The Lancet
Guy G Brusselle, Marc Humbert
September 05, 2022
Site editor:
Joaquim Cardoso MSc.
Health Transformation Review
September 7, 2022
Chronic obstructive pulmonary disease (COPD) is a highly prevalent and heterogeneous chronic disease of the lower airways and lungs …
… that is associated with huge morbidity, disability, and mortality worldwide and disproportionately affects poor and vulnerable people. 1
Pathologically, COPD is characterised by variable degrees of chronic inflammation and remodelling of small airways (bronchiolitis) and destruction of alveolar walls (emphysema). 2
Diagnosis of COPD relies on respiratory symptoms and the presence of spirometric airflow limitation. 3
COPD has long been considered a self-inflicted disease that occurs in adult cigarette smokers as a result of accelerated decline in lung function. 4
However, epidemiological evidence has shown that many other factors, including indoor and outdoor air pollution, occupational exposures, and use of e-cigarettes and cannabis, also cause COPD.
Furthermore, in addition to accelerated lung function decline in adulthood, several other lung function trajectories — characterised by impaired lung development in utero or impaired lung growth in early life — have been linked to COPD. 5
Indeed, COPD can be elicited by early-life events such as prematurity, childhood asthma, and childhood respiratory infections.
Importantly, tuberculosis and HIV — common chronic infections, especially in low-income and middle-income countries — can lead to airway obstruction and COPD.
Finally, although COPD is a complex disease caused by multiple gene–environment interactions throughout the life course, it is mainly genetically determined in specific subgroups of patients with early-onset COPD or a positive family history (eg, people with α1 antitrypsin deficiency).
COPD has long been considered a self-inflicted disease that occurs in adult cigarette smokers as a result of accelerated decline in lung function.
However, epidemiological evidence has shown that many other factors, … also cause COPD.
Because the causes, pathogenesis, clinical presentation, prognosis, and response to treatment in COPD are so heterogeneous, there is a major need to expand and refine the classification of COPD.
In the Lancet Commission on COPD, Daiana Stolz and colleagues 6 provide an excellent comprehensive review of the epidemiology and pathophysiology of COPD, and discuss the challenges for optimal prevention, diagnosis, and treatment.
Importantly, they propose a novel classification of COPD encompassing five types based on the predominant risk factors driving the disease (panel). This classification of COPD, if disseminated and implemented urgently and globally, could foster prevention, drug development, and clinical management of COPD.
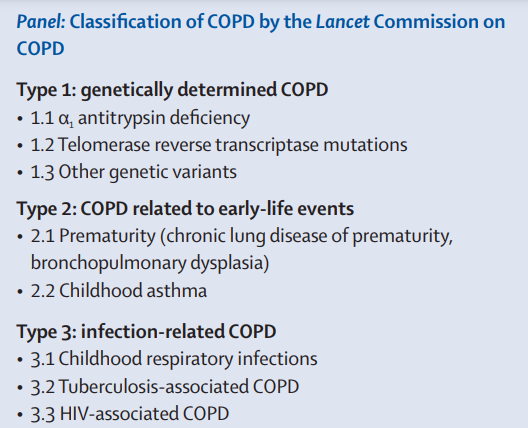
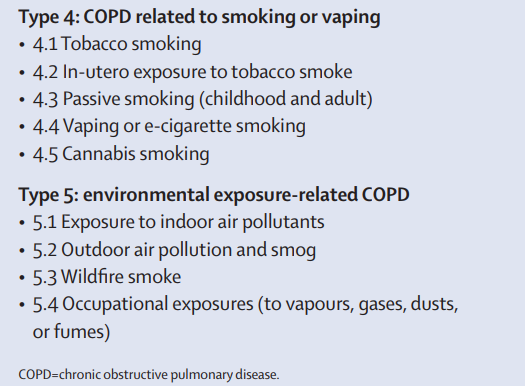

