the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
10 de outubro de 2023
Sumário executivo
Qual é a mensagem?
A radiologia está em uma encruzilhada à medida que enfrenta a integração da inteligência artificial (IA) em sua prática.
Embora a IA tenha um imenso potencial para aprimorar os processos de diagnóstico e melhorar o atendimento ao paciente, sua adoção enfrenta desafios devido a perspectivas distintas sobre seu valor e impacto no campo da radiologia.

Pontos-Chave
Visões Divergentes sobre o Valor da IA:
A IA é percebida de forma diferente por várias partes interessadas no campo médico. Para executivos hospitalares e fornecedores de IA, a IA representa um promissor retorno sobre o investimento e geração de receita. No entanto, os radiologistas, os usuários finais da IA, veem-na como uma potencial ferramenta para aumentar a produtividade, o que gera preocupações, uma vez que já enfrentam altos volumes de imagens.
Dilema da Produtividade:
Os radiologistas estão presos em um dilema de produtividade, onde seu desempenho é avaliado com base na quantidade de estudos que leem. A promessa de maior produtividade da IA pode agravar sua carga de trabalho, potencialmente levando ao esgotamento e ao aumento do estresse.
IA como Auxílio no Diagnóstico:
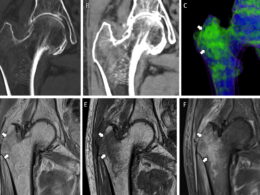
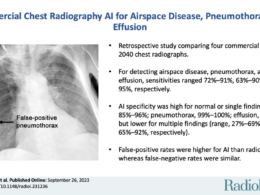
A IA tem o potencial de auxiliar os radiologistas na detecção de achados sutis e na redução de erros diagnósticos. No entanto, os radiologistas podem ser cautelosos em relação à capacidade da IA de equilibrar sensibilidade e especificidade, o que é crucial para a precisão diagnóstica.
A Armadilha dos Falsos Positivos:
A sensibilidade da IA pode levar a um aumento no número de resultados falso-positivos, potencialmente distraindo os radiologistas de resultados verdadeiramente positivos e submetendo os pacientes a intervenções desnecessárias. Isso pode afetar a precisão diagnóstica da radiologia.
Substituição de Radiologistas pela IA em Tarefas Selecionadas:
A IA pode ser usada para identificar resultados de estudos normais, permitindo que os radiologistas se concentrem em casos anormais. No entanto, contextualizar resultados “normais” com os sintomas do paciente e entender a ampla gama de normalidade em imagens médicas é uma tarefa complexa.
Mudança no Papel dos Radiologistas:
Os radiologistas podem precisar evoluir de meros geradores de relatórios para gerentes ativos de caminhos diagnósticos e cuidados com o paciente. A IA pode ajudar a automatizar certos aspectos do trabalho do radiologista, permitindo que se concentrem na gestão de informações e na coordenação de sistemas.
Desafios da Adoção da IA:
Em países de alta renda, como os Estados Unidos, os incentivos para que os radiologistas adotem a IA podem não ser tão convincentes devido à cultura estabelecida de produtividade. Modelos de pagamento baseados em valor e mudanças nos paradigmas de assistência médica devem incentivar uma maior adoção da IA na radiologia.
Integração Contínua da IA:
A IA já está avançando na radiologia, desde a reconstrução de imagens até a geração de relatórios. À medida que a IA amadurece, ela capacitará os radiologistas a atuarem no auge de suas capacidades, enfatizando a colaboração entre a expertise humana e a tecnologia de IA.
Em conclusão
A integração da IA na radiologia apresenta desafios e oportunidades. Os radiologistas devem navegar pelo cenário em constante evolução, reconhecendo o potencial da IA para aprimorar seu trabalho e abraçando a necessidade de adaptação e colaboração neste campo dinâmico.
IMERSÃO

