Stat News
Akila Muthukumar
June 23, 2022
Executive Summary by
Joaquim Cardoso MSc.
Health Revolution — Foundation
Vaccination — Institute
June 24, 2022
Key messages
- While the pandemic has taken a devastating toll around the globe, with more than 3.5 million deaths since the first vaccine was administered in December 2020, the study estimated that vaccinations also prevented 19.8 million deaths.
- Covid-19 vaccines cut the potential global death toll by more than half in the first year they were available, according to a study published Thursday in The Lancet Infectious Diseases.
- However, millions more deaths could have been prevented. The team found that one in five of the deaths that occurred due to Covid-19 in low-income countries could have been prevented if the World Health Organization’s global vaccine targets were met.
About the study
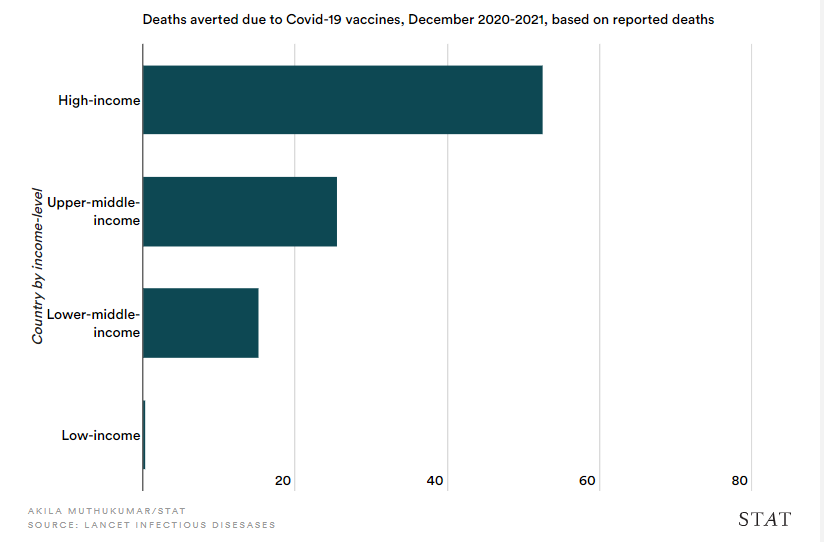
- Because many Covid deaths have not been registered or reported, particularly in low-income countries, the authors chose to look at a measure known as excess mortality, which calculates the difference between the observed and expected number of deaths in a country.
- For countries not included in the database of excess mortality that they used, the study used projections from a model developed by The Economist.
- The authors were unable to calculate excess mortality for some countries, including Iraq and Sudan.
- They also modeled the impact of vaccinations using a Johns Hopkins database of officially reported deaths. When the model was fit to these officially reported Covid deaths, they found 14.4 million deaths had been averted by vaccines, a more conservative estimate than that calculated using excess mortality.
- The actual number of deaths averted is “probably somewhere between the two, although it’s not necessarily just that simple,” according to Gregory Barnsley, a research assistant and co-first author on the study.
What are the additional benefits?
- Additionally, the study explains that while the majority of the benefit from vaccines came from direct protection — individuals are less likely to be infected or die from the disease after vaccination — there is also a degree of indirect protection.
- That is, vaccines reduce transmission in a population, relieving some strain on hospital resources and potentially, making it easier to care for the sickest patients. “A vaccination is not just for the people,” said Koum Besson. “It’s really for the health system, and for the environment.”
There are clear, if challenging, steps to improve the impact of Covid vaccines:
- scale up vaccine delivery infrastructure,
- increase vaccine confidence, and
- hold political leaders accountable for vaccine donations.

Covid-19 vaccines prevented nearly 20 million deaths in a year, study estimates
Stat News
Akila Muthukumar
June 23, 2022
Covid-19 vaccines cut the potential global death toll by more than half in the first year they were available, according to a study published Thursday in The Lancet Infectious Diseases.
The study modeled the spread of the disease in 185 territories and countries and found that without Covid vaccines, 31.4 million people would have died of the disease between December 2020 and 2021.
While the pandemic has taken a devastating toll around the globe, with more than 3.5 million deaths since the first vaccine was administered in December 2020, the study estimated that vaccinations also prevented 19.8 million deaths.
