributions that grew the most from the year 2000 onwards, as shown in Figure 3 (Panel B).
According to SIOPS records, between 2000 and 2017 total health spending per capita grew approximately 3-fold on average, from R$244 to R$738, while the average share of spending funded by transfers decreased from 45% to 41.4%. In particular, the average share of spending funded by PAB decreased from 31% to 24%. Still, transfers grew substantially in absolute terms, from R$99 per capita in 2000 to R$284 in 2017, when PAB represented on average 61% of total transfers in per capita terms.
Spending in PHC specifically increased substantially as well. It is worth noting that data on spending in PHC are originally provided by FINBRA, are available only from 2005 onwards, and do not allow us to connect expenditure with sources of funding. In this case, trends in expenditure on PHC might reflect funding from both transfers (e.g. PAB) and own resources, and are not necessarily connected to spending in the FHS — although spending in PHC and FHS are expected to be highly correlated. We observe that from 2005 to 2018, per capita spending on PHC rose exactly twofold, from R$245 to R$490, while the share of spending on PHC in respect to total municipal expenditure on health remained stable at 58% through the period.
Figure 3: Total Municipality Spending Growth and By Source of Funding
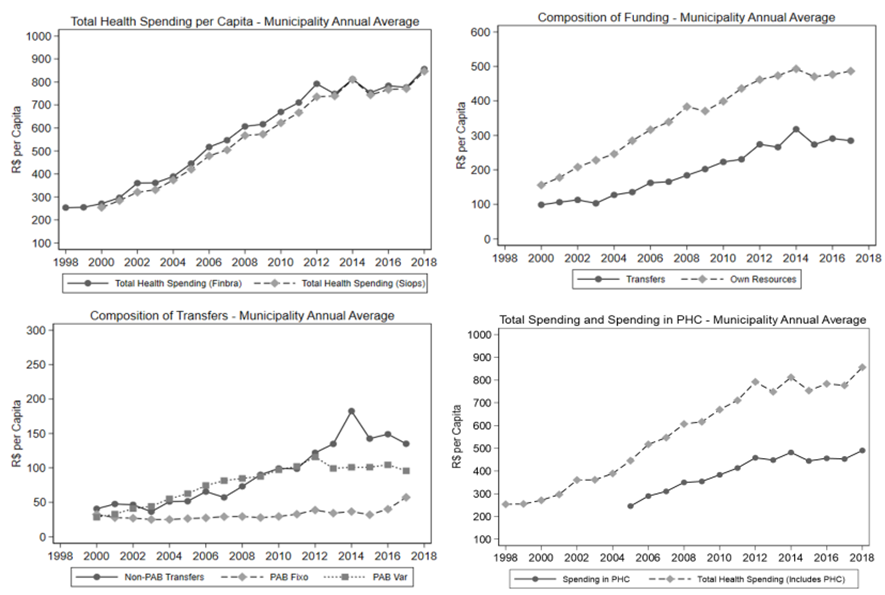
Notes: data originally from FINBRA and SIOPS. The plots present annual averages in per capita spending (in R$ values of 2018) across municipalities.
There are also considerable inequalities in levels of health expenditure across municipalities, as most of the municipal funding is associated with their own revenues and taxation capacity. The upper plots of Figure 4 show that total spending per capita is systematically lower for northern states (in the North and Northeast regions), where most of the poorest and most socioeconomically deprived municipalities in Brazil are located. We observe that the difference between northern and southern states comes entirely from own resources, as transfers are generally an equalizer. Indeed, in the bottom plots we observe that inequality in total spending per capita has decreased. The reduction in the Gini Index is led by a generally lower and decreasing Gini Index for transfers.
Figure 4: Inequality in Health Expenditures
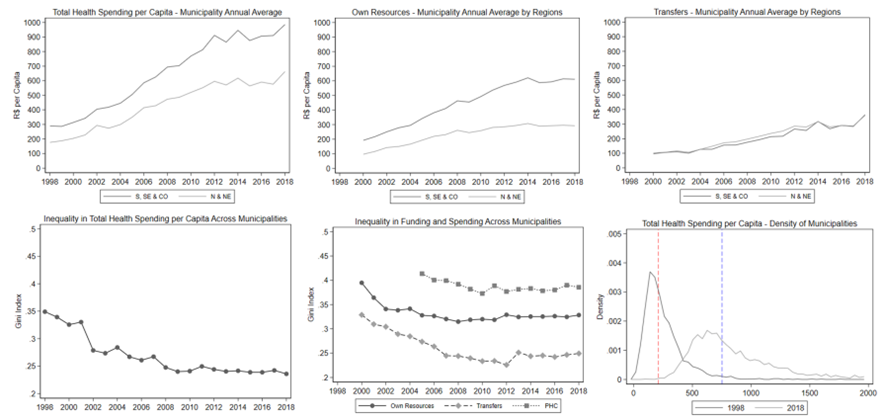
Notes: data originally from FINBRA and SIOPS. The upper plots present annual averages in per capita spending (in R$ values of 2018) across municipalities. The first two lower plots present Gini coefficients computed annually on municipality per capita spending. The remaining lower plot describe kernel densities for total spending in 1998 and 2018 based on data from FINBRA. The vertical dashed lines represent median R$ values for 1998 and 2018, respectively.
The upper plots of Figure 5 show the results of our equation (1), used to estimate the baseline determinants of total growth in health spending in general (between 2000 and 2017), and in PHC in particular (between 2005–2017). Growth in total spending was indeed lower in poorer municipalities and in the North and Northeast regions. Spending grew faster in municipalities with higher scores for municipal health governance, larger coverage of private health insurance, and higher HDI circa the promulgation of the 1988 Constitution and the creation of SUS. Independent of all previous factors, spending grew faster in smaller municipalities. A similar pattern is found for spending in PHC specifically.
On the other hand, the lower plots of Figure 5 are consistent with the view that transfers have been a relevant equalizer force. When we repeat the exercise by source of funding, we observe that PAB transfers have been either neutral or have contributed to spending growth in the poorest and smallest municipalities. An opposite pattern is found for growth in own resources. Interestingly, the lower right-hand plot suggests that the elasticities between own resources and total spending is relatively high, while the opposite if found for PAB transfers regarding spending in PHC. More specifically, an increase of 1% in PAB transfers has been converted into an increase of approximately 0.5% in PHC spending — which is nearly two-fold the elasticity associated with an increase of 1% in own resources.
