Payers and providers have the data and tech capabilities to tailor the consumer experience at scale and transform medical outcomes and business performance
APRIL 01, 2022
By Ozgur Adigozel and Kendra Wilson
Personalization has the potential to dramatically improve health care as we know it.
Indeed, thanks to advancements in technology, data, and analytics, truly personalized health care is possible on a scale that could not have been envisioned just a few years ago.
Yet while companies like Netflix, Starbucks, and Amazon are already using personalization to transform their businesses, the health care industry lags far behind.
In our work with clients, we’ve identified three ingredients that are critical for launching and scaling an effective health care personalization program.
Organizations that put these pieces in place can see a meaningful impact across many dimensions.
In just 6 to 12 months, some payers that have implemented personalization have seen customer experience improve by 10%, administrative costs drop by 5% to 10%, and quality standards increase by 20% to 25%.
Similarly, providers have seen significant improvements in consumer satisfaction, the length of hospital stays, and 30-day readmissions.
In just 6 to 12 months, some payers that have implemented personalization have seen customer experience improve by 10%, administrative costs drop by 5% to 10%, and quality standards increase by 20% to 25%.
Similarly, providers have seen significant improvements in consumer satisfaction, the length of hospital stays, and 30-day readmissions.

The Time for Health Care Personalization Is Now
As people increasingly take charge of their own health, they have come to expect an experience that’s suited to their unique history, behaviors, and preferences.
That’s as true for a busy mother of two who wants to know where she can get flu shots for her family as it is for a retired Medicare consumer who wants to be reminded to schedule critical preventive screenings.
In the past, it was difficult to capture information about consumer behavior and the other vital data required to personalize the health care experience.
And whatever data could be acquired resided in disparate legacy systems across the organization, which made it hard to create a comprehensive view of the individual.
Compounding these challenges, analytics tools and technology were not yet developed to the point where they could provide actionable insights.
Today, new mobile and cloud technologies along with advanced analytics allow companies to collect and connect a wide array of data and develop meaningful findings from it.
For the first time, organizations can create a truly holistic view of consumers and tailor solutions to their unique needs and preferences.
Today, new mobile and cloud technologies along with advanced analytics allow companies to collect and connect a wide array of data and develop meaningful findings from it.
For the first time, organizations can create a truly holistic view of consumers and tailor solutions to their unique needs and preferences.
Disruptors are seizing the opportunity.
Consumer-centric leaders such as Amazon and Walmart are quickly becoming major forces in the health care space.
So are disruptors like Teledoc Health, DispatchHealth, and Oak Street Health, whose innovative models could replace today’s familiar health care paradigm.
Disruptors are seizing the opportunity. Some examples are: Consumer-centric leaders such as Amazon and Walmart; and disruptors like Teledoc Health, DispatchHealth, and Oak Street Health
Incumbent payers and providers do not have to stand on the sidelines.
They have the data as well as the technological capabilities to customize the experiences of consumers at scale and create a sustainable strategic advantage.
In short, what was a core source of competitive differentiation for digital natives is now possible for all payers and providers.
In short, what was a core source of competitive differentiation for digital natives is now possible for all payers and providers.

Reshaping the Consumer Journey
Truly personalized health care combines two perspectives: that of the consumer and that of the health care organization.
For the consumer, personalized health care means being recognized as a unique individual with a unique health history and circumstances, receiving relevant content and a hassle-free experience, and achieving better health outcomes.
For the organization, it means getting to know the consumer better; using those insights to tailor the channel, timing, and messaging; and developing curated products and solutions.
If personalization is implemented with these perspectives front and center, it can reshape every step of the journey, from the selection of health providers and insurance all the way to posthospitalization and plan renewal.
If personalization is implemented with these perspectives front and center, it can reshape every step of the journey, from the selection of health providers and insurance all the way to posthospitalization and plan renewal.
Take, for example, a payer that wants to improve the experience of a diabetic mother with a newborn.
The company could use its insights on the individual’s unique history and preferences to make recommendations best suited to where that person is in the patient or member journey.
The woman might get a reminder to schedule her next A1C blood test for the same time as her baby’s next visit.
She might also receive personalized notes about taking extra precautions during cold and flu season. And she would get these messages via text and email rather than phone calls.
