the health strategist
research and strategy institute for continuous transformation
in value based health, care and tech
Joaquim Cardoso MSc
Chief Researcher & Editor
March 26, 2023
EXECUTIVE SUMMARY
Private technology companies are working with the UK’s National Health Service (NHS) to find ways to reduce costs and meet environmental targets.
- The partnership has already seen a mobile phone app created by TestCard and Guy’s and St Thomas’s NHS trust being used to trial the world’s first dual Covid and flu test.
- Meanwhile, MediMusic is working on a bespoke algorithm that identifies pieces of music proven to deliver health benefits, with one trial suggesting it could reduce care home stress management costs from £1,125 per resident per year to just £120.
However, funding and regulatory burdens are hampering the impact of some partnerships, with some concerned about data privacy.
DEEP DIVE
Can private tech groups reduce cost pressures on Britain’s NHS?
Financial Times
March 25, 2023
A new app that turns a mobile phone into a clinical-grade scanner is easing pressure on one of the UK’s busiest emergency departments, while another company is using music to treat anxiety and soothe pain, reducing drug bills.
Across the health and care sector, new partnerships with technology companies are being forged with the aim of cutting costs as well as contributing to wider environmental goals.
However, scarce resources and sometimes cumbersome regulatory requirements are hampering their impact, according to those in the sector, despite growing evidence that such innovations are reducing strain on services.
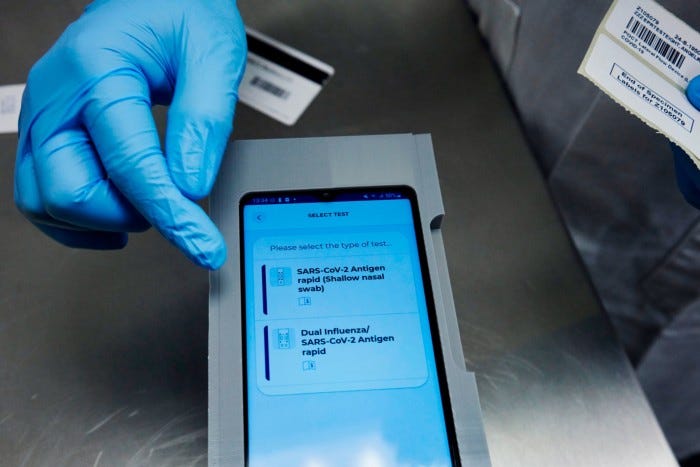
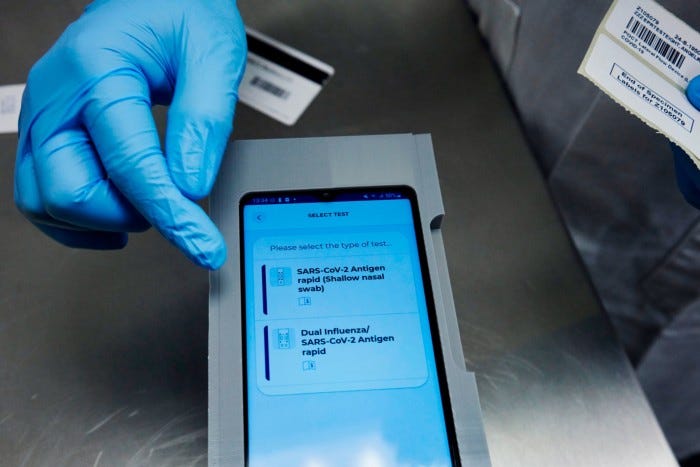
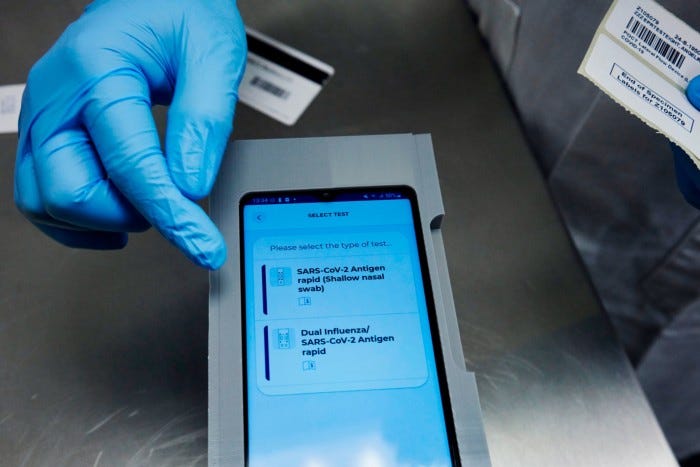
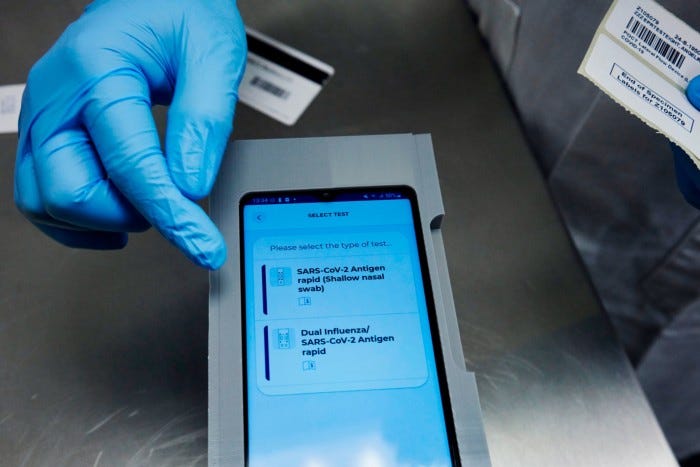
The testing application called ClearScreen, which can be installed on a smartphone has been developed by TestCard, a British diagnostics company, in collaboration with Guy’s and St Thomas’s, a large London NHS trust.
