Cancer Moonshot 2.0
The Lancet
David B Agus, Elizabeth M Jaffee, Chi Van Dang,
January 19, 2021 (republication)
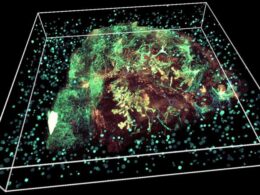
Copyright © 2021 James King-Holmes/Science Photo Library
Cancer moonshot 1.0 !
In his final State of the Union address on Jan 12, 2016, former President Barack Obama asked former Vice President Joe Biden to lead a new national effort — the Cancer Moonshot initiative …
… to accelerate research in cancer prevention, diagnosis, and treatment with the aim of making 10 years’ worth of progress in just 5 years.
In response, Biden convened a Cancer Moonshot Task Force that established a Blue Ribbon Panel charged with developing recommendations for a roadmap of research priorities to achieve Moonshot’s goals.
Together with the input from thousands of patients with cancer, caregivers, clinicians, scientists, advocacy groups, health organisations, technologists, and industry leaders, the Blue Ribbon Panel delivered their report on Oct 17, 2016.
Subsequently, Congress passed the 21st Century Cures Act on Dec 13, 2016, which authorised US$1·8 billion in funding to the National Cancer Institute (NCI) for the Cancer Moonshot initiative over 7 years.
In 2017, a Lancet Oncology Commission on future cancer research priorities in the USA was established to build and elaborate on the recommendations made in the Blue Ribbon report; the results of this Commission were published on Nov 1, 2017.1
The achievements!
Since the launch of the Cancer Moonshot initiative, the NCI has implemented initiatives to advance research in immuno-oncology, cancer drug sensitivity and resistance, childhood cancers, patient engagement, cancer health disparities, and clinical implementation science,
and has funded the Human Tumor Atlas Network.
These efforts have resulted in more than 70 initiatives, 240 new projects, and 69 million hours of analysis between 2013 and 2020 in the data sharing ecosystem, with more than 70 000 users per month.
The venture has successfully established scientific priorities and frameworks for clinical trial networks and design, for the development and use of data standards and community research practices, and has fostered collaboration between cancer researchers from across the USA.
Although COVID-19 has slowed some areas of progress, others have continued at a brisk pace.
The gaps and the opportunities!
Although these efforts have yielded rapid progress in the understanding, detection, and treatment of cancer and improvements in outcomes for patients, poor outcomes and a high death rate associated with cancer remains.
Numerous challenges have prevented Moonshot from reaching its full potential.
Moreover, the landscape of cancer therapies and technologies has changed markedly since the original roadmap was developed in 2016.
Cancer is a complex, dynamic system. Cause of disease, early detection, prevention, and therapies span genetic, molecular, cellular, tissue, population, environmental, and socioeconomic factors that evolve with time.
However, these changes can be traced and tracked with new technologies. A blend of statistics, mathematics, engineering, and machine learning tools used to understand tumour biology and clinical outcomes are ready to empower discovery in this data-driven age.
Advances here can lead to new methods for early detection, prevention, and treatment of cancer, and new methods of dissemination to combat existing health disparities.
For example, there is now the ability to collect, analyse, and interpret national cancer data in a standardised way. Instead of a system in which doctors and hospitals collect and analyse data ad hoc and reactively, patient data can be frequently and prospectively collected to populate structured databases in a privacy-protected way, enabling proactive management of individual patients using data gleaned from the wider patient database and interpreted by machine learning-driven and artificial intelligence-driven systems.
Nationally, health care will evolve to become a monitoring system — empowered by technology — that promotes and facilitates disease prevention, early detection, and data-driven therapy.
The most exciting part of this future is that cancer care outcomes will be democratised through lower costs and greater accessibility.
Crucially, this future can only happen with federal leadership: to establish cloud-based repositories, set data standards, ensure privacy protection, and incentivise data sharing.
Crucially, this future can only happen with federal leadership: to establish cloud-based repositories, set data standards, ensure privacy protection, and incentivise data sharing.
Republication from last year!
The inauguration of President-elect Biden on Jan 20, 2021, provides such an opportunity for federal leadership and investment in the Cancer Moonshot initiative.
But more than just building on the momentum and progress of the past 7 years, we must expand and amplify this progress.
Therefore, we hereby announce the formation of a team to undertake a second Moonshot Commission for The Lancet Oncology to accomplish goals left incomplete and address new challenges for this new era.
We have identified several research areas that warrant prioritisation in a Moonshot 2.0 initiative, including
- new database formats to capture and disseminate biological data linked to disease cause,
- patient clinical characteristics, and response to treatments;
- new technologies that generate patient-specific and tumour-specific information to identify potential vulnerabilities for exploitation with precision medicines;
- machine learning innovations that link the molecular structure of cancer pathways to more specific and effective drugs (as shown with a new targeted therapy against a specific KRAS mutation in lung cancer);
- new drug delivery systems that target specific cancer vulnerabilities, such as bispecific antibodies, nanotechnologies, microspheres and microchips, and cellular engineered products;
- enhanced molecular imaging, which specifically targets cancer cells and is sensitive enough to identify premalignant or early malignant cells that are readily treatable;
- and non-invasive liquid biopsy approaches that can be used to screen high-risk individuals to identify precancers and early cancers, and to follow cancers during the clinical course.
Insights in basic and translational research can feed back to clinical trials, leading to advances in clinical care.
Research in these priority areas could also identify ways to take advantage of real-world data and facilitate access to quality care for individuals in low socioeconomic and rural areas who have received a disproportionately lower benefit from advances during the past 7 years.
We have a long way to go to lessen the burden of cancer worldwide.
To achieve the true Cancer Moonshot vision for improved care of and outcomes for patients with cancer, efforts must be scaled up, redoubled, and accelerated.
Most importantly, the advances in care these efforts will generate, must be representative of, and accessible to, all Americans — regardless of age, gender, race, and ethnicity.
To achieve the true Cancer Moonshot vision for improved care of and outcomes for patients with cancer, efforts must be scaled up, redoubled, and accelerated.
About the authors
DBA is a member of the board of directors for and reports equity in Project Ronin, and is a scientific advisory board member for and reports equity in Tempus, outside the submitted work.
EMJ reports grants from Lustgarten Foundation, and Bristol Myer Squibb; is the co-founder of Abmeta Therapeutics; and is an unpaid scientific advisory board member for Aduro Biotech, Genocea, Adaptive Biotech, Dragonfly Therapeutics, CSTONE Therapeutics, Achilles Therapeutics, Medically Home, and Parker Institute, outside of the submitted work.
CVD reports no competing interests.
References
See the original publication: https://www.thelancet.com