OECD
Francesca Colombo
09/11/2021
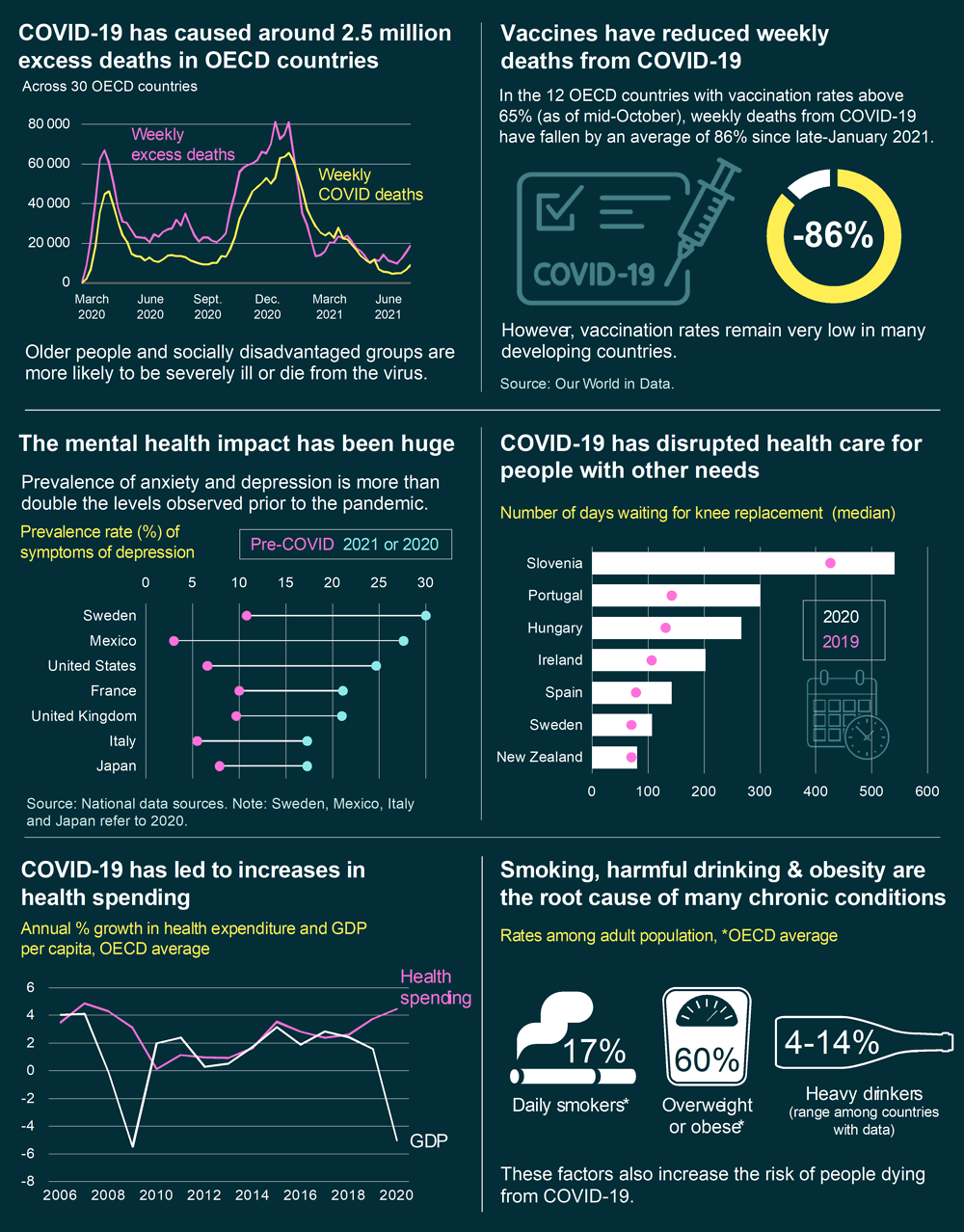
09/11/2021 — COVID‑19 contributed to a 16% increase in the expected number of deaths in 2020 and the first half of 2021 across OECD countries.
Life expectancy fell in 24 of 30 countries with comparable data, with drops particularly large in the United States (‑1.6 years) and Spain (‑1.5 years), according to a new OECD report.