Figure 5: Determinants of Spending Growth
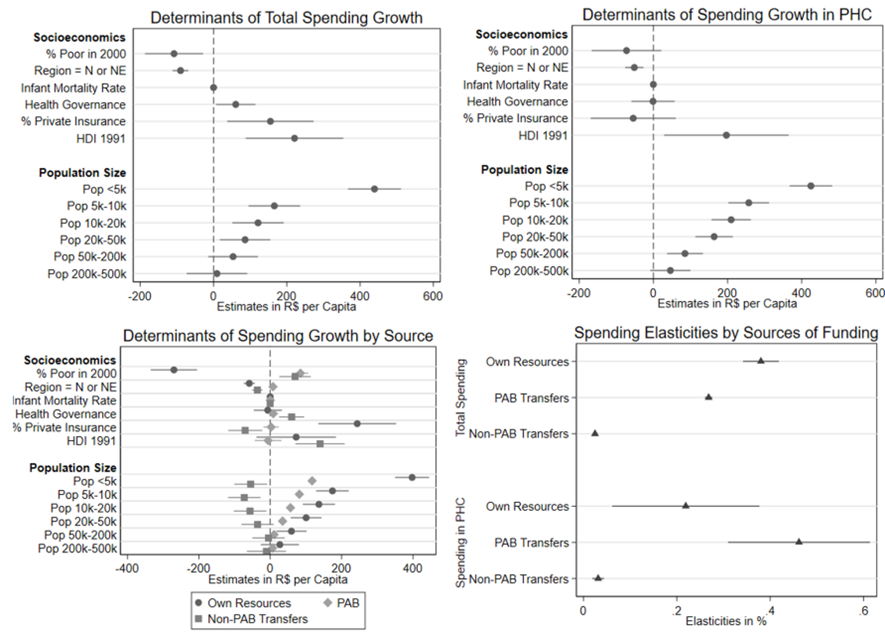
Notes: the upper plots present the results of equation (1), in which the variation in total spending (2000–2017) or in spending in PHC (2005–2017) were regressed on a set of baseline characteristics. The lower left-hand plot presents the results of regressions ran separately for spending growth by source of funding (own resources, PAB, and nonPAB transfers). The remaining plot documents the results of model (2), used to estimate the relationship between variation in total spending (or in spending in PHC, between 2005–2017) and variation in funding by source. Dependent and independent per capita spending variables are computed in logarithmic scale, so point estimates correspond to elasticities. In all regressions standard errors are clustered at the municipality level, all plots report confidence intervals at 95%.
Health System governance
The 1988 Constitution enhanced municipal responsibilities for providing public services by giving municipalities financial, administrative, and political autonomy, based on the assumption that municipalization was the best way to strengthen democracy. However, it established that the federal government should define national priorities, design policies and create mechanisms for supporting its implementation by lower levels of government. The role of state governments, to coordinate national policies at the regional level and balance local differences, was poorly executed. As a result, implementation of the SUS and expansion of PHC took place under widely unequal conditions and contradictions.
Decentralization to the municipal level allowed the construction of a unified health system in a continental country, reducing inequalities by including smaller and poorer municipalities in the SUS. However, given the significant regional heterogeneity and socioeconomic disparities in the country, considerable differences in the technical and administrative capacities of the municipalities created distinct differences in service delivery in PHC and integration with healthcare networks.
Furthermore, the coalition of tripartite management groups (CONASEMS, CONASS, MoH), which created a political and social basis to support the implementation of SUS including the approval of PHC policies, was not strong enough to create a better design for health system organisation and governance at the regional level.
As a result, municipalities had to undertake responsibility for managing the health system without support from state governments, as mentioned by the interviewees:
[I8] States own certain health resources, scale, and infrastructure that are scarce at the municipal level; they can contribute more to the solution of PHC services.
[I13] The states’ budgets for PHC did not increase enough, especially when compared to the spending of municipalities. In turn, the states do not adequately exercise the role of PHC coordination — to train and motivate FHS teams, and to agree and monitor health and quality indicators in municipalities within their jurisdiction.
[I13] We have not been able to advance and build a clearer obligation for states concerning PHC funding, despite the discourse that a) PHC is a priority and b) PHC is the organizing principle of the health network, and c) the PHC funding is tripartite.
Disparities between municipalities, the low level of participation of state governments and the lack of effective regional governance instruments, hindered the integration of PHC services into healthcare networks. Consequently, while the PHC financial arrangement was able to increase FHS coverage, it was not able to encourage FHS integration into health networks.
In 2001 and 2002, the MoH first attempted to organise hierarchical networks and set healthcare operational rules (Normas Operacionais da Assistência à Saúde — NOAS) by developing guidelines for an integrated planning process for distribution and financing of PHC, specialized and hospital services, and organizing them into health regions. In 2006, new guidelines for health system organisation and financing were defined by the Health Pact (Pacto pela Saúde), assembling several federal financial incentives into six financing blocks, including Primary Health Care. In 2011, presidential Decree 7.508 introduced contracts among the three levels of government to organize networks of services in health regions, reinforcing the role of PHC services as the main “front door” for accessing the SUS.
From 2011 to 2013, the MoH introduced a group of policies that set out guidelines and reoriented federal funds for integrating healthcare services in networks — for Maternal health, Emergencies, Mental Health, Disabilities, and Chronic diseases — by region. The policy was designed to overcome fragmentation and inequalities in funding of the health system and proposed to strengthen PHC as the basis for health regions with defined populations and territories.
However, all these efforts were neither supported by new substantial financial incentives nor by a regional managerial structure, limiting the ability to promote the integration of PHC services into health networks. Some interviewees explained these challenges:
[I2] Regionalization is aimed at encouraging networks, in order to bring the system together. However, it lacks clearer political agreements and a better alignment of incentives between the provision and financing of services between ‘importing’ and ‘exporting’ municipalities — those receiving or sending patients to neighbouring municipalities within the health region.
