BCG – Boston Consulting Group
Priya Chandran, Vincent Chin, Chan Harjivan, Martin Reeves, Yvonne Zhou
February 2020
The coronavirus outbreak is only the latest in a long series of wakeup calls over the past few decades for the global health community. Once again, a high consequence pathogen, likely incubated in nature, infected humans, and overwhelmed health care systems before the medical community could figure out how to contain it. As of the time of this writing, more than 78,000 COVID-19 confirmed cases and nearly 2,500 deaths have been reported.
The coronavirus outbreak—and other contagions that will inevitably follow—can be controlled. But it will take planning, collaboration, and a comprehensive, systemic approach. A truly effective health-emergency response system will require continuous vigilance and improvement in the capacity to rapidly identify and understand novel pathogens; develop diagnostics, vaccines and other countermeasures; and distribute necessary medicines, medical supplies, health professionals, and timely public information.
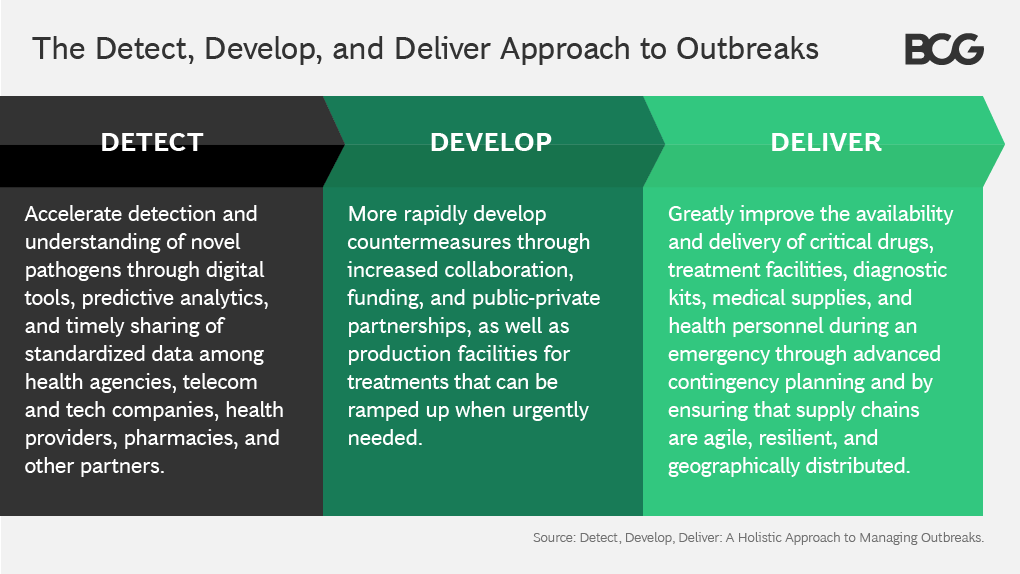
We frame this holistic approach as Detect, Develop, and Deliver.
Though the global readiness for infectious disease events is improving, the COVID-19 outbreak underscores the considerable work that still must be done to more effectively respond to disease outbreaks in today’s increasingly interconnected world. The key opportunities for improvement include:
- Accelerating detection and understanding of novel pathogens through digital tools, predictive analytics, and timely sharing of standardized data among health agencies, telecom and tech companies, health providers, pharmacies, and other partners.
- More rapidly developing countermeasures through increased collaboration, funding, and public-private partnerships, as well as production facilities for treatments that can be ramped up quickly in time of urgent need.
- Greatly improving the availability and delivery of critical drugs, treatment facilities, diagnostic kits, medical supplies, and health personnel during an emergency through advanced contingency planning and by ensuring that supply chains are agile, resilient, and geographically distributed.
Why Sustained Preparedness is Essential
If there is one given in infectious disease, it is that nature will continue to create new pathogens. Indeed, due in part to greater exploitation of the natural environment and higher population density, they are occurring with growing frequency. Just since the late 1970s, we have seen Ebola, HIV, SARS, MERS, “swine flu” (H1N1), “bird flu” (H5N1), West Nile, Zika, and now COVID-19—all thought to be caused by novel pathogens that jumped from animals to humans. Dramatic growth in travel—from 950 million international trips in 2010 to around 1.4 billion in 2018, according to the United Nations World Tourism Organization—makes it increasingly easy for local outbreaks to develop into epidemics, and epidemics into pandemics.
What’s more, it is currently difficult to predict the path a new epidemic will take. The method of transmission, odds of infection, incubation time, and mortality rate of novel pathogens vary dramatically. That makes it hard to contain a new infectious disease by using methods perfected during previous outbreaks.