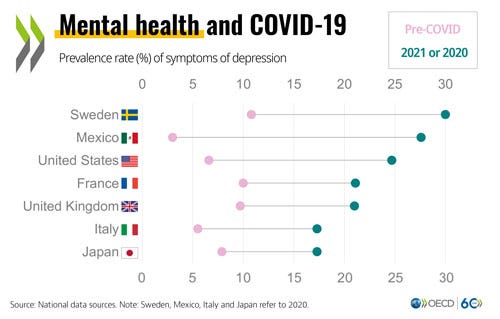
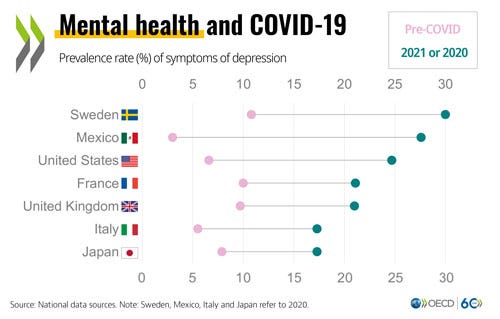
OECD Health at a Glance 2021 says that the mental health impact of the pandemic has been huge, with prevalence of anxiety and depression more than double levels observed pre-crisis in most countries with available data, most notably in Mexico, the United Kingdom and the United States.
COVID‑19 has also had a major indirect impact on people not infected with the virus.
For example, breast cancer screening fell by an average of 5 percentage points in 2020 compared to 2019, across OECD countries with available data.
The median number of days on a waiting list increased on average by 58 days for hip replacement, and 88 days for knee replacement in 2020, as compared to 2019.
The COVID-19 pandemic has led to a sharp increase in health spending across the OECD.
Coupled with reductions in economic activity, the average health spending to GDP ratio jumped from 8.8% in 2019 to 9.7% in 2020, across OECD countries with available data.
Countries severely affected by the pandemic reported unprecedented increases.
The United Kingdom estimated an increase from 10.2% in 2019 to 12.8% in 2020, while Slovenia anticipated its share of spending on health rising from 8.5% to more than 10%.
The pandemic highlights the persistent shortage of health workers stressing the importance of investing more in the years ahead on improving primary care and disease prevention and strengthen the resilience and preparedness of health systems.
Indeed, the report says that health spending continues to focus mainly on curative care rather than disease prevention and health promotion, and much more is spent on hospitals than on primary health care.
Prior to the pandemic, spending on health amounted to over USD 4 000 per person on average across OECD countries, reaching almost USD 11 000 in the United States.
Inpatient and outpatient services make up the bulk of health spending, typically accounting for 60% of all health spending.
Although the number of doctors and nurses have increased over the past decade in nearly all OECD countries, shortages persist.
The lack of health and long-term care staff is proving to be more of a binding constraint than hospital beds and equipment, says the report.
The pandemic has also underscored the impact of unhealthy lifestyles, with smoking, harmful alcohol use and obesity increasing the risk of people dying from COVID-19.
Yet spending on disease prevention remains relatively low, accounting for only 2.7% of all health spending on average.
Despite daily smoking rates decreasing in most OECD countries over the last decade, 17% still smoke daily.
Rates reached 25% or more in Turkey, Greece, Hungary, Chile and France.
People who drink heavily range from 4% to 14% of the population across the OECD countries analysed, yet consume 31% to 54% of alcohol.
Harmful drinking is particularly high in Latvia and Hungary.
Obesity rates continue to rise in most OECD countries, with an average of 60% of adults measured as overweight or obese.
Obesity rates are highest in Mexico, Chile and the United States.
EXECUTIVE SUMMARY OF THE REPORT
Executive summary
COVID-19 has generated enormous human, social and economic costs, and revealed the underlying fragilities of many health systems to withstand shocks. The pandemic has claimed millions of lives, with many more suffering ill-health as a direct or indirect consequence of the virus. It has placed immense pressure on health care services that were often already overstretched before the pandemic. The pandemic has also shown that effective health spending is an investment, not a cost to be contained: stronger, more resilient health systems protect both populations and economies.
At the same time, additional health spending and COVID-related debt will weigh heavily on budgets, and require careful scrutiny to maximise value for money. Health spending continues to focus predominantly on curative care rather than disease prevention and health promotion, and much more is spent in hospitals than on primary health care. Moving forward, it is imperative to strengthen the resilience and preparedness of health systems, Encouraging signs point to the potential for systemic change, with advances in digital health and better integrated care.