[I5] The proposal of the health regionalization pact was innovative in terms of regional planning, but states were initially concerned about joining in and having increased expenses.
[I9] Funding alone is not enough to organize the network. Health regions need a managerial structure able to coordinate, and a legal and operational mechanism to ensure administrative, bureaucratic, and managerial competence.
[I13] Regionalized planning is not enough if the consolidation of regionalization is not encouraged. The financing unit should be the health region rather than the municipality, but the municipal manager is not keen to assume new regional commitments with the MoH without deriving additional benefits from it.
Resource allocation and municipal management capacities
Despite the evident impact of the financing arrangements in expanding the FHS across the country, municipalities had to take on recurring payments for health staff, maintenance of equipment, and supplies, in highly unequal conditions.
There is considerable variation between municipal human resources management practices, the hiring models and the salaries paid to the teams, and in the infrastructure of PHC facilities. Municipalities with a smaller population in less developed regions of the country, which were the first to adopt the FHS model, had more difficulty attracting and retaining qualified health professionals, especially doctors, while wealthier municipalities were able to offer better salaries and working conditions. In addition, the geographic distribution of doctors is strongly skewed toward larger and wealthier cities. For instance, while in 2018, Brazil had 451,777 registered physicians (2.18 physicians per 1,000 inhabitants), there was one physician per 3,000 individuals in municipalities with fewer than 5,000 inhabitants. In comparison, there was one physician per 230 individuals in municipalities with more than 500,000 inhabitants (Scheffer, 2018)[8].
As pointed out by interviewees:
[I8] Human Resources costs are the most expensive element of the PHC budget.
[I12] FHS/CHW are not sustainable in the long run without strategic planning and continuing education related to the provision of professionals.
[I13] The model demands a family doctor (who is presently quite often not trained as such) with 40 hours a week dedicated to the FHS team. The training falls short of the demand for these professionals.
[I13] The decision to introduce a physician in the FHS within a civil service career structure puts pressure on PHC costs, and involves actuarial calculations for many years ahead, so it is a complex decision for the municipal manager.
Direct public administration has posed a series of bureaucratic obstacles for some municipalities to implement the health budget and pay for increased human resources costs, which are becoming unfeasible and are already violating the tax liability law (the level of municipalities’ budget expenditures is capped by law at 60% of their current net revenue). Further, despite the increase in the number of PHC facilities (Unidades Básicas de Saúde — UBS), poor infrastructure has hindered the ability of some clinics to deliver the broad range of PHC services.
To overcome these challenges, some municipalities have entered contracts with Social Organizations (OSS — Organização Social de Saúde). This solution enables staff to be hired and medical supplies bought in a more agile way than in regular public management, as pointed out by an interviewee:
[I3] Direct public administration poses a series of bureaucratic obstacles for executing the health budget at the municipal level. Contracts with OSS enable payment, buying and hiring in a more agile way than in the regular public management in the PHC system. They represent a more flexible management model and encourage good performance.However, adopting OSS as a solution for outsourcing the management of public health services has some drawbacks with regards to weak mechanisms for accountability, transparency, and financial control to prevent manipulation or fraud.
Attempts to address FHS challenges
Health inequalities
A social inequality factor was introduced in the PAB-fixed component in 2011, which defined four different per capita amounts ranging from R$ 18.00 to R$ 23.00. The variation was calculated based on socioeconomic indicators of the municipalities: GDP per-capita; percentage of the population with health insurance; percentage of the population with Bolsa Família; percentage of the population in extreme poverty; and demographic density.
Demands to include a social inequality factor in the PAB-fixed component came in the context of the Federal government establishing and prioritizing the ‘Brazil without Poverty’ programme (Brasil sem miséria). However, despite marginal differences in the per-capita values that were insufficient to produce a substantial change in financial inequalities, its implementation was resisted. Representatives of the SUS health managers at local levels demanded the same increase for all municipalities, as pointed out by one interviewee:
[I13] The need to address inequality through adjustments in the fixed PAB was met by paying more to those in greater need. Despite initial resistance to change, it made no sense to pay the same per capita for São Paulo and Chorrochó — there are different needs, per capita revenue profiles. This generated four groups for the fixed PAB.
The PNAB was also revised in 2011, requiring political efforts to reach agreement for establishing new financing arrangements for FHS teams in the PAB-variable, targeting specific population groups, such as riverine, indigenous and homeless people.
[I11] A great political effort was made to build a rapid pact for the PNAB revision in 2011, in which the MoH encouraged ‘semi-pilot’ projects. The financing of ‘Mobile Clinics´ (Consutório na Rua) and ‘better at home’ (Melhor em Casa) programs, focusing on the health of the homeless population, and home care, were incorporated into the variable PAB to encourage new care arrangements in PHC.
Poor infrastructure
The precariousness of the physical infrastructure was identified as a limiting factor in the provision of PHC services. Created to address the PHC infrastructure problems, the Requalifica UBS was established as part of the ‘PAC’ (Programa de Aceleração do Crescimento), a federal government programme for stimulating the country’s economy. It set a specific financial incentive for the construction, renovation, and improvement of the physical structure of UBS (Unidade Básica de Saúde), as described by interviewees.
[I8] It was necessary to invest in the physical infrastructure of PHC health units (e.g., vaccination rooms, doctors’ offices) to increase the ability to deliver solutions in these units. But although the physical capacity of many UBS and UPAs was precarious, taking existing units out of commission would imply closing many PHC services.
[I13] Until Requalifica UBS, the MoH made infrastructure investments in PHC through agreements with municipalities. This mechanism was improved and became part of the fund-to-fund transfer, with clear and defined rules, either for renovations or for construction/expansion in the ‘capital investment’ financing block. Consequently, the average size of a UBS in Brazil went from 140 to 270m2 — it almost doubled in size.
Performance assessment
Also implemented in 2011, the PMAQ was the first performance-based payment for FHS teams on a national scale. Its design followed a request from the President of the Republic to make increases in resources for PHC conditional on the performance of the FHS. The implementation of PMAQ was negotiated with CONASS / CONASEMS and academics, to create a new financing component linked to the performance of FHS teams, enabling an increase in the flexibility, organization and composition of the model, as reported by an interviewee:
[I13] PMAQ originates from the attempt to encourage change more directly in PHC processes and to reward those who achieve a PHC model closer to what is expected. Within a fund-to-fund transfer, PMAQ focused on a package of new practices and processes believed to be fundamental for PHC and that can be measured and audited.
