Reference: British Medical Journal paper (21 September), “Margin status and survival outcomes after breast cancer conservation surgery: prospectively registered systematic review and meta-analysis”
Site editor:
Joaquim Cardoso MSc
The Health Strategist — Institute: — for continuous health transformation
September 21, 2022
Executive summary:
Overview:
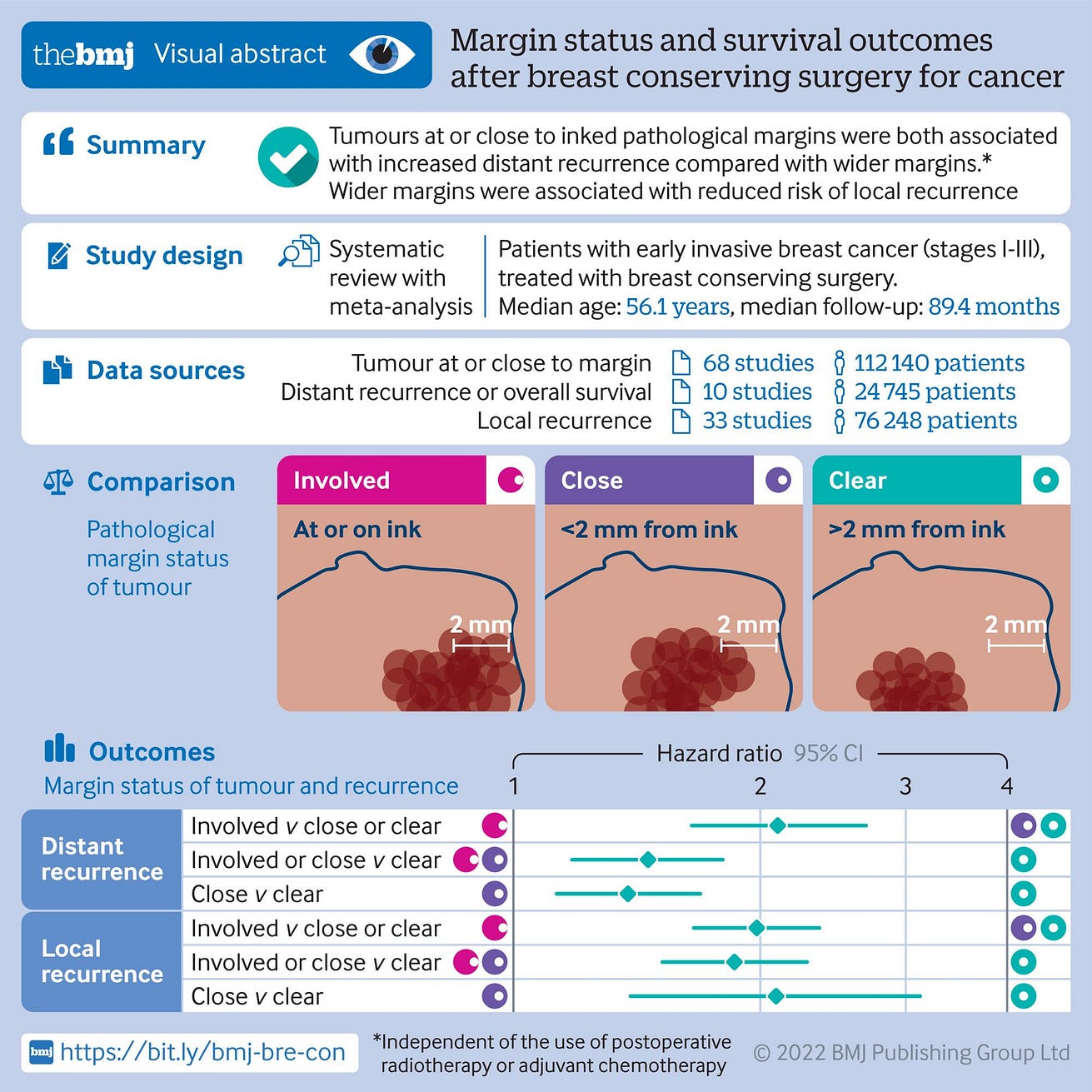
- Leaving a margin of at least one millimetre of healthy tissue when removing a breast tumour reduces the risk that the cancer will recur.
- A review of 68 observational studies that followed up on more than 100,000 people with breast cancer found that increasing the margin from zero to 2 millimetres halves the risk of cancer coming back.
- Researchers are now calling for a review of international guidelines.
Objective
- To determine if margin involvement is associated with distant recurrence and to determine the required margin to minimise both local recurrence and distant recurrence in early stage invasive breast cancer.