Key Points (summarized by the editor of the blog)
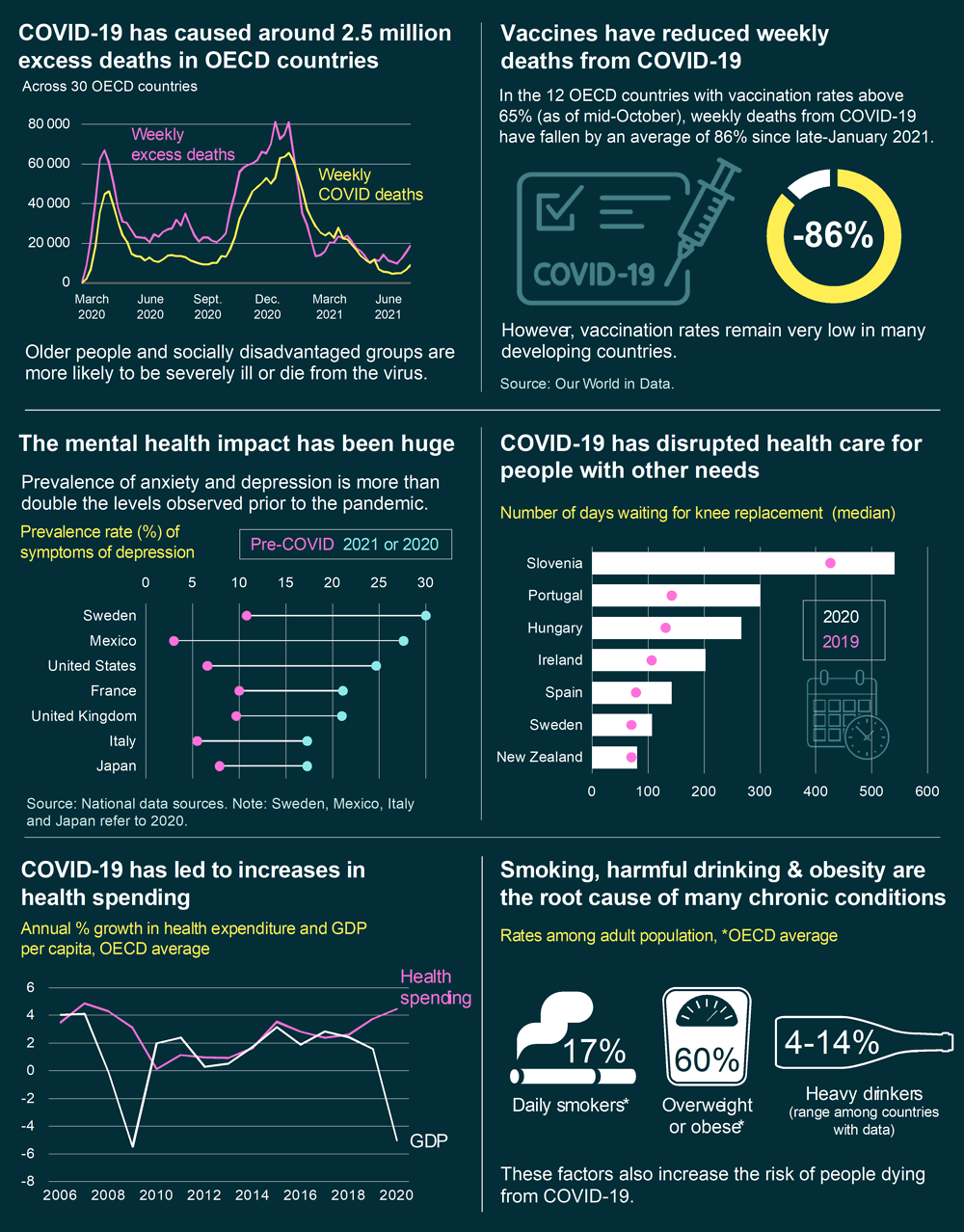
- COVID-19 has caused around 2.5 million excess deaths in OECD countries and had a major adverse impact on mental health
- Unhealthy lifestyles and poor environmental conditions continue to worsen quality of life, cut lives short and make populations less resilient to health shocks
- Despite universal health coverage in most OECD countries, barriers to access persist, with COVID-19 disrupting health care for people with other needs
- Quality of care is improving in terms of safety and effectiveness, and more attention is being placed on patient-reported outcomes and experiences
- COVID-19 has led to sharp increases in health spending, but health workforce shortages persist
COVID-19 has caused around 2.5 million excess deaths in OECD countries and had a major adverse impact on mental health
- COVID-19 contributed, directly and indirectly, to a 16% increase in the expected number of deaths in 2020 and the first half of 2021 across OECD countries. Life expectancy fell in 24 of 30 countries with comparable data, with drops particularly large in the United States (-1.6 years) and Spain (-1.5 years).