Algorithms at the Gate—Radiology’s AI Adoption Dilemma
JAMA Network
Saurabh Jha, MBBS, MS
October 6, 2023
ChatGPT, an artificial intelligence (AI) chatbot trained on large language models, whose feats include generating radiology reports in the literary style of Emily Brontë, has revived dystopias of AI. Radiologists are accustomed to AI-mediated extinction prophesies. The father of deep learning, Geoffrey Hinton, once advised against training radiologists because he believed that AI would soon replace them.1 Seven years after Hinton’s prophesy, far from extinction, a radiologist shortage exists.2 To understand the adoption trajectory of AI-enabled diagnosis from medical images, it is important to understand the structure of radiology and the incentives radiologists face.
AI and Productivity in Radiology
The value of AI is viewed differently by different stakeholders. Artificial intelligence vendors appealing to hospital executives make the business case for AI: a return on investment, which is invariably revenue generation. Industry sells AI as a productivity-enhancing tool, which is singularly unappealing to radiologists, AI’s end users, who already are at their wits’ end with imaging volumes. However, because of the reimbursement structure, productivity is the lifeblood of radiology. Radiologists are judged and rewarded for how many studies they read. They are in a productivity quagmire: productivity sustains them and productivity ails them.
Three trends have coalesced to shape radiology. Radiologists have become more efficient because of faster integrated reading systems. They view more images, largely from thin-section computed tomography. And the reimbursement per study has declined. The promise of AI’s increasing productivity could sink radiologists deeper into the productivity quagmire.
With efficiency gains from AI, radiologists can read either more studies in the same time or the same number of studies in less time. With the latter, AI could theoretically enable a more pleasant work experience. In practice this is unlikely. Although the link between productivity pressure and burnout seems clear,3 it is far from certain that marginal gains, such as finishing work an hour earlier, will spiritually rejuvenate radiologists. Instead, efficiency gains might extend the dominance of a smaller labor force: fewer radiologists working more efficiently but just as intensely, and similarly predisposed to burnout.
AI as a Diagnostic Aide
Artificial intelligence could be radiologists’ aide, pointing out subtle findings they might miss, such as small pulmonary emboli. Reducing errors is a compelling case for AI use. However, radiologists may be skeptical, aware of the stubbornness of the receiver operating characteristic (ROC) curve where gains in sensitivity often penalize specificity. There is no free ROC lunch. False-positive results overwhelm both radiologists by distracting them from true-positive results and patients by subjecting them to unnecessary interventions. Furthermore, sensitive technologies may overdiagnose pathology (ie, find clinically irrelevant diseases).4
Computer-aided detection for reading mammograms is instructive.5 In an attempt to be more sensitive and “never miss cancer,” it lost specificity and became the proverbial boy who cried wolf. Widespread adoption of AI may change how radiologists interpret images. Inexperienced radiologists in particular may be unable to ignore AI, succumbing to an avalanche of false-positive results.6
Whether AI augments radiologists’ performance or radiologists regress to AI’s level remains speculative. What is not speculative is that an extra pair of eyes, with both AI and radiologists checking each other’s work, may not reduce the net labor conscripted to extract meaningful clinical information from images. Over time, radiologists may reflexively note the possibility that AI will detect something that they will not and may make radiologists, who infamously hedge, hedge even more. Known as the Solow paradox, development in information technology has historically often slowed productivity.
AI Replacing Radiologists in Selected Tasks?
Another use for AI is reading normal study results, decanting the abnormal ones for radiologists. Because many study results are normal, AI could reduce radiologists’ workload. This sounds appealing but only superficially. For one, “normal” must be contextualized with symptoms because a normal study result does not mean the patient does not have an illness. To detect “abnormal,” radiologists must know normal. In fact, “normal” is arguably the most difficult diagnosis to make. On imaging, “normal” has a broad and variegated coastline. The heaviest radiology book I own is Atlas of Normal Roentgen Variants Which May Simulate Disease, which I still have not finished reading.
Just because radiologists may be reluctant to adopt AI does not mean other clinicians will not find AI useful. For instance, as soon as the result of computed tomography has been acquired, AI alerts neurologists about patients with stroke potentially amenable to thrombolysis, often with the patient still on the scanner and sometimes before the radiologist has viewed the images. Promptly informed, neurologists can commence therapy sooner, and because “time is brain,” patients may have better outcomes.7 Removed from the loop, radiologists are left cleaning up the false-positive results and incidental findings.
Radiologists have focused excessively on radiology reports, considering them the sole distillates of their expertise. Nothing is more sacrosanct for the profession than the turnaround time of reports. The report is only 1 part of imaging’s role in care systems. For example, positive imaging findings, such as coronary atherosclerosis, should induce other steps, such as ensuring the patient is taking an optimal dose of statins and directing the patient to the appropriate physician. By interrogating the electronic health record, AI can theoretically do this seamlessly. If the profession changes from being charged with just report generation to system management as well, in which the radiologist’s job is as much activating the next step in the diagnostic pathways as it is deciding whether a study finding is positive or negative, radiologists may find AI more useful.

AI Enabling an Expanded Scope for Radiology
Artificial intelligence enables automation; that is, it reduces the labor required to achieve tasks. Since the industrial revolution, labor and automation have coexisted, and it is labor that has adapted to technology. Automation has encouraged labor to imagine new roles, and labor has often benefitted from the automation. For example, automated teller machines, far from eliminating bank tellers, increased their numbers by growing the demand for banks.8
Radiologists are familiar with automation. Formerly, they were at the scanners guiding image acquisition. As specialized knowledge became more available and technology improved, acquisition was automated, and radiologists became involved less in acquisition and more in imaging interpretation. The automation from AI may displace radiologists once again, this time from imaging interpretation to novel roles such as information management. For instance, AI could scale radiology’s influence in population health, such as lung cancer screening, in which the radiologist’s job will not be reporting as many results of computed tomography as rapidly as possible, but in coordinating screening, leaving AI to seek lung nodules. To harness AI’s full potential, radiologists must relinquish some of their work to algorithms and reimagine the human nonautomatable components of their work.
In low- to middle-income countries, AI detects pathologies such as tuberculosis9 not only because it can but also because radiologists are scarce. The incentives to adopt AI by overoptimized US radiologists are not as compelling but may change with value-based payments, and whatever value will mean, new payment models are certain to extricate radiologists to some degree from the productivity quagmire, changing culture and encouraging adoption.
It took more than a decade for magnetic resonance imaging to travel from research to clinical practice; AI, which is still young, is already being used in the radiology value chain, from image reconstruction to report generation.10 Eventually, AI will allow radiologists to perform at the top of their license.
Originalmente publicado em https://jamanetwork.com/journals/jama