However, the complexity of the instruments used to assess performance reduced its impact, as pointed out by an interviewee:
[I3] Its toolset is complicated, with many variables and an unclear analysis plan. Changes in its implementation cycles made complete historical series unfeasible. It failed to return information promptly to health managers and created limited practical feedback for professionals.
Provision of doctors
Mais Médicos (More Doctors) programme was created to address imbalances in the distribution of PHC doctors, and has been the most important programme to support the FHS since the creation of the PAB financing arrangement. Instead of sending funding, the MoH provided a scarce resource directly to municipalities that struggled to hire and manage doctors.
[I4] Many small municipalities do not have the structure to attract and maintain qualified doctors. The ‘Mais Médicos’ program was instrumental in increasing the supply of doctors in distant or unattractive areas — reducing healthcare gaps and increasing PHC coverage and delivery of solutions for many municipalities, especially the smallest and poorest ones.
[I13] The ‘Mais Médicos’ programme represented a significant investment and a different funding design, where the federal government provides the doctors instead of transferring their payment to municipalities. Due to its size and role, the federal government has more capacity than the municipalities to provide and allocate professionals across the national territory.
However, these auxiliary programs have their limits. The lack of strategic cohesion between auxiliary programs and health policies has contributed to fragmentation and possible interruption of health efforts and funding. In addition, to create these programs without substantial new funding, the resources were simply reallocated. Finally, many programs have been interrupted or modified in recent years, as one interviewee explained:
[I13] The implementation process of these components (PMAQ, Mais Medicos, etc) was gradual, not global and agreed upon, these interconnected elements are often dissociated when planning budgetary and other changes. This weakens the sustainability of PHC policy.
Overall impact on health inequalities
The analyses outline how financial arrangements have played an important role in encouraging a model of PHC that had clear impacts in reducing the inequality in funding, potentially leading to improvements in access to services and health outcomes.
Figure 6 provides further evidence on the correlation between spending, PHC coverage, access to services, and outcomes. The upper left-hand plot presents the results of our model (2) for different dependent variables. Total spending per capita is positively associated with FHS and CHW coverages. We also observe positive associations with the number of PHC facilities per capita and the share of live births with seven or more prenatal visits during the gestational period. The right-hand side plot shows that most of the variation comes from effects triggered by PAB transfers.
In particular, we find elasticities greater than 1 for both FHS team and CHW coverages, which suggests that the financial arrangements and incentives embedded in PAB may have induced the expansion of PHC teams and coverage much beyond per capita transfers. These results are consistent with patterns observed in the lower plot, which documents spending effects on infant mortality rates (IMR). Although imprecise, estimates suggest a negative association between PAB transfers and IMR. The remaining coefficients are statistically insignificant and closer to zero.
Figure 6: Effects of Health Spending and Sources of Funding on PHC Coverage, Access to Services and Infant Mortality
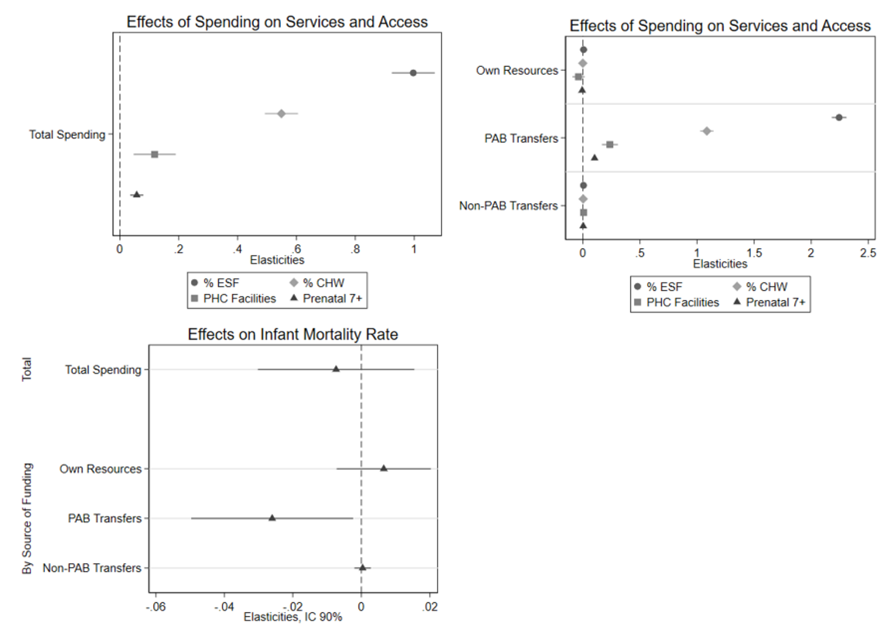
Notes: the three plots present the results of equation (2) separately for different dependent variables: the inverse hyperbolic sine (IHS) transformation of FHS coverage, CHW coverage, number of PHC facilities per capita and the share of 7 or more prenatal visits, in the upper plots; and of the infant mortality rate in the lower plot. Independent per capita spending variables are computed in logarithmic scale, so point estimates correspond to elasticities. In all regressions standard errors are clustered at the municipality level, the upper plots report confidence intervals at 95% while the lower plot report confidence intervals computed at 90%.
Based on the available data, it is not possible to conclude that these arrangements were able to improve service quality. Persistent inequalities remain in the quality of the services with unequal distribution of physicians and facilities, and even the programs that explicitly tried to address inequities were unsustainable and ended.
Risks in transition from PAB to risk-adjusted capitation, and future perspectives
Brazil’s ongoing political and economic crisis has affected financing for all public policies and programs including SUS. Long-term fiscal austerity policies were implemented in 2016 and followed by rationing measures (Massuda et al, 2018)[9].