Another factor contributing to recurring, large-scale contagion is that most health-care systems around the world are unprepared to cope with such crises. There is history of infectious diseases, like Ebola, emerging and persisting in developing nations with poor health systems. But the rapid spread of coronavirus in China illustrates how a major outbreak can quickly overwhelm the health systems even of regions that have made enormous strides in economic development and health preparedness. There is little reason to assume that a similar epidemic would not overwhelm the health systems of most advanced economies as well: consider, for example, the emergency-care crises in New Orleans in the wake of Hurricane Katrina in 2005 and in Puerto Rico after Hurricane Maria in 2017.
Furthermore, the interconnectivity of the global economy and public panics that are amplified by social media are heightening the economic impacts of infectious-disease outbreaks. A 2015 outbreak of Middle East respiratory syndrome (MERS) in South Korea infected just 186 people, and avoidance measures cost that nation’s economy an estimated $8.2 billion, according to the Korea Economic Research Institute. The US National Institute of Health estimates that the total economic impact of the 2003 SARS outbreak in Asia was at least $40 billion; the economic fallout of coronavirus is expected to be far greater, according to an analysis by IHS Markit.
A Multi-Pronged Strategy for Managing Outbreaks
Containing modern contagions, therefore, requires holistic, ongoing, and adaptive emergency preparedness strategies for managing outbreaks along the three dimensions of detection, development, and delivery.
1.Detection
Detection is the process of identifying and characterizing a pathogen causing an outbreak. Scientists are making impressive strides in their ability to identify new pathogens. Chinese scientists were able to genetically sequence the coronavirus in early January, around a month after it was identified, and shared the sequence with the World Health Organization. This gave health authorities around the world a head start in developing vaccines and diagnostic tests that could be used in the field. The disease surveillance network that China developed after SARS allows public health workers to rapidly report unusual illnesses to central health authorities.
Detecting and tracking dangerous new pathogens is not just the job of biomedicine. Because they are created in nature, and their spread is influenced by a wide range of social and economic factors, detection efforts by health organization should marshal the expertise of a far broader ecosystem of experts than they do now, including wildlife biologists, veterinarians, ecologists, and even political scientists and economists.
Outbreak detection can also go from being reactive to predictive. In the US and most other countries, authorities learn of outbreaks only after patients visit physicians or emergency rooms after contracting an illness. To track the outbreak, authorities then attempt to retrace those patients’ footsteps and discover others who may have been exposed.
Improved digital tools can be deployed to detect outbreaks more quickly. Currently, however, these tools primarily are used by individual companies and organizations. They could provide valuable early-warning systems if used in an integrated way. Sudden increases in internet searches for symptoms of fevers or flu, social media posts by people saying they are staying home due to illness, or increased purchases of ibuprofen or antibiotics at local pharmacies, for example, can offer signals that clusters of people are coming down with a certain illness. Unusual changes in the movement patterns of cellphones—such as that large numbers of users in a neighborhood haven’t left their homes for several days—could also be tip-offs of possible outbreaks. Such tools are available in much of the world, including Africa, Southeast Asia, and Latin America.
Although safeguards would be required to assure privacy, agencies such as the World Health Organization or a national agency, such as the Centers for Disease Control in the US, could form partnerships with telecom companies, online media companies, pharmacies, and other sources to aggregate such data and detect emergencies earlier through predictive analytics. Some technology companies have worked on such detection systems; further efforts should be supported and coordinated. Such information could also enable authorities to alert pharmacies, health care providers, and suppliers of essentials such as diagnostic kits to prepare to gear up. This can also facilitate more timely, coordinated, and consistent reporting by health care providers.
Just as important as identifying a new pathogen and an outbreak is understanding how it works. How pathogens spread and their impact can be understood through three broad factors—transmission rate, latency and mortality rate.
The transmission rate is measured by R0, pronounced “R naught,” a mathematical term that expresses how contagious a virus is. Measles has an R0 of around 14, one of the highest. This means that up to 90% of unvaccinated individuals who are close to someone with measles will also become infected. By contrast, Hepatitis C, which requires close contact with the blood of an infected person, has a very low R0. Latency is the time it takes for an infected person to exhibit symptoms. For HIV/AIDs, this can take years, while for the main strains of flu it can be a few days. The mortality rate also varies widely by disease. The mortality rate for SARS was around 10%, according to World Health Organization data, and has averaged 50% for Ebola outbreaks.
Each of these factors, moreover, are dynamic and affected by many variables, including weather, population movement, and the individuals themselves. Because infectiousness can precede symptoms, there can be a period during which the host is capable of transmission— but unaware that he or she has been exposed to the infection. The spread of a pathogen, therefore, is also driven by the patients’ social behaviour.