- COVID-19 has disproportionately hit vulnerable populations. More than 90% of recorded COVID-19 deaths have occurred among those aged 60 and over. There has also been a clear social gradient, with disadvantaged people, those living in deprived areas, and most ethnic minorities and immigrants at higher risk of infection and death.
- Vaccinations have reduced the risk of severe illness and death from COVID-19, with the share of people fully vaccinated reaching over 70% in 9 countries and 15 countries starting booster programmes across the OECD for vulnerable groups, as of 18 October. Evidence points to vaccines being somewhat less effective against stopping symptomatic disease from the delta variant, but still highly effective (over 90%) against hospital admissions.
- The mental health impact of the pandemic has been huge, with prevalence of anxiety and depression more than double levels observed pre-crisis in most countries with available data, most notably in Mexico, the United Kingdom and the United States.
- Long COVID-19 has made the road to recovery slow and difficult. In the United Kingdom, for example, 1.1 million people (1.7% of the population) reported long COVID-19 symptoms as of early September 2021. In the United States, recent research has estimated that 37% of patients suffered from at least one long COVID-19 symptom 4–6 months after diagnosis.
Unhealthy lifestyles and poor environmental conditions continue to worsen quality of life, cut lives short and make populations less resilient to health shocks
- Smoking, harmful alcohol use and obesity are the root cause of many chronic conditions, and increase the risk of people dying from COVID-19.
- Daily smoking rates have decreased in most OECD countries over the last decade, but 17% still smoke daily. Rates reached 25% or more in Turkey, Greece, Hungary, Chile and France.
- People who drink heavily range from 4% to 14% of the population across the OECD countries analysed, yet consume 31% to 54% of alcohol. Harmful drinking is particularly high in Latvia and Hungary.
- Obesity rates continue to rise in most OECD countries, with an average of 60% of adults measured as overweight or obese. Obesity rates are highest in Mexico, Chile and the United States.
- Among adolescents, about 16% of 15-year-olds smoked at least once per month, and over 30% had been drunk at least twice in their lifetime, on average across OECD countries. Just over 18% were overweight or obese, with only 14% achieving WHO recommendations on physical activity.
- Ambient (outdoor) air pollution caused about 29 deaths per 100 000 people on average, and varied more than seven-fold across OECD countries. OECD projections estimate that ambient air pollution may cause between 6 and 9 million premature deaths a year worldwide by 2060.
- Spending on disease prevention remains relatively low, accounting for only 2.7% of all health spending on average.
Despite universal health coverage in most OECD countries, barriers to access persist, with COVID-19 disrupting health care for people with other needs
- COVID-19 has had a major indirect impact on those not infected with the virus. For example, breast cancer screening fell by an average of 5 percentage points in 2020 compared to 2019.
- Waiting times for elective surgeries, already a policy issue in many countries pre-pandemic, increased. The median number of days on a waiting list increased on average by 58 days for hip replacement, and 88 days for knee replacement in 2020, as compared to 2019.
- In-person consultations per capita dropped in seven of eight countries with 2020 data, and by up to 30% in Chile and Spain. However, declines in in-person consultations were offset to some extent by increased teleconsultations.
- Indeed, the pandemic has accelerated the digital transformation of health care across OECD countries. For example, an average of 45% of adults had a medical teleconsultation in 2021. Further, around 60% of adults searched for health information online in 2020, up from 36% in 2010.
Quality of care is improving in terms of safety and effectiveness, and more attention is being placed on patient-reported outcomes and experiences
- Despite improvements in patient safety over time, on average almost half of hospital staff thought that their workplace was not good enough at preventing medical errors.
- Strong primary care systems keep people well and treat most uncomplicated cases. They also relieve pressure on hospitals: avoidable admissions for chronic conditions have fallen in most OECD countries over the past decade, with large improvements in Korea, Lithuania and the Slovak Republic. However, primary care represents only 13% of health spending on average.
- Acute care services continue to improve in their fundamental task of keeping people alive. In almost every OECD country, 30-day mortality following a heart attack or stroke is lower than ten years ago. New data on readmissions, one-year mortality and medication prescriptions after hospitalisation point to slight improvements in the integration of care over time.