Design
- Prospectively registered systematic review and meta-analysis of literature.
Data sources
- Medline (PubMed), Embase, and Proquest online databases. Unpublished data were sought from study authors.
Eligibility criteria
- Eligible studies reported on patients undergoing breast conserving surgery (for stages I-III breast cancer), allowed an estimation of outcomes in relation to margin status, and followed up patients for a minimum of 60 months.
- Patients with ductal carcinoma in situ only or treated with neoadjuvant chemotherapy or by mastectomy were excluded.
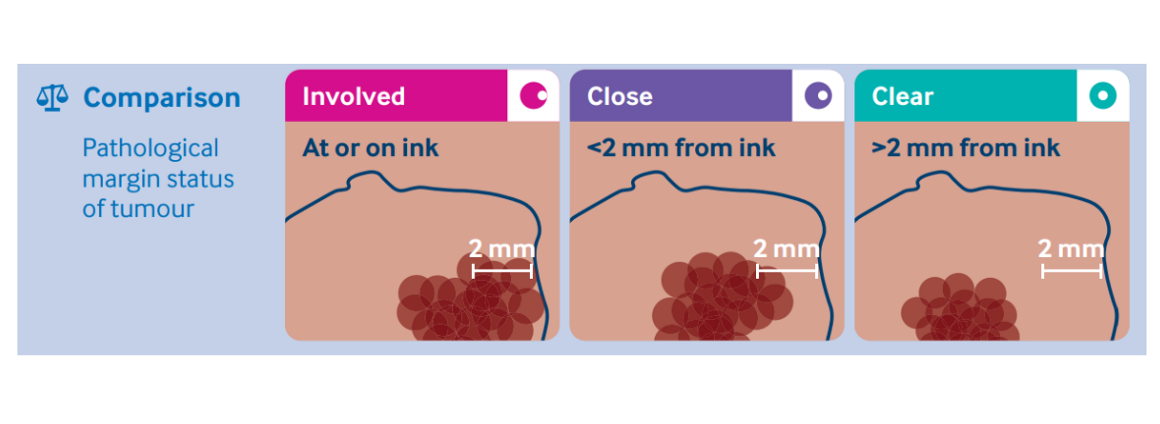
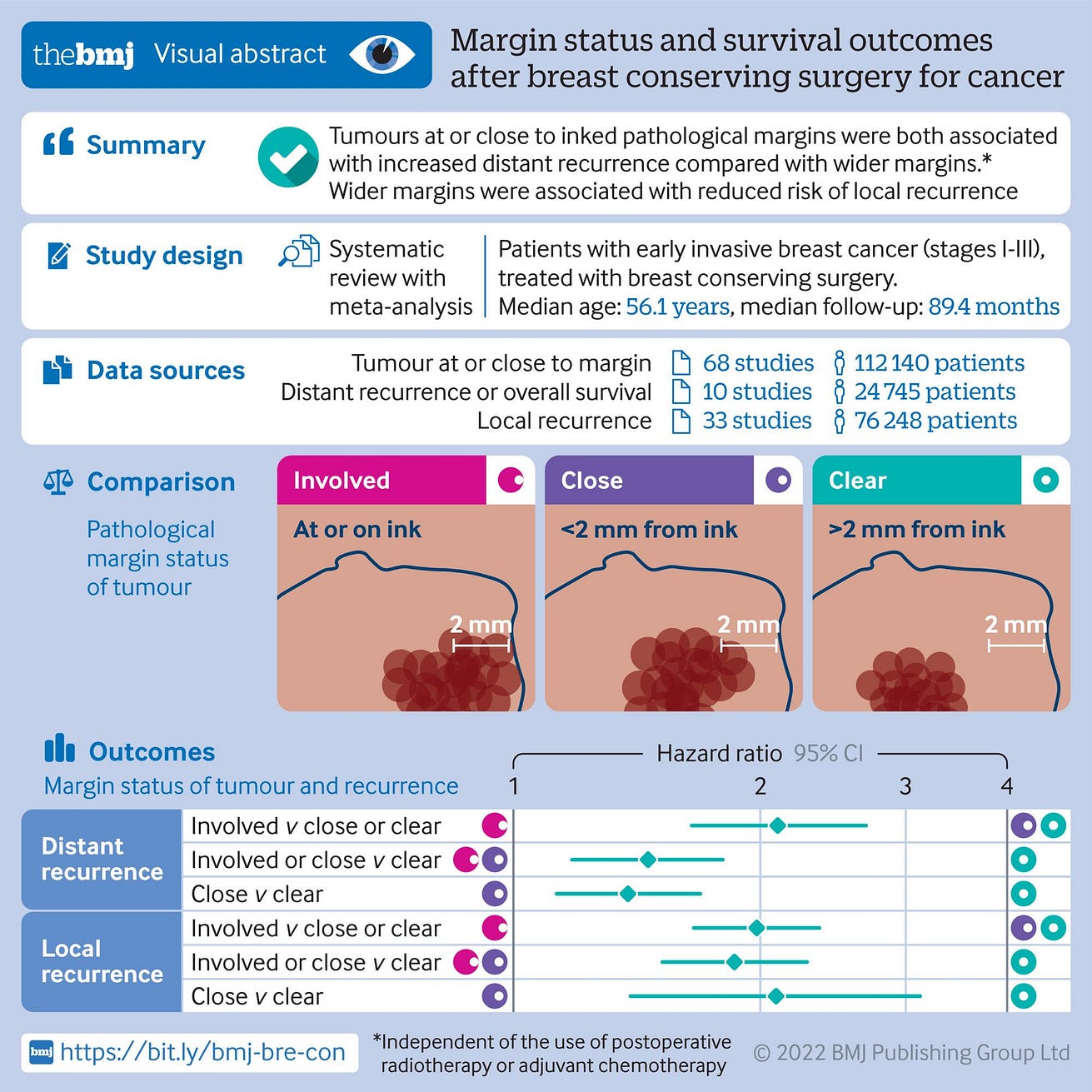
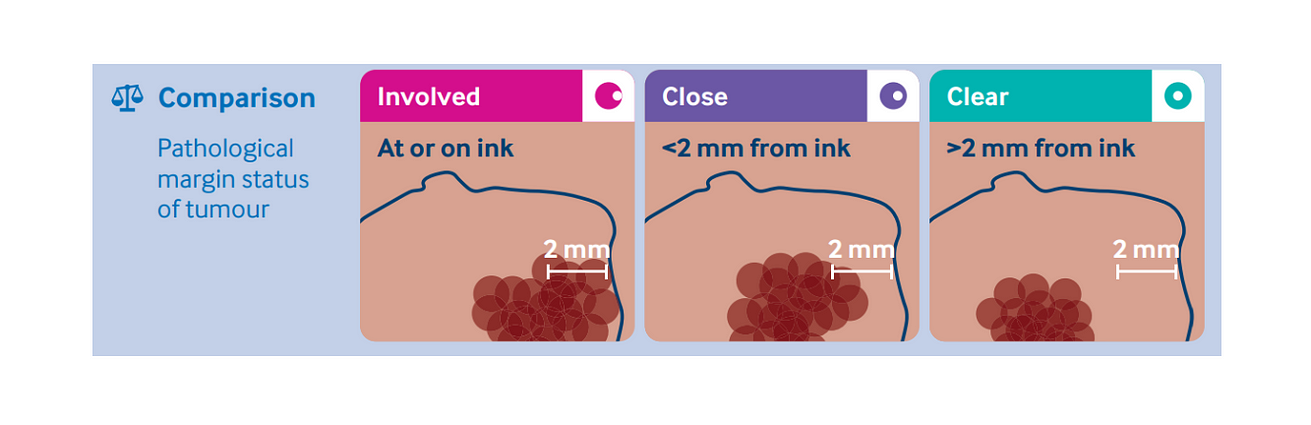
- Where applicable, margins were categorised as tumour on ink (involved), close margins (no tumour on ink but <2 mm), and negative margins (≥2 mm).
Results
- 68 studies from 1 January 1980 to 31 December 2021, comprising 112 140 patients with breast cancer, were included.
- Across all studies, 9.4% (95% confidence interval 6.8% to 12.8%) of patients had involved (tumour on ink) margins and 17.8% (13.0% to 23.9%) had tumour on ink or a close margin.
- The rate of distant recurrence was 25.4% (14.5% to 40.6%) in patients with tumour on ink, 8.4% (4.4% to 15.5%) in patients with tumour on ink or close, and 7.4% (3.9% to 13.6%) in patients with negative margins.
- Compared with negative margins, tumour on ink margins were associated with increased distant recurrence (hazard ratio 2.10, 95% confidence interval 1.65 to 2.69, P<0.001) and local recurrence (1.98, 1.66 to 2.36, P<0.001).
- Close margins were associated with increased distant recurrence (1.38, 1.13 to 1.69, P<0.001) and local recurrence (2.09, 1.39 to 3.13, P<0.001) compared with negative margins, after adjusting for receipt of adjuvant chemotherapy and radiotherapy.