Understanding a health outbreak is an iterative process. Every day, experts around the world learn new things about the coronavirus—such as how it spreads, the mortality rate, and which containment measures seem to be working. Health professionals are constantly validating and revalidating hypotheses and adjusting their responses accordingly. Governments must take an Agile approach as more information is gleaned and more is learned about the pathogen.
Transparency and wide sharing of data—not just within countries but globally—is therefore critical to understanding the pathogen. Current systems for sharing data must be strengthened, ramped up, and include a broader network of partners. What’s more, much of the data that is currently exchanged is inconsistent and in formats that are not usable to all. One hospital may report how many patients are infected, for example, while another may only report how many patients were treated or how many diagnostic tests were conducted. Governments need to create and foster data sharing strategies. Coordination across health systems can assure that data is interoperable.
Faster detection of pathogens and understanding of how they work might also mitigate the adverse economic impact of contagions. Panic buying, workplace closures, and event cancellations based on rumors or faulty information may be avoided if authorities can more quickly inform the public of the nature of the threat and evidence-based actions for avoiding infection.
2.Development
Improvements in detection will in turn improve the next stage—Develop. The more scientists learn about a pathogen, the faster they will be able to develop vaccines or other effective treatments. A free exchange of information among health authorities on their experiences with countermeasures will help answer key questions—such as whether or not quarantines really work.
Early detection and better information also enable authorities to develop countermeasures more quickly. They can prepare public communication strategies that can help containment once the pathogen arrives in their population, such as campaigns to remind citizens to wash their hands and to avoid public places. They can also be better informed regarding which advice to communicate, such as whether or not face masks actually offer protection.
In terms of treatments, the recent outbreaks have exposed continued shortcomings in development of new countermeasures in the global health community. Novel pathogens often fail to respond to treatments currently on the market. Because development of new antimicrobials has been declining, there are fewer other weapons readily available in the fight.
Given the anticipation of emerging pathogens, new antimicrobials should always be under development. Governments and international health organizations should fund ongoing R&D programs and offer financial support that can sustain manufacturers, such as more robust reimbursement strategies. Antimicrobials that proved ineffective against previous pathogens should be vigilantly maintained, for they may be effective against new ones. By maintaining a broad armamentarium of antimicrobials, researchers can test novel pathogens against a wider range of potential treatments. Health organizations should also further bolster strategies in place with drug developers so that R&D, clinical trial networks, and manufacturing capacity can be more quickly mobilized and scaled up to test new treatments during an outbreak.
Science has gotten much better in recent years at rapidly developing new vaccines. New technologies and approaches aim to reduce the time from initial research to human testing down to a couple months from the identification of a new pathogen. Even greater funding and coordination is needed to expand drug and vaccine research programs and to accelerate the entire drug-development process, including testing, pilot production, and large-scale manufacturing.
This will require strong public-private partnerships and even greater incentives for pharmaceutical companies to invest in research in areas where the economics may be less attractive than other areas, such as oncology and chronic disease. While there are ample supplies of treatments for known diseases, private pharmaceutical companies have little financial incentive to develop potential drugs that may have no market, and they cannot develop vaccines for a disease that is unknown and cannot be tested on patients.
Governments and health authorities should also develop in advance strategies for quickly addressing the social and economic implications of a major infectious disease outbreak— which are often overlooked until substantial damage has been done. They should develop contingency plans for shutdowns of schools and extended closures of factories and other workplaces, for example. Governments should also anticipate the potential economic hardships on workers and families. They can ask how children will continue to learn while they are not in school. How will companies manage during extensive shutdowns, and will they compensate employees? What about self-employed workers with no other sources of income? If transportation is restricted, how will stores and households get needed supplies? Such an assessment may also offer an opportunity to look at industries holistically and review investment in new technologies, regulatory processes, or infrastructure.
Singapore is using a number of innovative approaches to mitigate some of these problems during the current coronavirus outbreak. The government has launched a $55 million relief fund for 40,000 taxi and ride-hailing service drivers who are coping with falling ridership, for example, and is preparing a strong government budget to offset a broader economic impact.
School districts and workplaces can also leverage digital tools during long closures. All schools in China, for example, are using online channels for remote classes, while many companies are leveraging video conferences and collaboration tools for remote work. Downloads of DingTalk, a mobile collaboration platform of Alibaba, have reached 1.1 billion. Local authorities should also develop plans to ensure that households will be able to get food and other necessities if stores are closed or transportation is curtailed. In addition to helping mitigate social and economic hardships, such contingencies could secure greater cooperation from employers, parents, and workers when they are asked to stay indoors.
