Health, Care and Tech — transformation institute
Joaquim Cardoso
Chief Researcher, Editor and Advisor
December 11, 2022
Executive Summary
What is the situation?
- Americans may be returning to their pre-pandemic habits, but most have not returned to their primary care doctors. Primary care visits are down 10.3% on average across U.S. cities relative to pre-pandemic levels.
- That, combined with more people with chronic diseases like diabetes, obesity, and cancer, and accelerating health care costs as inflation soars, signal a troubled future for the health of Americans and the U.S.’s $4.1 trillion health economy.
What is the issue?
- The author, as a health economist and health services researcher, is concerned to see such little attention paid to how the pandemic has changed consumer health care behaviors, like delaying or forgoing primary care and other necessary health care services.
- The author worries that providers, payers, policymakers, public health institutions, and others in the health economy aren’t talking about the impact of these delays and the public health crisis that will emerge from it.
- And, make no mistake, a crisis is coming, and every health care stakeholder must be prepared.
Table of Contents (TOC)
- Introduction
- Patients aren’t returning to primary care
- Red flags: shifts in cardiovascular disease, and mergers and acquisitions
- From red flags to action
Conclusion & recommendations:
- The negative ripple effects of patients not engaging in routine primary care are evident.
- Health care providers need to act now to get people back on track and engaged with their care, which starts by better understanding and meeting the needs of the various patient populations and markets they serve.
Infographic
The author, as a health economist and health services researcher, is concerned to see such little attention paid to how the pandemic has changed consumer health care behaviors, like delaying or forgoing primary care and other necessary health care services.
And, make no mistake, a crisis is coming, and every health care stakeholder must be prepared.
ORIGINAL PUBLICATION (full version)

Deferral of primary care signals a troubled future for Americans’ health
StatNews
By Sanjula Jain
Dec. 7, 2022
Americans may be returning to their pre-pandemic habits, but most have not returned to their primary care doctors.
Primary care visits are down 10.3% on average across U.S. cities relative to pre-pandemic levels.
That, combined with more people with chronic diseases like diabetes, obesity, and cancer, and accelerating health care costs as inflation soars, signal a troubled future for the health of Americans and the U.S.’s $4.1 trillion health economy.
As a health economist and health services researcher, I’m concerned to see such little attention paid to how the pandemic has changed consumer health care behaviors, like delaying or forgoing primary care and other necessary health care services.
I worry that providers, payers, policymakers, public health institutions, and others in the health economy aren’t talking about the impact of these delays and the public health crisis that will emerge from it.
And, make no mistake, a crisis is coming, and every health care stakeholder must be prepared.

Patients aren’t returning to primary care
Two years after the start of the Covid-19 pandemic, data collected by Trilliant Health, the company I work for, suggest that “delayed” primary care has actually been forgone with much of the use of primary care services attributed to Covid-19-related care as opposed to “routine” primary care services.
Specifically, when excluding care directly related to Covid-19, the volume of primary care visits was down 10.3% in 2021 compared to 2019, suggesting consumers won’t be using primary care more now to make up for the care they missed out on during the pandemic.
Some of this is to be expected: a person who did not see a physician for diagnosis and treatment of the flu does not need to “make up” for not seeking that care.
But delayed or forgone visits for routine screening for heart disease, diabetes, cancer, and other conditions, or for other preventive care, will inevitably result in delays in treating serious diseases that might have been prevented, or at least diagnosed earlier.
But delayed or forgone visits for routine screening for heart disease, diabetes, cancer, and other conditions, or for other preventive care, will inevitably result in delays in treating serious diseases that might have been prevented, or at least diagnosed earlier.
Looking at primary care use across different patient demographics reveals interesting shifts in demand as well:
Commercially insured women between the ages of 20 and 49 are the ones most likely to be resuming visits with their primary care providers.
However, the demand is distributed unequally across various metro areas with demand greater in areas like Dallas and Miami compared to Los Angeles, New York City, Philadelphia, Houston, Seattle, and Washington, D.C.
Commercially insured women between the ages of 20 and 49 are the ones most likely to be resuming visits with their primary care providers.