In 2017, around 1,200 ministerial decrees, which regulate transfers of federal resources, were unified under a single consolidating decree in an initiative called “SUS Legal”, merging SUS financing blocks for PHC, secondary and tertiary care, and others (Brazil, 2017)[10]. As a direct consequence, it is no longer possible to easily monitor the share of PHC in the federal fund-to-fund transfers to states and municipalities (see Table 3). A more serious effect of this measure is the risk of increased underfinancing in strategic areas for health systems, such as PHC and public health, due to the strong political lobby for concentrating financial resources in specialized and hospital care (Massuda et al, 2020)[11]. This problem is also being exacerbated given the rapidly escalating spend on high-cost pharmaceutical products (Vieira, 2018)[12].
Following the fiscal austerity measures, a new policy for PHC financing was introduced in 2019 called Prevent Brazil (Previne Brasil) with the support of technicians from the World Bank (Harzheim et al, 2020)[13]. This policy replaced the PAB fixed and variable components with a capitation mechanism, based on the number of people enrolled in FHS teams registered by municipalities, weighted by socioeconomic vulnerability criteria. Despite recognising the need for PHC financing reform and the eventual benefits of capitation and performance assessment mechanisms that encourage greater accountability of managers and professionals, several interviewees reported concern about its effects. These include the risk of significant fluctuations in financing given the fiscal restrictions in the country.
[I2] ‘Previne Brasil’ and ‘SUS legal’ represented a rupture in the coalition of interests between managers of the SUS in three federative entities.
[I5] The appraisal of payment for performance in the ‘Previne Brasil’ is complex and many health managers and health teams are unable to implement and monitor it — something that did not happen with the variable PAB payment. Complex financing formulas tend to only work in theory — they end up being used in reverse, to fit existing resources.
[I8] The creation of PAB was an invaluable innovation in the transfer of funds from the federal government to the municipalities. The abolition — instead of the adjustment — of something so successful with the new PHC financing model is incomprehensible, especially in a scenario where there are no new resources for PHC.
[I8] Linking financing to the population registered within SUS — instead of the existing population that, in practice, uses and needs SUS — penalizes health financing. The focus on user registration at the individual level links PHC to an individual care perspective, moving away from the collective and health educational logic, linked to the territory and its communities.
[I13] Due to budget constraints, ‘Previne Brasil’ is an attempt to change funding without the inflow of new resources. It can generate significant fluctuations in financing.
There are already clear signs that the quality of PHC has deteriorated in recent years (Giovanella et al, 2020)[14]. PHC was mainly responsible for the increase in vaccination coverage in the country, reaching more than 95% of the target population, but since 2016 vaccination coverage has been decreasing, with major differences between municipalities (Arroyo et al., 2020)[15]. Infant mortality, which also declined substantially following the implementation of the SUS and the FHS, stopped falling and grew slightly for the first time in 2016 (Colluci, 2018)[16].
Finally, during the COVID-19 epidemic, which has dramatically affected Brazil causing more than 321,500 deaths by March 31st 2021, PHC is playing at best a secondary role in the country’s response (Massuda et al., 2021)[17]. Unlike during previous public health emergencies, in which FHS teams played a leading role coordinating public health actions to interrupt disease transmission and to protect vulnerable population groups, the lack of preparedness of PHC teams to deal with the pandemic is a disaster (Lotta et al., 2020)[18].
5. Discussion
To our knowledge, this is the first study that used a mixed-method approach, combining data analysis, interviews with key actors, and reviewing official documents to explore the historical development of the SUS financing arrangements and its effects on the FHS scaling up in Brazil.
Our analysis suggests new elements in understanding how government financing mechanisms underpinned the FHS expansion in Brazil, the progress achieved, and unresolved challenges.
Findings related to the research questions
The political context of strengthening democracy, economic development, and social progress in Brazil enabled the development of national policies to ensure a sustained advance towards UHC between 1990 and 2015.
Scaling-up of the FHS occurred in this environment with significant financial and political commitment from the federal government and implementation the responsibility of municipalities.
Our findings highlight that this lay at the core of the reform of Brazil’s health system.
Having a PHC model in place “shovel-ready” meant that the additional financing translated into rapid scaling-up of the FHS.
The fiscal space generated from economic growth at the time, as well as the politics, were both important factors behind the increase in PHC spending.
The population-based resource allocation mechanism, which provided financial incentives to encourage the adoption of the FHS, created an important financing arrangement for driving the change.
PAB replaced the fee-for-service reimbursement to providers, which had previously concentrated resources in wealthier regions, and spread federal resources to all municipalities to expand the provision of PHC services, with relatively greater benefits for those in deprived areas.
Additionally, our findings emphasise how driving federal funds to public managers underpinned an active role for municipal governments in managing the health system, which together with a steady flow of federal funds for PHC, created a resilient way of delivering community-based PHC services.
However, despite the successful scaling-up, fragilities in the financial arrangements and the unresolved problems of the SUS left inequalities largely unchanged.
Although the PAB variable component encouraged scaling-up of the FHS in regions where public need was greatest, this expansion was funded largely by rises in municipal own resources amid a chronic federal underfinancing of the SUS.
Our findings show that the rise in per-capita health expenditure overall was faster in wealthier municipalities.
Since municipal governments had to take on regular payments for PHC services, including medical staff, the financial inequalities between municipalities exacerbated imbalances in the allocation of resources, particularly doctors.
Our findings also show that despite the proportion of PAB-transfers reducing over time, correlations between PAB-transfers and input/outcome indicators are substantially stronger compared with correlations between municipal funding and the same indicators.
This fact highlights the crucial role of federal resources in encouraging the FHS model, which achieved remarkable results.
Overall, on average, federal transfers have been relatively less important as a source of funding for municipal health services, PHC included, but the marginal funding allocated through federal mechanisms has had the greatest impact.
On the other hand, our findings evidence fragilities in the financing arrangements with tensions between decentralised responsibility and federal standards, which limited innovation and local responsiveness.
Aiming to increase PHC coverage rapidly with the same model, it reduced the flexibility of the composition of the FHS team, compromising its capacity to adapt to the wide diversity of social, cultural, epidemiological, and demographic realities, hindering quality assurance.
In addition, we observed that federal initiatives to address FHS challenges — management support, performance assessment, uneven distribution of doctors, and crucially, integration into regional networks — have had limited impact due to other health system fragilities.
Overall, the mix of financing arrangements, designed and channelled through federal transfers and directed to municipalities, has never targeted goals other than FHS scaling-up, and improvements in coverage and quality of services at the municipal level.