3.Delivery
As the health community develops new treatments and countermeasures, work on Delivery must also gain greater urgency. Considerable improvement is needed in global health infrastructure. Authorities should systematically ensure the resiliency and redundancy of global supply chains on which patients depend for critical drugs. While this is an issue even for treatments of common chronic diseases such as diabetes and hypertension, it is particularly challenging in times of crisis, such as natural disasters and disease outbreaks. Hurricane Maria, for example, contributed to critical shortages of medical saline manufactured in Puerto Rico.
When effective treatments are found, there needs to be ability to rapidly scale in time of need, and ensure that the infrastructure is in place to deliver supplies to populations—including people living in remote villages or highly impacted neighborhoods. It is virtually impossible to plan for the scale of crisis that has occurred in Wuhan during the coronavirus outbreak. But authorities around the world should explore every tool available to improve the capacity of supply chains for everything from diagnostic kits and protective clothing to hospital beds . Health systems need a plan to quickly ramp up health care workers to meet the crushing demands of a modern epidemic.
One key lesson that has emerged from recent infectious-disease crises is that the supply network must be geographically distributed. If mass quantities of medicines or certain equipment is urgently needed in South Africa and Brazil, for example, supplies may need to be shipped from long distances. Another risk of concentrating too much production or storage of critical drugs or medical supplies in one area is that transportation or manufacturing facilities could be locked down if that location itself is struck by a disease outbreak. Manufacturing footprints and stockpiles of treatments, testing kits, and other medical supplies should therefore be distributed across a number of regions, and redundancy should be built into the system.
The ability of a given company to rapidly scale production of potentially useful drugs and diagnostic kits is often constrained. Governments could secure agreements with pharmaceutical companies to share licenses and production techniques with other manufacturers if they are unable to scale up rapidly to produce sufficient quantities of vaccines or new treatments. They could also proactively define approaches that protect intellectual property and sustain incentives for innovation.
The enormous stresses on the health care system of Wuhan during the coronavirus outbreak also illustrated the urgency of assuring that medical care can be delivered to large numbers of patients on short notice. In Wuhan, 27 hospitals designated for treating coronavirus patients were quickly filled to overflowing. One of the most impressive achievements in China’s response was its ability to mobilize 2,000 workers to build two new modular hospitals in just ten days, adding 2,600 beds. In most nations, even getting the land in a major city to build a new hospital in months would be impossible.
But with advance planning, there are a number of actions communities can take to assure there will be enough diagnostic facilities—probably the most critical need—and quarantine space during a major outbreak. For example, as new hospitals are constructed, they can be built with areas that can be rapidly converted into infectious-disease isolation wards.
Government agencies should design logistical resilience for delivery of essential supplies into their emergency preparedness plans. Supply chains have numerous private and public actors: delivery providers such as UPS and postal services, drug store chains, grocery stores, wholesalers, and even e-commerce platforms such as Amazon and Alibaba. Authorities should co-develop and coordinate emergency preparedness plans, including commercial partnerships, to guarantee that there are not shortages of drugs, food, medical supplies, water, and other basic needs—and that people quarantined in their homes will be able to obtain them. In Hong Kong, rumors that there were shortages even of such common essentials as toilet paper triggered panic buying.
Once the coronavirus outbreak subsides, there should be a period of reflection on the lessons learned—and how those lessons can be incorporated into future preparedness plans.
Responding quickly to a fast-moving outbreak would be hard for any country, especially in a highly connected world. Identifying and containing an outbreak is more difficult. Through integrated strategies, agile approaches, use of digital tools and improved planning and collaboration, outbreaks can be managed more effectively. In fact, the Detect, Develop, and Deliver model can apply to all high-consequence health and humanitarian threats, including genetically engineered biological weapons, chemical and nuclear threats, malaria outbreaks, earthquakes, and tsunamis.
About the Authors
Priya Chandran is a managing director and senior partner in the New Jersey office of Boston Consulting Group and leader of the Health Care Systems sector.
Vincent Chin is a managing director and senior partner in the Singapore office of Boston Consulting Group and global leader of the Public Sector practice.
Dr Chan Harjivan is a managing director and partner in the firm’s Washington DC office with a focus on health security.
Martin Reeves is a managing director and senior partner in the firm’s San Francisco office and chairman of the BCG Henderson Institute, BCG’s think tank on new approaches to strategy and management.
Yvonne Zhou is a managing director and partner in the firm’s Beijing office. She leads the firm’s Public Sector practice in Greater China and is a leader in its real estate and city development sectors.
To download the PDF open the URL below:
https://media-publications.bcg.com/Whitepaper-Detect-Develop-Deliver-A-Holistic-Approach-to-Managing-Outbreaks-feb-2020.pdf