the health and tech strategist
institute for continuous health transformation
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
March 13, 2023
EXECUTIVE SUMMARY
The Biden-Harris administration’s has made proposal to launch a five-year program aimed at eliminating hepatitis C in the US.
- Although direct-acting antivirals (DAAs) have been developed that can cure more than 95% of people infected with hepatitis C, the treatment is not reaching many of the over 2.4 million US residents who are chronically infected with the disease, resulting in over 15,000 unnecessary deaths annually.
- The administration’s program seeks to significantly expand screening, testing, treatment, prevention, and monitoring of hepatitis C infections in the United States, with a focus on populations at the greatest risk for infection.
- The program has three main priorities:
(1) accelerating the availability of point-of-care diagnostic tests,
(2) providing broad access to curative hepatitis C medications, and (3) implementing a comprehensive public health effort to identify persons with hepatitis C and link them to care.
- The administration is calling on Congress to support the program to eliminate hepatitis C in the United States.
DEEP DIVE
A National Hepatitis C Elimination Program in the United States
A Historic Opportunity
JAMA Network
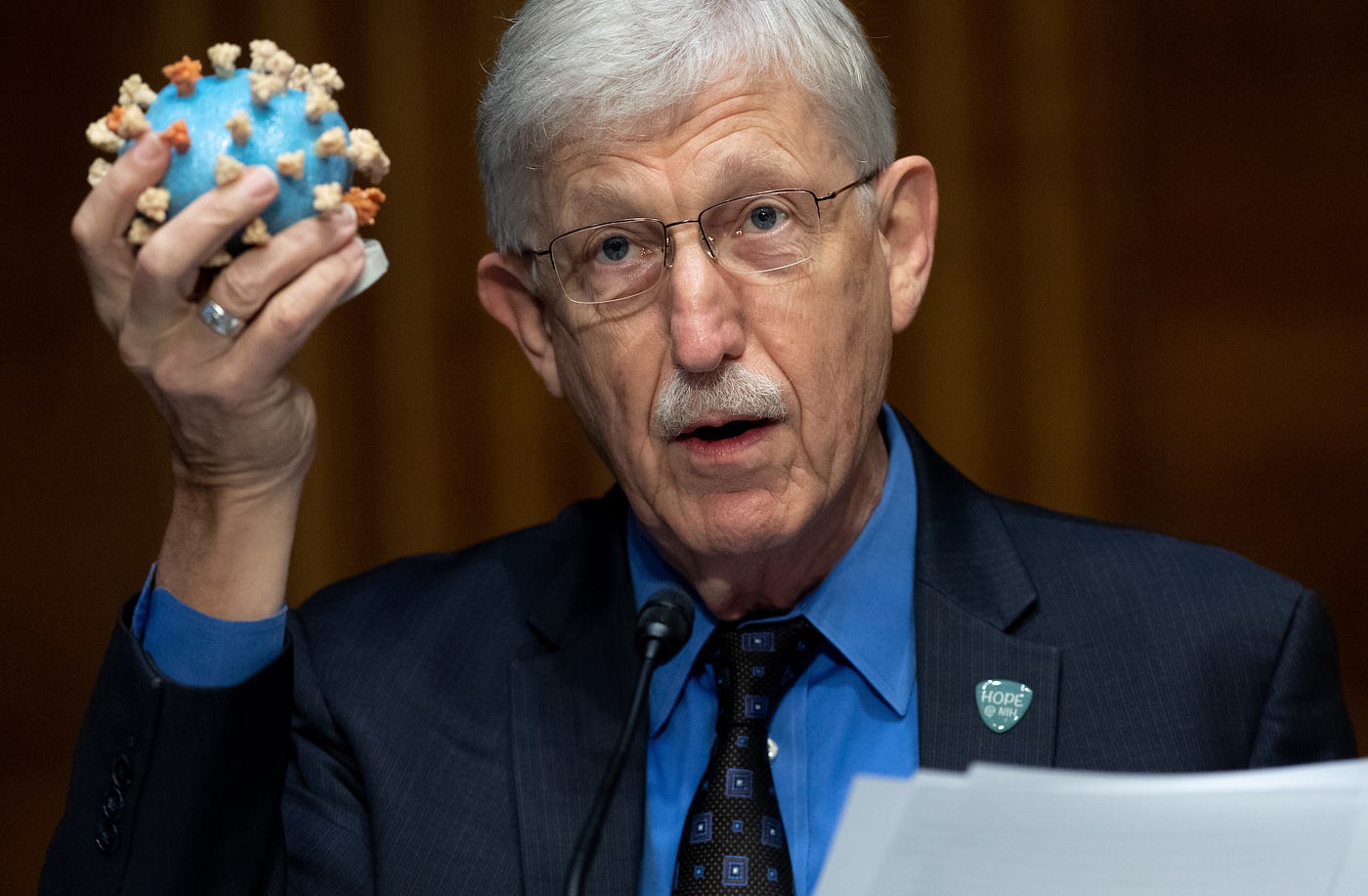
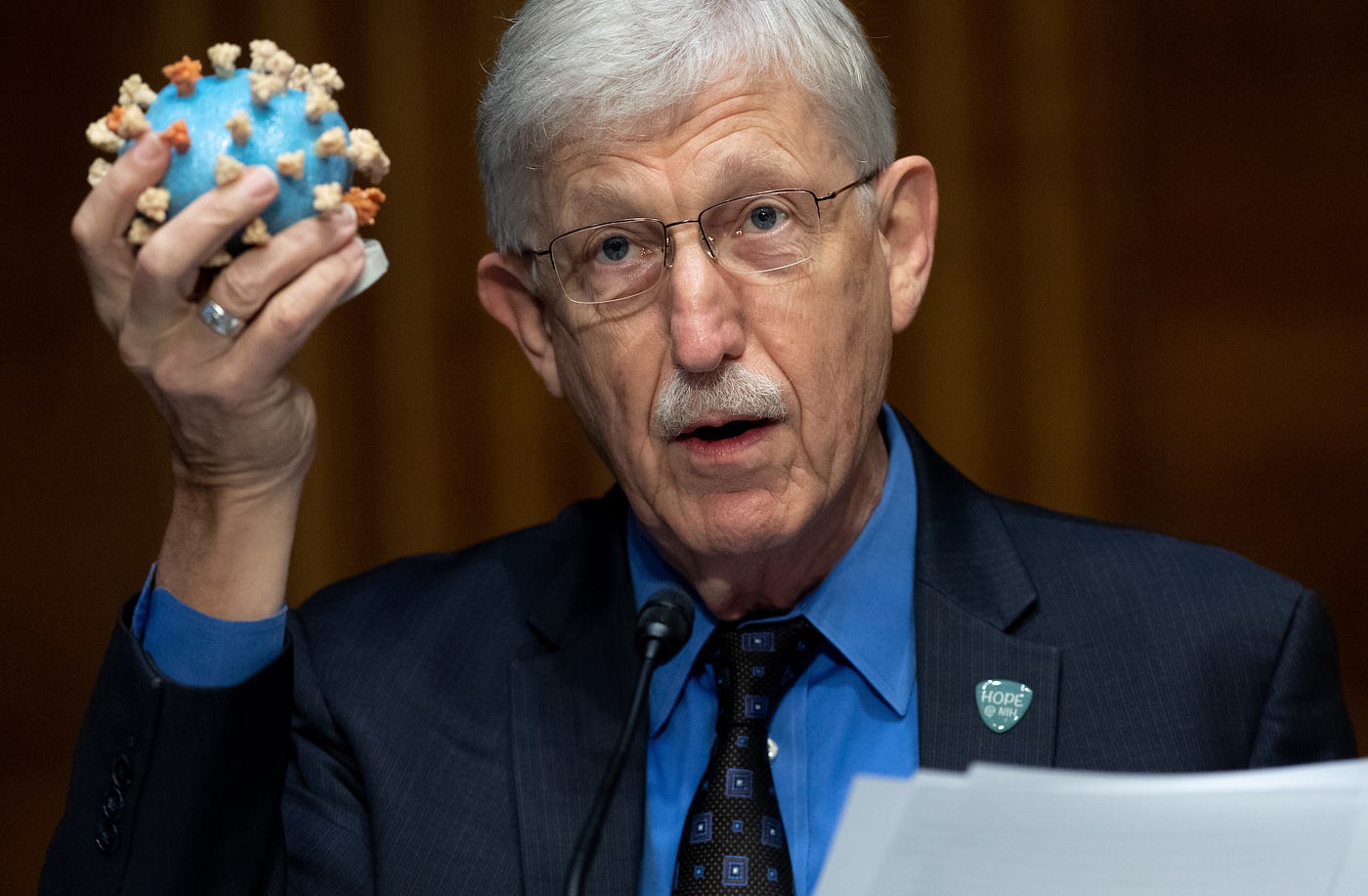
Rachael L. Fleurence, MSc, PhD1; Francis S. Collins, MD, PhD1
March 9, 2023
One of the most dramatic scientific achievements of the last few decades has been the development of direct-acting antivirals (DAAs) that can cure hepatitis C in more than 95% of people infected.