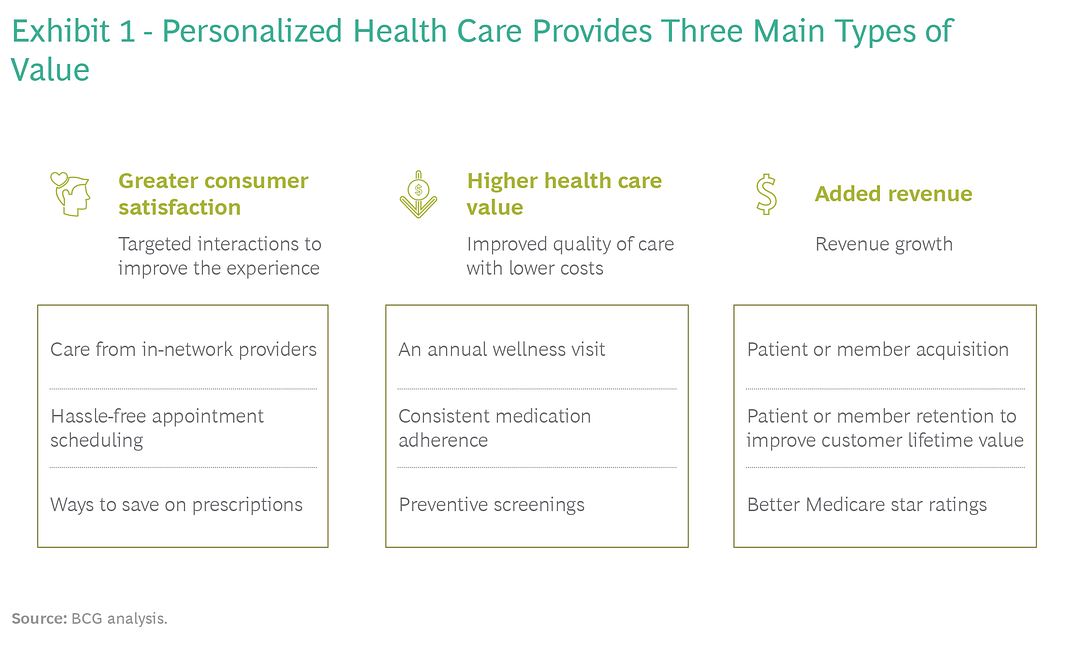
Personalized touch points create greater consumer satisfaction, higher health care value, and added revenue. (See Exhibit 1.)
Developing a Deep Personalization Capability
Any health care organization that seeks to develop this capability needs three basic building blocks: a list of well-defined focus areas that can be delivered on end to end, a personalization engine, and agile ways of working.
A List of Focus Areas
Health care organizations should begin by determining which issues need to be addressed first.
Examples include increasing access to primary care providers, reducing hospital readmission rates, and building awareness of the preventive services that are available.
Prioritization decisions must be based on potential impact and feasibility: organizations should start with the areas that promise the highest value and help build the needed technical and data foundations.
The savings from these cases can then be used to fund the development journey for the rest.
Organizations need to conduct this process regularly to accommodate changes in business priorities, feasibility, and customer needs.
The Personalization Engine
After selecting the most important use cases, organizations need to harness the relevant data, analytics, and clinical expertise to deliver the right interventions to the right members or patients, through the right channel, at the right time.
This requires what we call a “personalization engine,” a technology stack consisting of five elements. (See Exhibit 2.)
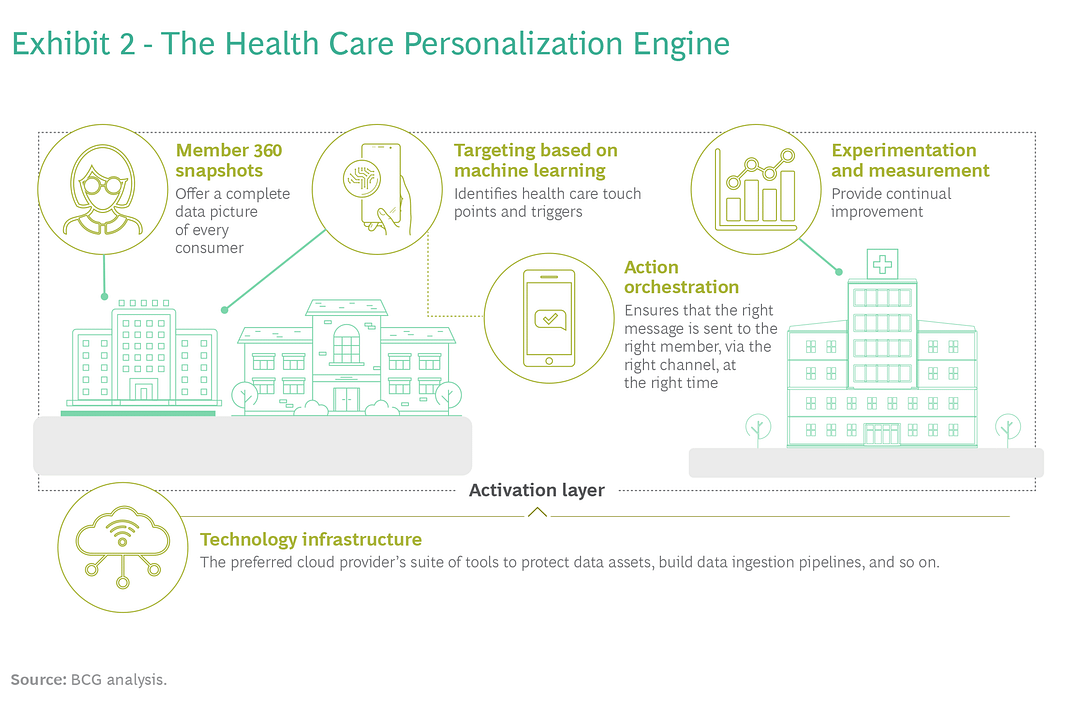
Member 360 Snapshots. A central data repository, Member 360, contains hundreds of attributes for each consumer. With the help of analytics, this information can provide a complete picture of the consumer.