“We knew it was going to be a large number, but I did not think it would be as high as 20 million deaths during just the first year,” said Oliver Watson, a Fellow at Imperial College London and the London School of Hygiene and Tropical Medicine and co-first author on the study.
However, millions more deaths could have been prevented.
The team found that one in five of the deaths that occurred due to Covid-19 in low-income countries could have been prevented if the World Health Organization’s global vaccine targets were met.
However, millions more deaths could have been prevented.
The team found that one in five of the deaths that occurred due to Covid-19 in low-income countries could have been prevented if the World Health Organization’s global vaccine targets were met.
The team applied a Covid transmission model, incorporating what we know now about the disease and vaccines, to three situations: one in which no vaccines were available, one in which vaccines were delivered but didn’t reduce transmission, and third, the scenario that actually unfolded, with effective vaccines rolled out — in some parts of the world — in record time.
Then, they took the number of estimated Covid deaths from the first situation — if no vaccines were to exist — and subtracted the number of observed Covid deaths in the third situation to determine how many deaths were averted.
It’s an approach that assumes Covid-19 transmission looks the same across countries, which is not necessarily the case, noted Émilie Koum Besson, a research fellow at the London School who was not affiliated with the study. Still, the research offers a new look at how many lives Covid-19 vaccinations might have saved.
Because many Covid deaths have not been registered or reported, particularly in low-income countries, the authors chose to look at a measure known as excess mortality, which calculates the difference between the observed and expected number of deaths in a country.
For countries not included in the database of excess mortality that they used, the study used projections from a model developed by The Economist.
The authors were unable to calculate excess mortality for some countries, including Iraq and Sudan.
“Having estimates of excess mortality for each country was paramount to this study, and enabled us to try and better capture the true size of pandemic in many lower-income countries,” Watson said.
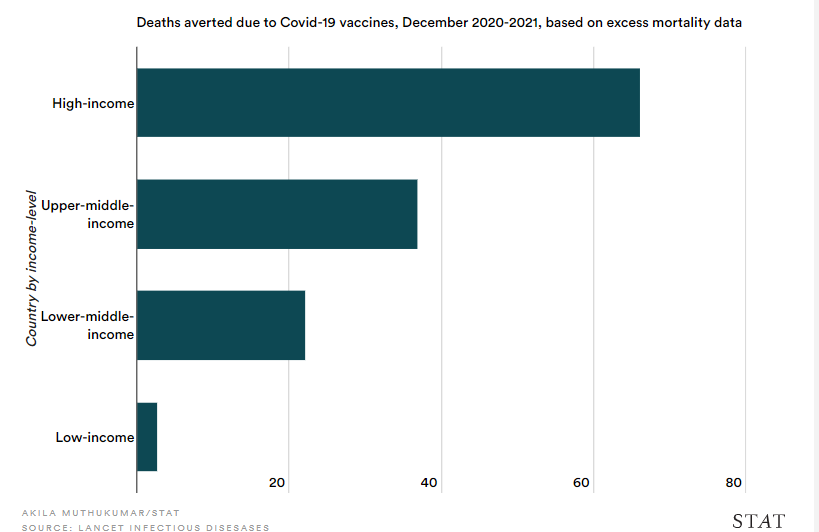
They also modeled the impact of vaccinations using a Johns Hopkins database of officially reported deaths.
When the model was fit to these officially reported Covid deaths, they found 14.4 million deaths had been averted by vaccines, a more conservative estimate than that calculated using excess mortality.
The actual number of deaths averted is “probably somewhere between the two, although it’s not necessarily just that simple,” according to Gregory Barnsley, a research assistant and co-first author on the study.
Barnsley said excess mortality could include deaths independent of Covid and that there are complications in ascertaining Covid as cause of death in people with multiple morbidities.
Additionally, the study explains that while the majority of the benefit from vaccines came from direct protection — individuals are less likely to be infected or die from the disease after vaccination — there is also a degree of indirect protection.
That is, vaccines reduce transmission in a population, relieving some strain on hospital resources and potentially, making it easier to care for the sickest patients.
there is also a degree of indirect protection.
That is, vaccines reduce transmission in a population, relieving some strain on hospital resources and potentially, making it easier to care for the sickest patients.
“A vaccination is not just for the people,” said Koum Besson. “It’s really for the health system, and for the environment.”
The team used nationally aggregated data on the rate of first and second dose vaccines and quantified vaccine efficacy based on the predominant vaccine type in each country.
