In 2020 the WHO estimated there was a global shortage of 5.9mn nurses — almost one-quarter of the current global workforce of almost 28mn.
Financial Times
June 2, 2022.
Danielle Henderson, a mother of five in north-west Arkansas, quit her job as a registered nurse as Covid-19 began spreading around the world in 2020.
There weren’t enough gowns, masks and other equipment to protect her from infection, she says. “I was pregnant at the time and I just didn’t feel protected. And, mentally, I just think I was burnt out already, even before Covid.”
Henderson, who had been in her job for eight years, is one of hundreds of thousands of frontline nurses to have left a profession that was struggling to retain staff even before the pandemic struck.
In 2020 the World Health Organization estimated there was a global shortage of 5.9mn nurses — almost one-quarter of the current global workforce of almost 28mn.
By far the biggest shortfalls were in low and middle-income nations in Africa, Latin America, south-east Asia and eastern Mediterranean regions.
In 2020 the WHO estimated there was a global shortage of 5.9mn nurses — almost one-quarter of the current global workforce of almost 28mn.
The pandemic has made things worse. As many as 180,000 healthcare workers died from Covid-19 between January 2020 and May 2021, according to the WHO.
Many others suffered burnout and mental health challenges as they struggled to deal with the chaos, fear and death caused by successive waves of the highly contagious virus as it filled up intensive care units all over the world.
The pandemic has made things worse. As many as 180,000 healthcare workers died from Covid-19 between January 2020 and May 2021, according to the WHO.
Health authorities in many rich countries now warn that the departure of skilled nurses, and high levels of sick leave among frontline staff, are putting huge strains on overstretched services and reversing any progress made in recent years to boost nursing workforces.
Howard Catton, chief executive of the International Council of Nurses, a federation of more than 130 national nursing organisations, says nurses were rightly lauded as “heroes” by governments when the pandemic hit.
Even so, authorities are not doing enough, he says, to tackle structural problems such as low pay, poor conditions and inadequate training.
Meanwhile, ageing populations in the US and Europe are intensifying demand for healthcare while insufficient training opportunities in some western nations and global health budget constraints make it harder to recruit.
“The scale of the worldwide nursing shortage is one of the greatest threats to health globally,” says Catton. He estimates that as many as 3mn more nurses could leave the profession earlier than they had otherwise planned due to the pandemic.
Structure of the article
- No quick fix
- An international crisis
- Shopping for nurses
- ‘Unprecedented damage’

No quick fix
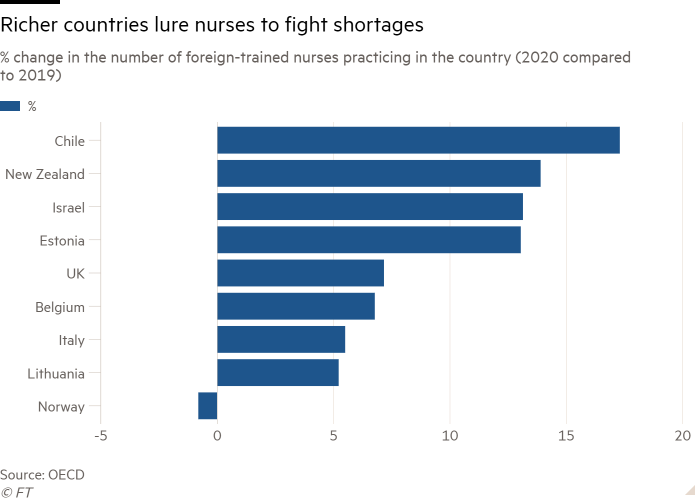
At the height of the Covid-19 crisis, several US states called on the National Guard to help in hospitals and care homes. Many other rich nations implemented “rapid and emergency policy responses” to recruit overseas nurses, which some experts warn could transform an acute shortage in the developing world into a longer-term crisis.
The Canadian province of Quebec is spending C$65mn ($51mn) on a two-year campaign to recruit and train foreign nurses, with Algeria, Cameroon, Mauritius, Morocco and Tunisia among the francophone countries targeted.
Authorities in Western Australia launched an overseas recruitment drive last year that offered free flights, relocation allowances and free mandatory hotel quarantine to attract foreign nurses.
In times of need, recruiting from overseas is often seen as a “quick fix,” says Catton, but such hiring is often made from countries with the lowest ratio of nurses to population, which “can least afford to lose” them, he adds. “The impact of that can really be dramatic.”
The complete picture of the pandemic’s impact on the nursing workforce is yet to be properly understood due to inadequate data collection. But surveys and some national statistics highlight the challenges health employers are facing to hold on to their staff.
Last month, the UK’s Nursing and Midwifery Council disclosed that just over 27,000 nurses and midwives left the official register in the year leading up the end of March 2022 — a rise of 13 per cent from the year before.
One-third of respondents to its survey said the pandemic influenced their decision to leave, as did pressure and a poor workplace culture.