By raising awareness of the detrimental role of early-life events, infections, and air pollution (in addition to smoking and vaping) in the pathogenesis of COPD, 7 the Commission underlines ample opportunities for prevention of COPD by protecting lung health throughout the life course.
- To eliminate COPD worldwide, it is crucial to prohibit all kinds of smoking and to reduce exposure to indoor and outdoor pollutants.
- Clean air is essential to respiratory health.
- Levels of outdoor air pollutants should be decreased as advocated by the WHO Air Quality Guidelines, 8 because exposure even to low or moderate environmental air pollution is associated with adverse effects on respiratory health, especially in vulnerable people (eg, children and pregnant people).
- Reducing the use of biomass fuel for cooking and heating in poorly ventilated houses in low-income and middle-income countries will also have major public health benefits.
- Prevention of premature birth, childhood infections, tuberculosis, and HIV are other important preventive strategies to reduce the burden of COPD globally.
By raising awareness of the detrimental role of early-life events, infections, and air pollution (in addition to smoking and vaping) in the pathogenesis of COPD, …
the Commission underlines ample opportunities for prevention of COPD by protecting lung health throughout the life course.

The Commission’s classification of COPD will also facilitate novel therapeutic strategies and drug development.
Indeed, the current Global Initiative for COPD (GOLD) classification of COPD severity is based on the degree of dyspnoea and the frequency of exacerbations (acute episodes of worsening symptoms). 3
However, because symptoms are non-specific and not linked to precise underlying pathogenetic pathways, this classification system and the tendency to treat COPD as an irreversible, end-stage disease have hampered therapeutic innovation in COPD. 9
In severe asthma, by contrast, elucidation of the driving mechanisms of disease has led to major breakthroughs in management (eg, targeted treatment with monoclonal antibodies in specific phenotypes). 10
Stolz and colleagues’ work in the Commission is an important step in discerning the diverse pathophysiological mechanisms of COPD, and paves the way towards novel treatments specifically tailored to disease type.

The Lancet Commission on COPD is reminiscent of the successful approach taken in other fields of medicine in which refined classifications have allowed for substantial advances and improved management of patients with conditions that can be driven by multiple distinct mechanisms.
One example in respiratory medicine is pulmonary hypertension, which was the focus of WHO meetings in 1960 on cor pulmonale and in 1973 on primary pulmonary hypertension.
The clinical classification of pulmonary hypertension has been developed and refined since these pioneer proposals.
Conditions associated with pulmonary hypertension are grouped on the basis of broadly similar pathomechanisms, clinical presentations, haemodynamic findings, and management. 11

In the past 50 years, this classification has evolved alongside scientific knowledge and provided a strong basis for successful therapeutic innovations in group 1 (pulmonary arterial hypertension) and group 4 (chronic thromboembolic pulmonary hypertension) disease.
Of note, group 3 pulmonary hypertension associated with lung diseases including COPD is the focus of active research, which could benefit greatly from the advances triggered by the Lancet Commission on COPD.
In summary, it is time to complement the GOLD symptom-based classification of COPD severity with the Lancet Commission’s subtype classification of the disease, which would offer many opportunities for prevention, therapeutic innovation, and precision medicine.
As in pulmonary hypertension, this classification will need regular updating, to incorporate novel pathogenetic insights and to foster efficacious preventive and therapeutic strategies.
The ultimate aim is to eliminate COPD, a preventable disease.
The ultimate aim is to eliminate COPD, a preventable disease.
Disclaimers
GGB has received payments from AstraZeneca, Boehringer-Ingelheim, Chiesi, GlaxoSmithKline, Merck Sharp & Dohme, Novartis, and Sanofi for advisory boards and lectures on asthma, COPD, interstitial lung disease, and chronic cough.
MH declares payments for advisory boards or lectures on asthma or pulmonary hypertension from Acceleron, Aerovate, Altavant, AOP Orphan, AstraZeneca, Bayer, Chiesi, Ferrer, GlaxoSmithKline, Janssen, Merck, MorphogenIX, Novartis, Sanofi, Shou Ti, and United Therapeutics, and grants to his institution from Acceleron, AOP Orphan, Janssen, Merck, and Shou Ti.
References
See the original publication
Originally published at https://www.thelancet.com.
ORIGINAL PUBLICATION (reference)