All of their data and code is publicly available. Their work comes with limitations, including a lack of genetic sequencing data to confirm the frequency of circulating variants, uncertainty about vaccine efficacies, and an inability to account for how governments would likely change lockdown policies or travel restrictions.
The researchers also evaluated two additional scenarios.
The first is what would have happened if all the countries covered by the COVID-19 Vaccine Access initiative’s Advance Market Commitment — a plan incentivizing manufacturers to deliver donor-funded Covid vaccines to 92 low and middle income countries — were able to vaccinate at least 20% of their populations.
The other estimated the 40% vaccine coverage for all countries, which is the goal the WHO set forth.
They found that 41 countries failed to meet the COVAX target and 96 countries failed to meet the WHO threshold.
Koum Besson said those findings underscore the need to examine who is responsible for the shortcomings in global vaccine access — and who has the power to change them.
However, that’s challenging to examine given how little data is available from certain parts of the world.
They found that 41 countries failed to meet the COVAX target and 96 countries failed to meet the WHO threshold.
“The paper is talking about global estimates, but most of the literature and the baseline information comes from Western institutions,” she said.
Watson said there are clear, if challenging, steps to improve the impact of Covid vaccines:
- scale up vaccine delivery infrastructure,
- increase vaccine confidence, and
- hold political leaders accountable for vaccine donations.
Watson said there are clear, if challenging, steps to improve the impact of Covid vaccines: (1) scale up vaccine delivery infrastructure, (2) increase vaccine confidence, and (3) hold political leaders accountable for vaccine donations.
Originally published at https://www.statnews.com on June 23, 2022
ORIGINAL PUBLICATION
Global impact of the first year of COVID-19 vaccination: a mathematical modelling study
The Lancet Infectious Diseases
Oliver J Watson, PhD †
Gregory Barnsley, MSc †
Jaspreet Toor, PhD
Alexandra B Hogan, PhD
Peter Winskill, PhD
Prof Azra C Ghani, PhD
June 23, 2022
SUMMARY
Background
The first COVID-19 vaccine outside a clinical trial setting was administered on Dec 8, 2020.
To ensure global vaccine equity, vaccine targets were set by the COVID-19 Vaccines Global Access (COVAX) Facility and WHO.
However, due to vaccine shortfalls, these targets were not achieved by the end of 2021. We aimed to quantify the global impact of the first year of COVID-19 vaccination programmes.
Methods
A mathematical model of COVID-19 transmission and vaccination was separately fit to reported COVID-19 mortality and all-cause excess mortality in 185 countries and territories.
The impact of COVID-19 vaccination programmes was determined by estimating the additional lives lost if no vaccines had been distributed.
We also estimated the additional deaths that would have been averted had the vaccination coverage targets of 20% set by COVAX and 40% set by WHO been achieved by the end of 2021.
Findings
- Based on official reported COVID-19 deaths, we estimated that vaccinations prevented 14·4 million (95% credible interval [Crl] 13·7–15·9) deaths from COVID-19 in 185 countries and territories between Dec 8, 2020, and Dec 8, 2021.
- This estimate rose to 19·8 million (95% Crl 19·1–20·4) deaths from COVID-19 averted when we used excess deaths as an estimate of the true extent of the pandemic, representing a global reduction of 63% in total deaths (19·8 million of 31·4 million) during the first year of COVID-19 vaccination.
- In COVAX Advance Market Commitment countries, we estimated that 41% of excess mortality (7·4 million [95% Crl 6·8–7·7] of 17·9 million deaths) was averted.
- In low-income countries, we estimated that an additional 45% (95% CrI 42–49) of deaths could have been averted had the 20% vaccination coverage target set by COVAX been met by each country, and that
- an additional 111% (105–118) of deaths could have been averted had the 40% target set by WHO been met by each country by the end of 2021.
Interpretation
COVID-19 vaccination has substantially altered the course of the pandemic, saving tens of millions of lives globally.
However, inadequate access to vaccines in low-income countries has limited the impact in these settings, reinforcing the need for global vaccine equity and coverage.
Funding
Schmidt Science Fellowship in partnership with the Rhodes Trust; WHO; UK Medical Research Council; Gavi, the Vaccine Alliance; Bill & Melinda Gates Foundation; National Institute for Health Research; and Community Jameel.
Originally published at https://www.thelancet.com