During the course of a trial, started in 2021, the app has proved so effective that staff are now using it to trial the world’s first dual Covid and flu test, developed by Derby-based SureScreen Diagnostics and piloted by the NHS trust.
Clinicians say that by identifying infected people faster, the scanner helps to stop disease spreading within the hospital. A swift diagnosis can also spare patients waiting hours in A&E to find out whether they have tested positive, limiting bottlenecks.
The partnership began early in the coronavirus pandemic in 2020, explained Dr Rahul Batra, deputy director for the Centre for Clinical Infection and Diagnostics Research at the trust. It had initially partnered with SureScreen Diagnostics, a UK-based manufacturer of lateral-flow tests, to develop a Covid antibody test.
Batra said working with two British companies had been “great . . . because it’s given us the ability and the insight to rapidly make changes” to the technology. “I think that type of partnership is really important for the future of the NHS.”
MediMusic, a Hull-based company that aims to use music to lift depression and ease pain, is another example of a company that is forging links with individual hospitals to reduce NHS costs.
Chief executive and co-founder Gary Jones said it had developed a bespoke algorithm that identified pieces with a specific timbre and tempo proven to deliver health benefits.
Over a period of 20 to 25 minutes, a playlist could reduce heart rate and production of the stress hormone cortisol, and improve cognitive response, among other positive results.
Jones said one trial, conducted by University College London, showed the cost of managing stress in care home residents could be cut from about £1,125 per resident a year to around £120 when MediMusic’s technology was deployed.
He said this amounted to an 86 per cent return on investment and a potential saving of millions to larger care home groups.
“We have a ‘biofeedback loop’. So if someone’s wearing a heart rate monitor and they don’t respond the way that we expect, we can dynamically swap out tracks to bring the heart rate down at a faster rate.”
The approach is currently being piloted in five care home groups and two large hospitals, and negotiations are under way with another three trusts.
Another study had shown a 23.8 per cent reduction in the prescription of anxiolytics, a class of drugs used to prevent or treat anxiety symptoms or disorders, for patients who received this kind of musical therapy.
This in turn helped to diminish the sector’s carbon footprint, he argued, pointing out the pharmaceutical industry was among the largest emitters of greenhouse gases.
However, while tech solutions can provide useful tools to ease pressure on overstretched NHS resources, tech entrepreneurs say a lack of funding in the cash-strapped service is holding back their potential.
Oxehealth, a business founded in 2012 by Professor Lionel Tarassenko as an Oxford university spinout, installs infrared cameras in mental health patients’ rooms to reduce falls, self-harm and provide other monitoring.
The company’s technology, Oxevision, is present in almost half of English NHS mental health trusts. Research by York Health Economics Consortium, funded by Oxehealth, estimated the technology could save NHS England mental health trusts more than £80mn a year by reducing spending on agency staff and other costs.
Although Oxevision said installation expenses can be recouped through savings, they are a barrier for some trusts. Fitting the tech costs £1,682 per room on a yearly basis, according to the company’s 2021 accounts.
“Where you have a trust that’s really facing financial difficulties, you can get trapped in this life and limb spending,” said Hugh Lloyd-Jukes, Oxehealth’s chief executive. “Very modest funding that . . . could come in becomes a struggle.”
NHS partnerships with the tech sector have also sparked concerns over data privacy.
Camden and Islington NHS Foundation Trust said it discontinued its use of Oxevision last year after patients said the constant monitoring could be harmful for survivors of abuse.
“No other NHS Trusts discontinued the use of Oxevision due to the decision,” Oxehealth said.
Other companies have struggled to monetise their work with the NHS.
Babylon, the telemedicine company behind GP at Hand app, has wound down UK operations to instead focus on the more lucrative US market.
At MediMusic, Jones lamented a lack of “segmentation” that meant all digital technology, from an app “right the way through to high end robotics”, had to bear the same burden of regulatory compliance. In the US, in contrast, burdens varied according to the complexity of the intervention, he suggested.
He welcomed an announcement by chancellor Jeremy Hunt this month that the UK medicines regulator, the MHRA, would from next year “allow rapid, often near automatic” sign-off for technologies already approved by trusted regulators elsewhere and would set up a fast new approval process for the most cutting-edge devices.
The NHS said it was “already leading the world in developing and adopting innovations which improve patient care”.
“Thanks to partnerships with industry, we have led the way in achieving the world’s first ever net zero cancer operation, we have delivered chemotherapy drugs by drone and the NHS has the UK’s first hospital capable of being powered completely by solar energy.”
Originally published at https://www.ft.com on March 26, 2023.
Names mentioned
- Dr Rahul Batra, deputy director for the Centre for Clinical Infection and Diagnostics Research at the trust.
- Chief executive and co-founder Gary Jones
- Professor Lionel Tarassenko as an Oxford university
- Jeremy Hunt