In the US, about 15 per cent of nurses quit their jobs during the first year of the pandemic, according to a survey by McKinsey & Co published last August, up from about 11 per cent the previous year.
One in five nurses reported they might leave their roles in providing direct patient care in the next year, the survey found.
Dissatisfaction among nurses is widely spread across countries, according to a follow-up report by McKinsey.
It found that in five of the six nations surveyed (the US, UK, Singapore, Japan and France) around one-third of nurses said they were likely to quit within the next year.
The reasons cited by prospective leavers were strikingly consistent, says Gretchen Berlin, who led the research and is herself a former registered nurse. Pay came relatively low on the list. Instead, concerns revolved around a lack of recognition and appreciation, workload and the need for “a sense of belonging”. The “good news”, says Berlin, “is that we have solutions to those challenges”.
In Arkansas, Henderson set up a cookie design business when she quit her job. She says the physical and mental demands of nursing had become too great.
“You have so much on your plate: basic hospitality, cleaning, a lot of physical lifting and then nursing people where you have to be compassionate. I don’t think nurses are compensated for that.”

An international crisis
As Henderson can attest, burnout and mental health problems were an issue even before the pandemic.
A 2021 study by Jama, a US research network, found female nurses were twice as likely as women in the general population to commit suicide.
A 2021 study by Jama, a US research network, found female nurses were twice as likely as women in the general population to commit suicide.
And since Covid hit the US in March 2020, a survey by the American Nursing Association found that one-third of nurses were not “emotionally healthy”. Matthew Crecelius, who recently finished a short-term nursing contract in Missouri, is one of those considering quitting the profession.
“My mental health hasn’t been great working night shift and extended hours. It’s a really tough job,” says the 31-year-old, who is interviewing for a job training people to use medical equipment. Crecelius says the stress of working during the pandemic in New York, where bodies piled up in refrigerated trucks, had taken its toll on him. He was also worried by a recent high-profile case involving a nurse who faced criminal charges after making a medical error. “I did reach out to mental health professionals, you know, to get a little counselling, which is new for me,” he says.
In September the association called on the US government to declare a “national crisis” due to the nursing shortage, which it estimated could be as high as 1mn.
It also recommended a list of structural improvements that could be made for the workforce and ways to improve the mental wellbeing of nurses.
Yet experts say the US is in a much better position than many other high-income nations, with 16 nurses per 1,000 population — one of the highest ratios in the developed world.
The World Bank estimates the equivalent figure in the UK is 10, while the global average is just four.
“The US doesn’t have a nursing shortage. We’ve been increasing the supply for two decades, introducing policies that make nursing more attractive, and 185,000 nurses are graduating every year,” says Linda Aitken, a professor at University of Pennsylvania School of Nursing.
“Our problem is that healthcare organisations are not hiring enough of them.”
“The US doesn’t have a nursing shortage… “Our problem is that healthcare organisations are not hiring enough of them.”
Private employers, she says, are not investing enough in hiring available graduates, causing a shortage of nursing staff in hospitals and nursing homes.
One of the glaring problems in the US system, she adds, is that typically there are no minimum safe staffing requirements to ensure high standards of care.
One of the glaring problems in the US system, she adds, is that typically there are no minimum safe staffing requirements to ensure high standards of care.
The UK has a different predicament, Aitken says. Its shortage is the result of a longstanding reliance on foreign nurses, which has filled the gaps in domestic recruitment and training.
In the year to the end of March, the UK’s nursing and midwives register rose to its highest ever level of almost 760,000, but almost half of the new additions had trained overseas.
The UK has a different predicament, Aitken says. Its shortage is the result of a longstanding reliance on foreign nurses, which has filled the gaps in domestic recruitment and training.
Andrea Sutcliffe, who heads the UK Nursing and Midwifery Council, says two-thirds of the foreign recruits came from India and the Philippines.
Relying to this extent on international recruits carries significant risks, she adds. “In the first three months of the pandemic our international registration dropped to nearly zero because people obviously weren’t coming into the country. Our reliance upon overseas nurses means that we are vulnerable to changing circumstances elsewhere in the world.”
A mixture of increased recruitment from within the UK and better retention is needed, Sutcliffe adds. She also raises questions over the ethical nature of some of the overseas recruitment. “Are we making sure that we’re not denuding other countries of [a] valuable precious resource?” she says.
The UK department for health and social care has “an ethical code of practice” which means recruitment should not be conducted in countries that have their own shortages, but Sutcliffe says “we can see that . . . nurses are joining from some of those countries that were red listed by the WHO”.
It is not the NMC’s job to police compliance with that code but she warns that, along with the health department, it is relying upon employers to “be mindful of where it is that they’re doing their proactive recruitment”.

Shopping for nurses
Nigeria and Ghana are both on that WHO red list. Yet almost 4,000 nurses from the two countries joined the UK register in the year to the end of March this year.
There are also 3,655 nurses on the register from Zimbabwe, which has significant gaps in its own nursing care.