As a result, coordination of actions and policies between municipalities, within regions, and integration of PHC services into a more structured and coordinated grid of mid- and high-complexity services have been limited.
Finally, all these arrangements are currently under revision with likely adverse consequences.
Despite the need to improve financing arrangements to address PHC challenges, the substitution of PAB-transfers by capitation and performance assessment is risky for several reasons.
Firstly, in a widely unequal continental-size country, with a health system decentralised to the municipal level, the PAB arrangement was crucial for creating a stable source of funds for PHC and to drive the implementation of the FHS model. Losing it may provoke undesirable fluctuations in PHC financing.
Secondly, if not supported by the MoH, the registration of the population and assignment to FHS teams, as well as the recording of performance indicators, are not easy tasks. This is particularly worrisome among municipalities in deprived regions, which typically lack state capacity and rely relatively more on federal transfers. Its effects are likely to reverse gains in reducing health inequalities between municipalities that had been achieved by the expansion of FHS.
Thirdly, despite the eventual benefits of adopting capitation to encourage FHS teams to be held accountable by the people they assist, its implementation as a substitute for PAB, in a context of economic crisis and long-term austerity measures, may serve to limit the provision of PHC services by the constrained resources. As a result, the recent changes proposed in financing arrangements for PHC are likely to jeopardise the universal and comprehensive character of the FHS model, which ought to be the major impetus for the reform of Brazil’s health system.
Findings related to the existing literature
Our findings draw attention to how financial arrangements established to expand UHC in Brazil encouraged the scaling up of FHS, contributing to improvements in access and health outcomes, with relatively more benefits to those in deprived areas.
Positive effects of FHS were associated with a reduction in social inequalities, avoidable hospitalizations, infant- and amenable mortality causes (Hone et al., 2017[1]; Macinko et al., 2010[2]; Dourado et al., 2011[3]; Ceccon et al., 2014[4]; Macinko et al., 2006[5]; Aquino et al., 2009[6]; Rocha and Soares, 2010[7]; Rasella, 2013[8]; Macinko and Lima-Costa 2012[9]; Lima-Costa et al., 2013[10]; de Santiago et al., 2014[11]).
It is in line with the overall literature, which shows that the strengthening of PHC systems is associated with improvements in health outcomes and an equitable distribution of these better outcomes (Starfield et al., 2005[12], Macinko et al., 2009[13]; Kruk et al., 2010[14]; Bitton et al., 2019[15]).
However, PHC financial arrangements had limitations. The FHS was implemented in Brazil with substantive regional differences.
This contrasts with the experiences of PHC in high-income countries, developed as the effective basis for health systems (Friedberg et al., 2010[16]; Starfield, 2010[17]; Kringos, 2013[18]).
Persistent health inequalities in Brazil, enhanced by a dual public-private health system, was a critical obstacle not only to FHS expansion, but also for undermining the PHC functions in the SUS, such as coordination of access to the health system (Andrade et al., (a) 2018[19]; Andrade et al., (b) 2018)[20].
Our study also highlights some consequences of the recent economic and political crisis and fiscal austerity measures, aggravating the chronic federal underfunding of SUS, and changing PHC financing arrangements.
The literature describes a cascade of events triggered by restrictive fiscal policies that weakened PHC systems and led to citizens foregoing healthcare.
Consequently, there is an increase in unmet health needs, in the use of emergency services, and in preventable hospitalization and avoidable mortality (Karanikolos et al., 2013)[21].
The restriction of federal health funds and the deregulation of PHC policies are rapidly deteriorating the role of PHC in the health system in Brazil.
As reported by the literature, progress achieved by the FHS expansion is under threat (Camargo et al., 2020[22]; Vieira, 2020[23]; Melo et al., 2020[24]; Melo, Mendonça and Teixeira, 2019[25]; Melo et al., 2018[26]).
Finally, in a review of PHC financing arrangements in Brazil, the obstacles reported in the scant literature (Silva, 2017)[27] agree overall with the challenges that emerged from our in-depth interviews with key informants.
It is worth mentioning that the national and international literature includes few studies describing the complexity of challenges, factors, and implications of implementing financing mechanisms and policies to strengthen PHC (Angell, 2019[28], Goodyear-Smith et al., 2019[29]; Silva, 2017[30]).
There is little country-specific evidence of PHC financing in low- and middle-income countries (Goodyear-Smith et al., 2019)[31].
Aspects relevant to other settings
Brazil’s experience with financing PHC can offer valuable lessons for other LMIC settings.
The political will to provide universal and comprehensive healthcare was a major driver for creating financial arrangements for scaling up a resilient FHS model.
In contrast with many other LMIC, PHC in Brazil, inspired by the UK’s National Health Service, was developed to be the basis of health system and not a vertical or separate programme.
Establishing financial transfer to local managers closer to where people live and targeted at PHC, was a successful strategy for fostering political commitment to spreading the delivery of PHC services.
Population-based mechanisms were essential for creating stability and predictability for public managers to invest in PHC, while financial inducements directed the implementation of the FHS.
In this decentralized system, the MoH played a vital role in coordinating national policy and municipalities were crucial for delivery.
The deficiencies of the arrangement also can provide lessons.
Federal health budget constraints led to a disproportional increase in municipal health financing, which created further inequalities in the allocation of resources, such as doctors. This situation was aggravated by the lack of participation by state governments in PHC management, as well as poor health system regional governance.
Attempts to create financial incentives to improve FHS performance and to integrate PHC into health networks both failed. If such attempts only redirect resources, without adding new funds, not only are they unlikely solve the problems, but they can also create other problems. This serves as a warning to the current government about its initiative of replacing the PAB with risk-adjusted capitation.
Limitations
Our study has some limitations. First is the time frame. The decision to look at the period 1990–2015 limits the analysis of factors that preceded the changes and what occurred after 2015. Although some of these previous elements were covered in the interviews, the decision to analyse the restricted period is justified because this was the moment of greatest change to the SUS. It is also justified by the availability of data.