Much of the 360 data comes from legacy systems, including claims, call center logs, labs, appeals and grievances, pharmacy records, and billing. But several newer kinds of data can also provide considerable value. Electronic health records (EHR), which contain a consumer’s clinical data as well as details on things like time preferences and no-shows, enables providers to share information and make better decisions. In addition, consumers’ behavioral data can be collected from wearables that measure physical activity and fitness. And organizations can use publicly available data sources to determine if an individual has limited access to housing, food, or other needs related to social determinants of health (SDoH).
Member 360 provides important value on several fronts. In addition to supporting a wide variety of analytics use cases, it improves organizational data quality and usability. Moreover, because it collects and integrates legacy and new data in one place, Member 360 eliminates the challenges associated with disparate legacy systems and serves as a single source of truth. And since the platform updates automatically as new data are identified, it ensures that the snapshot of each consumer stays current as well.
Targeting Based on Machine Learning. An ML algorithm then combs through the broader Member 360 data to determine the individual consumer’s key care touch points and triggers for those touch points.
Advanced analytics make it possible to identify the optimal care pathway for every consumer. For patients with a history of back problems, for example, ML can help determine for each care touch point which types of interventions have eliminated the need for major surgery and use these interventions for other patients with similar back problems. ML can then help determine, for instance, the best communications to provide following cortisone injections, such as sending reminders to activate gym benefits or providing educational articles on a promising new drug.
All these signals can be codified into a sequencing logic. For example, a consumer’s failure to refill a hypertension medicine prescription would trigger a communication reminding the consumer to go to the pharmacy or call her cardiologist.
Action Orchestration. When ML models and simple decision rules are used in combination, they can ensure that individuals receive the right message, via the right channel, at the right time, thus maximizing the likelihood of response. The personalization engine selects the level of touch for each communication, whether high (outbound calls and secure messaging) or low (emails and text messages). The engine also selects the delivery channel. Since digital and analog channels are integrated, the delivery of communications is completely seamless.
Experimentation and Measurement. Different testing methods are critical for ensuring that interventions are effective and that a personalization program delivers value. Simple A/B testing (using two or more versions) and multivariate testing (determining which combination of variables works best) can measure the impact and maximize the value of the analytics.
Consumer input is provided via a feedback mechanism embedded in channel applications. The advanced analytics models use this input to continually improve the experience and deliver more value over time.
Technology Infrastructure. At the core of the personalization engine lies the technology: a data infrastructure and a production framework. Together, they enable messages to be developed and deployed throughout the organization.
The data infrastructure consists of the preferred cloud provider’s suite of tools for protecting data assets, developing data ingestion pipelines, and building development, testing, and production environments as well as docker-based deployments.
A cloud-based infrastructure offers some important advantages. Setup is simple. Only a few clicks are needed to add a new service, which makes it convenient to adapt to state-of-the-art technologies. It’s also easy to rapidly build and release more personalization use cases. The infrastructure is based on HIPAA-compliant architecture, which ensures that security standards are met. And monitoring is straightforward because cloud services provide detailed metrics.
The production framework is a cloud-agnostic, scalable solution that enables the design and deployment of production systems.
It automates versioning, path and configuration management, as well as cluster termination, and uses Apache Airflow automation.
With scalable infrastructure and automation handling the day-to-day requirements of artificial intelligence projects, the technology infrastructure allows the team to focus on the data science regardless of the choice of cloud provider.
Ways of Working
The development of use cases requires an agile approach in which a small working team with expertise from across the organization iteratively designs and tests different personalized communications to see if they resonate with individual patients or members.
A continual feedback loop enables the team to use the learning from each outreach to refine the design. This ongoing cycle of testing and learning allows the team to create value while building capabilities.

Accelerating the Path to Value
It could take two to three years to achieve mastery in personalization. Yet with the right preparation, organizations can see significant value in as little as six months.
It could take two to three years to achieve mastery in personalization. Yet with the right preparation, organizations can see significant value in as little as six months.
To start generating value quickly, organizations need to evaluate their maturity in the five components of the personalization engine, from cataloging their data assets to evaluating their channels and technology infrastructure.
On the basis of this assessment, organizations can start developing a roadmap for the personalization journey.
he roadmap should detail how to leverage and build out the data repository.
The plan should also discuss which uses cases to start with, how to set up the teams that will build the first personalized interventions and applications, and how to integrate the various channels that will be used.
Once the assessment and roadmap have been completed, organizations can start their personalization journey.
There has never been a better time for health care organizations to develop a sophisticated personalization capability. Those that start now will create a source of advantage for many years to come.
Originally published at https://www.bcg.com on March 28, 2022.

There has never been a better time for health care organizations to develop a sophisticated personalization capability. Those that start now will create a source of advantage for many years to come.