But 9 years after the first such treatment was approved in the United States, the simple 8- to 12-week oral cure is not reaching a significant fraction of the more than 2.4 million US residents chronically infected with hepatitis C.1 More than 15 000 US residents die of hepatitis C every year unnecessarily. In its fiscal year 2024 budget proposal, the Biden-Harris administration has put forward a bold 5-year program to put the nation on course to eliminate hepatitis C in the United States.
The consequences of untreated hepatitis C can be severe: cirrhosis, liver failure, hepatocellular cancer, and death.
Curative treatment stops transmission, prevents liver cancer and liver failure, and saves lives. It is even likely to be cost-saving, by avoiding expensive medical treatments for liver failure and liver cancer. So why is this not a public health success story? One major reason is that many people with hepatitis C have poor access to health care and experience other chronic health and social inequities. Hepatitis C disproportionately affects individuals without insurance, American Indian and Alaska Native persons, non-Hispanic Black persons, justice-involved populations, and people who use illicit drugs.2
Treatment requires diagnosis, but only an estimated 40% of those chronically infected with hepatitis C are aware of their infection.3
Screening for hepatitis C is recommended by the Centers for Disease Control and Prevention and the US Preventive Services Task Force for all adults, pregnant persons, and anyone with identified risk factors, but uptake in practice has been limited. One major limitation is that testing for hepatitis C now requires 2 steps: initiating treatment starts with an antibody test to detect prior infection, followed by an RNA test to determine whether infection is active. Return of those test results can take days or weeks, and then a third visit is needed to initiate treatment.
Among those diagnosed, hepatitis C treatment coverage is far below what is needed to achieve elimination goals.
Only about one-third of people diagnosed with hepatitis C who have private insurance, Medicare, or Medicaid get treated, and the proportion is probably even lower for those without insurance.4 This is in part due to current restrictions, such as requirements for patient sobriety, requirements to document evidence of liver fibrosis, and the restriction of access to treatment only to those seen by specialists, that have been put in place by public and private insurers in reaction to the high cost of DAAs ($90 000 per patient initially, still around $20 000). Low rates of treatment may also reflect the complexity of traversing the full cascade of care in our health care delivery system.
Addressing this missed opportunity can save both lives and money. A national effort can build on lessons from programs launched by jurisdictions such as the states of Louisiana and Washington, the Cherokee Nation, the Veterans Health Administration, and the Federal Bureau of Prisons.
For example, the Veterans Health Administration has treated more than 92 000 veterans with hepatitis C virus since 2014, with cure rates exceeding 90%.5
A key lesson from these initiatives is that success requires both managing the cost of the medications and developing a comprehensive public health effort to identify persons with hepatitis C and link them to care.
To bring these efforts to a national scale, the Biden-Harris administration is calling on Congress to embrace its proposed 5-year program to eliminate hepatitis C in the United States.
This program was developed through extensive consultations with key stakeholders within and outside government, including patient groups, physician groups, and federal agencies. The program aims to significantly expand screening, testing, treatment, prevention, and monitoring of hepatitis C infections in the United States, with a specific focus on populations at the greatest risk for infection. Hepatitis C is the most common cause of liver cancer today, so this initiative is an important contribution to President Biden’s Cancer Moonshot.