- A deeper understanding of quality of care requires measuring what matters to people. Health systems are increasingly asking patients about the outcomes and experiences of their care. Preliminary results show improvements in patient-reported outcomes. For example, following hip replacement, an individual’s quality of life improved on average by 44% based on the Oxford Hip Score.
- Preliminary data for 2020 indicates that quality of care in primary and acute care settings has often been maintained despite the severe pressures faced, although access to many of these services has been difficult.
COVID-19 has led to sharp increases in health spending, but health workforce shortages persist
- Prior to the pandemic, spending on health amounted to over USD 4 000 per person on average across OECD countries, reaching almost USD 11 000 in the United States. Inpatient and outpatient services make up the bulk of health spending, typically accounting for 60% of all health spending.
- With the onset of COVID-19, sharp increases in health spending occurred in many countries, notably within Europe. Coupled with reductions in economic activity, the average health spending to GDP ratio jumped from 8.8% in 2019 to 9.7% in 2020. Countries severely affected by the pandemic reported unprecedented increases in the share of GDP allocated to health. The United Kingdom, for example, estimated an increase from 10.2% in 2019 to 12.8% in 2020, while Slovenia anticipated its share of spending on health rising from 8.5% to more than 10%.
- Although the number of doctors and nurses have increased over the past decade in nearly all OECD countries, shortages persist. These shortages have been thrown into sharp relief during the pandemic, with a lack of health and long-term care staff proving to be more of a binding constraint than hospital beds and equipment.
- Population ageing increases demand for health services, with the share of the population aged 65 years and over reaching 17% in 2019. COVID-19 has underscored pre-existing weaknesses in the long-term care sector, including challenges with infection control in facility-based care.
Infographic 1. Key facts and figures
Originally published at https://www.oecd.org.
Please cite this publication as:
OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
About the authors
Health at a Glance 2021 was prepared by the OECD Health Division under the co‑ordination of Chris James.
Chapter 1 was prepared by Chris James and Gabriel Di Paolantonio;
Chapter 2 by Michael Mueller, Elina Suzuki, Gabriel Di Paolantonio, Emily Hewlett and Chris James, with research assistance from Julia Aubé;
Chapter 3 by Elina Suzuki, Gabriel Di Paolantonio, Emily Hewlett and Chris James;
Chapter 4 by Marion Devaux, Alena Piatrova and Elina Suzuki, with input from Michele Cecchini;
Chapter 5 by Chris James, Gaëlle Balestat, Marie‑Clémence Canaud, Michael Mueller, Caroline Penn, Caroline Berchet, Tiago Cravo Oliveira Hashiguchi and Jillian Oderkirk;
Chapter 6 by Katherine de Bienassis, Rie Fujisawa, Frédéric Daniel, Eliana Barrenho, Gabriel Di Paolantonio, Candan Kendir, Philip Haywood, Suzannah Chapman and Silje Rene, with input from Niek Klazinga;
Chapter 7 by Michael Mueller, Fan Xiang, Sebastian Klavus, Luca Lorenzoni and David Morgan;
Chapter 8 by Gaetan Lafortune, Gaëlle Balestat and Marie‑Clémence Canaud;
Chapter 9 by Ruth Lopert, Suzannah Chapman, Martin Wenzl, Fan Xiang and Marie‑Clémence Canaud;
Chapter 10 by Elina Suzuki, Julia Aubé, Marie‑Clémence Canaud, Paola Sillitti, Katherine de Bienassis, Michael Mueller, Tiago Cravo Oliveira Hashiguchi and Eileen Rocard, with input from Ana Llena Nozal.
Only names with no duplication
Chris James;
Alena Piatrova;
Ana Llena Nozal;
Candan Kendir;
Caroline Berchet;
Caroline Penn;
David Morgan;
Eileen Rocard Eliana Barrenho;
Elina Suzuki;
Emily Hewlett;
Fan Xiang;
Frédéric Daniel;
Gabriel Di Paolantonio,
Gaëlle Balestat,
Gaetan Lafortune,
Jillian Oderkirk;
Julia Aubé,
Katherine de Bienassis,
Luca Lorenzoni;
Marie‑Clémence Canaud,
Marion Devaux,
Martin Wenzl,
Michael Mueller,
Michele Cecchini;
Niek Klazinga;
Paola Sillitti,
Philip Haywood,
Rie Fujisawa,
Ruth Lopert,
Sebastian Klavus,
Silje Rene,
Suzannah Chapman
Tiago Cravo Oliveira Hashiguchi