In a report to the World Health Assembly, which concluded last weekend, Tedros Adhanom Ghebreyesus, the WHO’s director-general, warned that many countries “are once again turning to international recruitment to rapidly increase domestic capacity”, a development that was “likely to accelerate global migration and mobility of health personnel”.
Yet not all international recruitment is a bad thing, say health experts. Some countries, such as the Philippines, India and Jamaica, have established themselves as training grounds for nurses and their economies have benefited from the remittances they generate overseas.
Yet not all international recruitment is a bad thing, say health experts. Some countries, such as the Philippines, India and Jamaica, have established themselves as training grounds for nurses and their economies have benefited from the remittances they generate overseas.
In Africa, where the ratio of nurses to population can fall as low as 0.1 to 1,000 people, the ethics are more complex. Kenya offers an example of the complicated dynamics involved in transferring nursing labour and expertise from a developing country to a richer one.
The UK government has signed an agreement with Kenya to accept nurses who were unemployed in their own country. Bernard Mwega, an official with the National Nurses Association of Kenya, says the deal does not in itself risk denuding the country’s health system since many more were graduating from nursing schools than could be found employment.
Yet the reason many trained nurses in Kenya cannot find work at home is because of funding shortfalls in the public health system. Mwega says there have been unconfirmed reports that the government is considering putting restrictions on the number of nurses who are allowed to go overseas.
Jim Campbell, the WHO’s director for health workforce, says the most common destinations are the UK, Canada, New Zealand, Australia, the US, the Gulf countries and France.
When the UK left the EU, Campbell adds, it switched off a principal source of nurses and is now coping with “a huge number of vacancies” while attempting to fulfil a political commitment by Boris Johnson’s government to deliver 50,000 additional nurses by 2024.
“So where do you turn?” Campbell says. “You turn to the historic Commonwealth linkages that the NHS has always had.”
The pandemic and its aftermath may have made working in the UK more attractive as a proposition, he adds. “If you’re working in sub-Saharan Africa and with inflation, your salary is suddenly worth 20 per cent less [and] medical supplies and Covid tools are not available . . . you suddenly look at your work circumstances [and think you could go to] a beautiful hospital in London or a care facility in Scotland and get 10 times your current wages and access to education so you can put your children through school”.
In a sign of tensions between low and middle-income countries and their rich neighbours, Campbell says that the vice-president of Zimbabwe, Constantino Chiwenga, who is also the country’s health minister, was asking the UN to assist in the recovery of compensation for the health workers that had left his country to go to the UK.
Official figures showed that, last year alone, Zimbabwe lost nearly 1,800 nurses, or more than 10 per cent of all the nurses working in public hospitals, mainly to the UK.
“If you apply the vice-president’s logic and numbers, the estimated investment in human capital . . . rapidly surpasses $100mn that is now a resource within the NHS,” Campbell adds.

‘Unprecedented damage’
Covid has already caused “unprecedented damage” to the global nursing workforce, concluded the International Centre on Nurse Migration in a report published in January.
The NGO urged national and global health authorities to implement an urgent action plan.
It recommended independent monitoring of the international flows of foreign nurses, the recruitment agencies that act as middle men, and country to country agreements between rich nations and the developing world.
James Buchan, senior fellow at the UK charity the Health Foundation, and a co-author of the report, says it remains a “blurry” issue as to whether some rich countries are violating the WHO code of conduct because it is hard to ascertain how foreign nurses enter national systems. Stricter monitoring would help.
What we need, he says, is co-ordinated national and international action. National authorities should address the dangerously low staffing levels that lead to burnout and leaving the profession. They should look at how to increase domestic training opportunities and provide fair pay and conditions.
In a November referendum, the Swiss voted to improve working conditions for nurses — a move spurred by staff shortages during the pandemic. “We have too many nurses leaving the profession, a third of leavers are below the age of 35,” says Yvonne Ribi, managing director of the Swiss Professional Association of Nursing Women and Nursing Specialists. “Pay is not the main problem, but bad working conditions.”
The referendum committed the government to work on reforms. Ribi says other countries should take inspiration from its message. “People need nurses, everywhere in the world. Otherwise there will be suffering, death and higher costs for healthcare,” she says.
That sentiment is echoed by Buchan: “Authorities need to recognise that nursing is going to be front and centre of economic recovery,” he says.
“One of the critical messages here is that we’re not looking at nursing as a cost to the country but as an investment.”
Originally published at https://www.ft.com on June 2, 2022.
NAMES MENTIONED
Howard Catton, chief executive of the International Council of Nurses
Gretchen Berlin
Linda Aitken, a professor at University of Pennsylvania School of Nursing.
Andrea Sutcliffe, who heads the UK Nursing and Midwifery Council,
Tedros Adhanom Ghebreyesus, the WHO’s director-general,
Bernard Mwega, an official with the National Nurses Association of Kenya
Jim Campbell, the WHO’s director for health workforce
James Buchan, senior fellow at the UK charity the Health Foundation
Yvonne Ribi, managing director of the Swiss Professional Association of Nursing Women and Nursing Specialists.