Second is the limited scope of the collected data. The interviews were conducted with only 13 respondents. However, to reduce the problems with data bias, we made the interviews as representative as we could. In addition, the data were all triangulated between document analysis, interviews, and quantitative data. Third, our quantitative results also face limitations. Coefficient estimates of linear regressions should not be interpreted as causal but reveal correlational patterns between municipality spending, its baseline determinants, and their potential consequences in terms of PHC coverage, access to health services, and health outcomes. Besides, we used administrative data in our analysis, which might have been under-reported, potentially leading to attenuation bias in our estimates.

5. Discussion
To our knowledge, this is the first study that used a mixed-method approach, combining data analysis, interviews with key actors, and reviewing official documents to explore the historical development of the SUS financing arrangements and its effects on the FHS scaling up in Brazil.
Our analysis suggests new elements in understanding how government financing mechanisms underpinned the FHS expansion in Brazil, the progress achieved, and unresolved challenges.
Findings related to the research questions
The political context of strengthening democracy, economic development, and social progress in Brazil enabled the development of national policies to ensure a sustained advance towards UHC between 1990 and 2015.
Scaling-up of the FHS occurred in this environment with significant financial and political commitment from the federal government and implementation the responsibility of municipalities.
Our findings highlight that this lay at the core of the reform of Brazil’s health system.
Having a PHC model in place “shovel-ready” meant that the additional financing translated into rapid scaling-up of the FHS.
The fiscal space generated from economic growth at the time, as well as the politics, were both important factors behind the increase in PHC spending.
The population-based resource allocation mechanism, which provided financial incentives to encourage the adoption of the FHS, created an important financing arrangement for driving the change.
PAB replaced the fee-for-service reimbursement to providers, which had previously concentrated resources in wealthier regions, and spread federal resources to all municipalities to expand the provision of PHC services, with relatively greater benefits for those in deprived areas.
Additionally, our findings emphasise how driving federal funds to public managers underpinned an active role for municipal governments in managing the health system, which together with a steady flow of federal funds for PHC, created a resilient way of delivering community-based PHC services.
However, despite the successful scaling-up, fragilities in the financial arrangements and the unresolved problems of the SUS left inequalities largely unchanged.
Although the PAB variable component encouraged scaling-up of the FHS in regions where public need was greatest, this expansion was funded largely by rises in municipal own resources amid a chronic federal underfinancing of the SUS.
Our findings show that the rise in per-capita health expenditure overall was faster in wealthier municipalities.
Since municipal governments had to take on regular payments for PHC services, including medical staff, the financial inequalities between municipalities exacerbated imbalances in the allocation of resources, particularly doctors.
Our findings also show that despite the proportion of PAB-transfers reducing over time, correlations between PAB-transfers and input/outcome indicators are substantially stronger compared with correlations between municipal funding and the same indicators.
This fact highlights the crucial role of federal resources in encouraging the FHS model, which achieved remarkable results.
Overall, on average, federal transfers have been relatively less important as a source of funding for municipal health services, PHC included, but the marginal funding allocated through federal mechanisms has had the greatest impact.
On the other hand, our findings evidence fragilities in the financing arrangements with tensions between decentralised responsibility and federal standards, which limited innovation and local responsiveness.
Aiming to increase PHC coverage rapidly with the same model, it reduced the flexibility of the composition of the FHS team, compromising its capacity to adapt to the wide diversity of social, cultural, epidemiological, and demographic realities, hindering quality assurance.
In addition, we observed that federal initiatives to address FHS challenges — management support, performance assessment, uneven distribution of doctors, and crucially, integration into regional networks — have had limited impact due to other health system fragilities.
Overall, the mix of financing arrangements, designed and channelled through federal transfers and directed to municipalities, has never targeted goals other than FHS scaling-up, and improvements in coverage and quality of services at the municipal level.
As a result, coordination of actions and policies between municipalities, within regions, and integration of PHC services into a more structured and coordinated grid of mid- and high-complexity services have been limited.
Finally, all these arrangements are currently under revision with likely adverse consequences.
Despite the need to improve financing arrangements to address PHC challenges, the substitution of PAB-transfers by capitation and performance assessment is risky for several reasons.
Firstly, in a widely unequal continental-size country, with a health system decentralised to the municipal level, the PAB arrangement was crucial for creating a stable source of funds for PHC and to drive the implementation of the FHS model. Losing it may provoke undesirable fluctuations in PHC financing.
Secondly, if not supported by the MoH, the registration of the population and assignment to FHS teams, as well as the recording of performance indicators, are not easy tasks. This is particularly worrisome among municipalities in deprived regions, which typically lack state capacity and rely relatively more on federal transfers. Its effects are likely to reverse gains in reducing health inequalities between municipalities that had been achieved by the expansion of FHS.
Thirdly, despite the eventual benefits of adopting capitation to encourage FHS teams to be held accountable by the people they assist, its implementation as a substitute for PAB, in a context of economic crisis and long-term austerity measures, may serve to limit the provision of PHC services by the constrained resources. As a result, the recent changes proposed in financing arrangements for PHC are likely to jeopardise the universal and comprehensive character of the FHS model, which ought to be the major impetus for the reform of Brazil’s health system.
Findings related to the existing literature
Our findings draw attention to how financial arrangements established to expand UHC in Brazil encouraged the scaling up of FHS, contributing to improvements in access and health outcomes, with relatively more benefits to those in deprived areas.
Positive effects of FHS were associated with a reduction in social inequalities, avoidable hospitalizations, infant- and amenable mortality causes (Hone et al., 2017[1]; Macinko et al., 2010[2]; Dourado et al., 2011[3]; Ceccon et al., 2014[4]; Macinko et al., 2006[5]; Aquino et al., 2009[6]; Rocha and Soares, 2010[7]; Rasella, 2013[8]; Macinko and Lima-Costa 2012[9]; Lima-Costa et al., 2013[10]; de Santiago et al., 2014[11]).
It is in line with the overall literature, which shows that the strengthening of PHC systems is associated with improvements in health outcomes and an equitable distribution of these better outcomes (Starfield et al., 2005[12], Macinko et al., 2009[13]; Kruk et al., 2010[14]; Bitton et al., 2019[15]).
However, PHC financial arrangements had limitations. The FHS was implemented in Brazil with substantive regional differences.