The national program has 3 main priorities:
1.First, accelerating the availability of point-of-care (POC) diagnostic tests.
Currently, POC hepatitis C RNA diagnostic tests are available outside of the United States, empowering a test-and-treat approach in a single visit. The administration proposal will support the Independent Technology Assessment Program, a collaboration between the Food and Drug Administration and the National Institutes of Health, to speed up clearance or approvals for such tests, just as was done by this same group for COVID-19 POC tests.6 The availability of such POC tests will be game-changing for hepatitis C single-visit programs, particularly in high-impact settings such as community health centers, substance use disorder treatment clinics, correctional facilities, emergency departments, and mobile vans.
2.Second, the program aims to provide broad access to curative hepatitis C medications.
A key element will be a national subscription model to purchase DAAs for those who are particularly underserved today: Medicaid beneficiaries, justice-involved populations, people without insurance, and American Indian and Alaska Native individuals who are treated through the Indian Health Service. With this approach to drug purchasing pioneered in Louisiana,7 the federal government will negotiate with manufacturers to purchase as much treatment as needed for all individuals in the designated groups. The pharmaceutical industry can expect more revenue for DAAs for these populations than it is receiving today, but at a much lower per-patient cost. That’s a win-win. Beyond the subscription model, the program will seek to provide additional co-pay assistance to Medicare beneficiaries. Private insurers will also be strongly encouraged to increase coverage for hepatitis C testing and treatment and limit out-of-pocket costs where possible.
3.Third, the program will include a comprehensive public health effort to engage, inform, identify, and treat people with hepatitis C.
By supporting grassroots organizations and trusted community partners, the effort will build trust and create the conditions for more people to seek testing and care. The program will support universal screening as part of routine care and will seek to diversify testing locations available, including by using networks of pharmacies where possible. To build the infrastructure for treatment, the program will scale up training programs for clinicians, including physicians, nurse practitioners, and physician assistants, using innovative models such as the Extension for Community Healthcare Outcomes program. These clinicians will staff a growing network of treatment sites, many of which will be able to offer expedited test-and-treat services. Innovative models of care to be explored include mobile treatment, treatment through telehealth, treatment in primary care, and advanced pharmacy practice models with support from physician specialists. Recognizing the multiple needs of individuals with hepatitis C, the program will support community access sites, including federally qualified health centers, and use of case managers, community health workers, and perinatal case coordinators to link patients to treatment and other needed services. The program also seeks to reenergize vaccine research, which might be accelerated by the advent of the mRNA platform.8 Hepatitis C can spread rapidly through a susceptible population of people who inject drugs, and DAAs do not prevent reinfection. But with access to preventive and harm-reduction services, reinfection after treatment is uncommon. Still, a vaccine will be the best insurance for the future.
Leadership for the program will be housed at the Office of the Assistant Secretary of Health in the Department of Health and Human Services to ensure critical effective coordination between key federal agencies, including the Centers for Disease Control and Prevention, Centers for Medicare & Medicaid Services, Food and Drug Administration, Health Resources and Services Administration, Indian Health Service, National Institutes of Health, and Substance Abuse and Mental Health Services Administration. A vigorous communication plan will be developed to launch the national program, including awareness campaigns for clinicians and the public, designed in coordination with affected communities. Real-time tracking of testing and treatment will allow for close monitoring of implementation and adjustment as needed. The costs of this outreach effort will reach several billion dollars over 5 years — a sizable investment, but less than the savings that economists project would be generated in the future by preventing tens of thousands of expensive cases of liver failure and liver cancer. Recent data also showed that the benefits of treating hepatitis C extend beyond liver disease to diabetes and kidney disease, making the savings from cures likely to be even greater.9
It is rare to have the opportunity, using a simple and safe oral medication, to eliminate a lethal disease. But that is the situation facing the United States with hepatitis C. Congressional support can make possible a historic public health initiative that can prevent suffering, save lives, and ultimately save money — to the benefit of all US residents. How can we not do this?
Originally published at https://jamanetwork.com