Red flags: shifts in cardiovascular disease, and mergers and acquisitions
While the magnitude of the pandemic’s impact on downstream health outcomes — like cancers diagnosed at later stages — will not be realized for several years, current indications suggest that near-term interventions are needed.
While the magnitude of the pandemic’s impact on downstream health outcomes — like cancers diagnosed at later stages — will not be realized for several years, current indications suggest that near-term interventions are needed.
Among the emerging signals are
- excess mortality (more people dying than expected) and
- the increased severity of certain diseases, particularly among people aged 25 to 44 years.
Forecasts are already revealing growth in demand for cardiovascular care for people in this age range, which has also seen a disproportionate increase in the number of deaths since the summer of 2021.
Among the emerging signals are: (1) excess mortality (more people dying than expected) and (2) the increased severity of certain diseases, particularly among people aged 25 to 44 years.
Forecasts are already revealing growth in demand for cardiovascular care for people in this age range, which has also seen a disproportionate increase in the number of deaths since the summer of 2021.
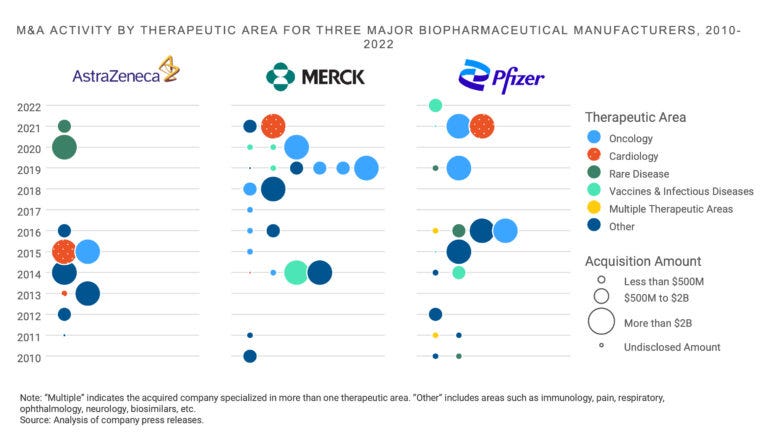
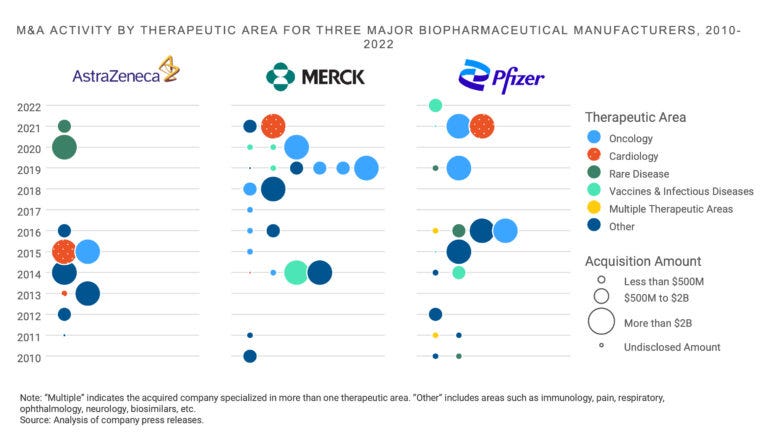
Investment trends among life science companies foreshadow an increasing burden of chronic disease, …
… with two of the four largest merger and acquisition transactions in 2021 focused on cardiovascular disease — a scenario that has not happened in recent years, especially given the recent decline in cardiovascular research and development.
In addition to cardiology, the other two large transactions were generally focused on immuno-oncology and rare disease.
Investment trends among life science companies foreshadow an increasing burden of chronic disease: (1) cardiovascular disease , (2) immuno-oncology and (3) 0rare disease.
Recent investments by life sciences companies also signal a material and enduring change in the clinical burden of disease, with cardiovascular disease and cancer being of particular concern.
Shifts in the need for cardiovascular care, along with the increasing severity and burden of disease overall, will define the post-pandemic health economy for decades.
Shifts in the need for cardiovascular care, along with the increasing severity and burden of disease overall, will define the post-pandemic health economy for decades.
Instead of sitting idly by, health care stakeholders need to do something about it.
Instead of sitting idly by, health care stakeholders need to do something about it.
From red flags to action
From a public health perspective, health care delivery organizations and health care stakeholders in both the private and public sectors should be educating Americans about the importance of preventive care.
From mobile health fairs and mobile screenings to reach vulnerable populations to nationwide communications campaigns and consistent outreach from providers and health plans, it is up to the health care system to better deliver both the message and the means for people to get care.
From a public health perspective, health care delivery organizations and health care stakeholders in both the private and public sectors should be educating Americans about the importance of preventive care.
Traditional health care providers, like hospitals and health systems, as well as new entrants, like CVS Health and Amazon/One Medical, must also find ways to reach and engage patients …
… who remain reluctant to seek routine care — an increasingly difficult challenge given that patients are also losing trust in providers.
Traditional health care providers, like hospitals and health systems, as well as new entrants, like CVS Health and Amazon/One Medical, must also find ways to reach and engage patients … who remain reluctant to seek routine care
an increasingly difficult challenge given that patients are also losing trust in providers.
One way health systems can more effectively reach patients and coordinate care is by better understanding their needs and preferences …
… (considering factors like a patient’s past use of health care and referral patterns, as well as psychographics,including any differences in habits or motivations across patient segments).
When health systems know why patients are delaying care, they can develop more targeted strategies to ultimately improve care delivery and uptake.
When health systems know why patients are delaying care, they can develop more targeted strategies to ultimately improve care delivery and uptake.
Hospital and health system executives should also be considering ways to partner with emerging primary care entrants.
Because new entrants to primary care generally don’t deliver more complex services, like radiology or surgery, hospitals and health systems that enter into partnerships with emerging primary care providers get an important mechanism for driving these primary care patients to their health systems for higher-acuity and more specialized care services.

The negative ripple effects of patients not engaging in routine primary care are evident.
Health care providers need to act now to get people back on track and engaged with their care, which starts by better understanding and meeting the needs of the various patient populations and markets they serve.
Sanjula Jain is the chief research officer and senior vice president of market strategy at Trilliant Health.
Originally published at https://www.statnews.com on December 7, 2022.