This contrasts with the experiences of PHC in high-income countries, developed as the effective basis for health systems (Friedberg et al., 2010[16]; Starfield, 2010[17]; Kringos, 2013[18]).
Persistent health inequalities in Brazil, enhanced by a dual public-private health system, was a critical obstacle not only to FHS expansion, but also for undermining the PHC functions in the SUS, such as coordination of access to the health system (Andrade et al., (a) 2018[19]; Andrade et al., (b) 2018)[20].
Our study also highlights some consequences of the recent economic and political crisis and fiscal austerity measures, aggravating the chronic federal underfunding of SUS, and changing PHC financing arrangements.
The literature describes a cascade of events triggered by restrictive fiscal policies that weakened PHC systems and led to citizens foregoing healthcare.
Consequently, there is an increase in unmet health needs, in the use of emergency services, and in preventable hospitalization and avoidable mortality (Karanikolos et al., 2013)[21].
The restriction of federal health funds and the deregulation of PHC policies are rapidly deteriorating the role of PHC in the health system in Brazil.
As reported by the literature, progress achieved by the FHS expansion is under threat (Camargo et al., 2020[22]; Vieira, 2020[23]; Melo et al., 2020[24]; Melo, Mendonça and Teixeira, 2019[25]; Melo et al., 2018[26]).
Finally, in a review of PHC financing arrangements in Brazil, the obstacles reported in the scant literature (Silva, 2017)[27] agree overall with the challenges that emerged from our in-depth interviews with key informants.
It is worth mentioning that the national and international literature includes few studies describing the complexity of challenges, factors, and implications of implementing financing mechanisms and policies to strengthen PHC (Angell, 2019[28], Goodyear-Smith et al., 2019[29]; Silva, 2017[30]).
There is little country-specific evidence of PHC financing in low- and middle-income countries (Goodyear-Smith et al., 2019)[31].
Aspects relevant to other settings
Brazil’s experience with financing PHC can offer valuable lessons for other LMIC settings.
The political will to provide universal and comprehensive healthcare was a major driver for creating financial arrangements for scaling up a resilient FHS model.
In contrast with many other LMIC, PHC in Brazil, inspired by the UK’s National Health Service, was developed to be the basis of health system and not a vertical or separate programme.
Establishing financial transfer to local managers closer to where people live and targeted at PHC, was a successful strategy for fostering political commitment to spreading the delivery of PHC services.
Population-based mechanisms were essential for creating stability and predictability for public managers to invest in PHC, while financial inducements directed the implementation of the FHS.
In this decentralized system, the MoH played a vital role in coordinating national policy and municipalities were crucial for delivery.
The deficiencies of the arrangement also can provide lessons.
Federal health budget constraints led to a disproportional increase in municipal health financing, which created further inequalities in the allocation of resources, such as doctors. This situation was aggravated by the lack of participation by state governments in PHC management, as well as poor health system regional governance.
Attempts to create financial incentives to improve FHS performance and to integrate PHC into health networks both failed. If such attempts only redirect resources, without adding new funds, not only are they unlikely solve the problems, but they can also create other problems. This serves as a warning to the current government about its initiative of replacing the PAB with risk-adjusted capitation.
Limitations
Our study has some limitations. First is the time frame. The decision to look at the period 1990–2015 limits the analysis of factors that preceded the changes and what occurred after 2015. Although some of these previous elements were covered in the interviews, the decision to analyse the restricted period is justified because this was the moment of greatest change to the SUS. It is also justified by the availability of data.
Second is the limited scope of the collected data. The interviews were conducted with only 13 respondents. However, to reduce the problems with data bias, we made the interviews as representative as we could. In addition, the data were all triangulated between document analysis, interviews, and quantitative data. Third, our quantitative results also face limitations. Coefficient estimates of linear regressions should not be interpreted as causal but reveal correlational patterns between municipality spending, its baseline determinants, and their potential consequences in terms of PHC coverage, access to health services, and health outcomes. Besides, we used administrative data in our analysis, which might have been under-reported, potentially leading to attenuation bias in our estimates.

6. Conclusion
Implementing a universal and comprehensive health system in a country with widespread inequality was a major achievement in Brazil.
Influenced by the political impetus to restabilize democracy and increase social rights, and inspired by creative municipal experiences in different regions of the country which sought to overcome adversity, the Family Health Strategy was applied nationwide.
The FHS used financing arrangements that combine federal incentives, composed of fixed and variable components, with municipal resources.
The model showed an efficient and effective way to improve access and health outcomes, especially for the poor, serving as an example of innovation for Latin American and other low-income countries.
However, unresolved structural problems in Brazil, which remains one of the most unequal democracies in the world, and the fragilities of the health system have limited the reach of the FHS.
Financing arrangements were not robust enough to face challenges such as imbalances in the allocation of health professionals, the poor quality of some PHC provision, the need to introduce innovative health technologies and to integrate better with health networks.
Looking ahead, as a prolonged economic and political crisis unfolds in the country, dramatically exacerbated by the COVID-19 pandemic, replacing the successful PHC financing model by simply redirecting the existing resources according to new criteria, is foolhardy.
The PAB was an arrangement that, despite its issues, was fundamental for creating stability in PHC financing.
In moments of crisis, such as the current COVID-19 pandemic, the need for a consistent financing scheme for PHC is crucial.
Capitation can be a valuable enhancement of the financing mechanisms for PHC in Brazil if it is integrated with the successful PAB scheme in a blended model.
Health inequalities are already increasing rapidly, mainly affecting that part of the Brazilian population which benefited most from the Family Health Strategy over the past two decades. These setbacks should not be ignored but reversed, in order to continue to support the fabric of society.
Suggested citation
Massuda A, Malik AM, Lotta G, Siqueira M, Tasca R, Rocha R Brazil’s Primary Health Care Financing: Case Study. Lancet Global Health Commission on Financing Primary Health Care. Working Paper №1. 2022
Funding
This work was funded by a grant from the Bill & Melinda Gates Foundation. However, the views expressed in the case study reports are those of the case study authors and do not necessarily reflect the views or policies of BMGF.
Originally published at https://www.researchgate.net
© London School of Hygiene & Tropical Medicine 2022© London School of Hygiene & Tropical Medicine 2022