- In five studies published since 2010, tumour on ink margins were associated with increased distant recurrence (2.41, 1.81 to 3.21, P<0.001) as were tumour on ink and close margins (1.44, 1.22 to 1.71, P<0.001) compared with negative margins.
Conclusions
- Involved or close pathological margins after breast conserving surgery for early stage, invasive breast cancer are associated with increased distant recurrence and local recurrence.
- Surgeons should aim to achieve a minimum clear margin of at least 1 mm.
- On the basis of current evidence, international guidelines should be revised.
Researchers are now calling for a review of international guidelines.
Infographic
ORIGINAL PUBLICATION (excerpt)
Margin status and survival outcomes after breast cancer conservation surgery: prospectively registered systematic review and meta-analysis
THE BMJ
James R Bundred,1,2 Sarah Michael,3,4 Beth Stuart,5 Ramsey I Cutress,5,6 Kerri Beckmann,7 Bernd Holleczek,8,9 Jane E Dahlstrom,10 Jacqui Gath,11 David Dodwell,12 Nigel J Bundred3,4
21 September 2022
Introduction
Pathological cancer specimens from breast conserving surgery are classified by a pathologist as involved if there is tumour at the edge of the specimen, implying that the specimen has been transected during surgery, or close if tumour is within a defined distance from the edge of the specimen or specimen margin, usually 1 mm or 2 mm.
Involved (tumour on ink or positive) or close (no tumour on ink to 2 mm) pathological margins after breast conserving surgery for early stage invasive breast cancer are associated with an increased risk of local recurrence.12 Patients who develop local recurrence have an increased risk of developing distant recurrence and of death from breast cancer.3 In 2014, American Society of Clinical Oncology4 stated that tumour (invasive cancer or ductal carcinoma in situ) not touching the ink at the specimen edge is acceptable to prevent local recurrence.45
The effect of margin involvement on distant recurrence or mortality is relatively unknown. A UK study of young women, aged 40 or younger, with early stage invasive breast cancer reported that in those undergoing breast conserving surgery, 239 (21%) of 1135 had margins of 1 mm or less, and this was associated with a 13.4% higher rate of distant recurrence and an 11.1% decrease in overall survival at five years compared with women who had margins of more than 1 mm.6 Positive margins worsen oncological outcomes, therefore avoiding these presents an achievable route to improve breast cancer outcomes.
We performed a systematic review and meta-analysis to determine the incidence of tumour on ink and close margins after breast conserving surgery and any association between margin involvement with subsequent distant recurrence and overall survival in early stage invasive breast cancer. We also aimed to update the evidence on the association between margin width and local recurrence.
Methods and additional information:
See the original publication
Results
See the original publication
DISCUSSION
Principal findings
This meta-analysis identified 68 studies comprising 112 140 women and provided evidence, for the first time to our knowledge, of associations between pathological margins and the risk of distant recurrence and mortality after breast conserving surgery.
This association was present despite adjustment for the use of postoperative radiotherapy and chemotherapy.
Positive or close margins were associated with increased distant recurrence, local recurrence, and lower overall survival compared with negative or wide margins and, importantly, close margins without tumour at ink were also associated with increased distant and local recurrence.
Strengths and weaknesses
This paper collates data from about four times the number of patients included in the 2014 meta-analysis, which addressed local recurrence and margins.1
This study is also the first to consider the association between distant recurrence and overall survival with margins.
Where tumours were at, or close to, the margin, risk of distant recurrence (and local recurrence) was increased, even in patients treated with adjuvant chemotherapy; a finding consistent across all the margin width comparisons.
Our analysis combined multivariable hazard ratios, the accepted standard for reporting time-to-event data, in preference to binary outcome data, avoiding bias introduced by the varying follow-up lengths of included studies.
Missing distant recurrence data not presented in studies were obtained in some cases by writing to authors directly.
Additionally, we conducted rigorous quality scoring of papers. Due to the study level nature of this analysis, we cannot fully exclude that differences in prognostic characteristics by margin group introduce confounding into our analyses; however, where possible, summary statistics meta-analysed were adjusted for commonly known potentially confounding factors.
Therefore, this association is probably independent of these factors. Additionally, subgrouping of only adequately adjusted studies provided results consistent with the overall results of the analysis.
Further studies could assess the impact of possible confounding factors, such as re-excision rates or boost radiotherapy, although boost radiotherapy has not been shown to affect distant recurrence or overall survival outcomes.
With the current practise of adjuvant systemic therapy for most patients with breast cancer, distant recurrence is the most frequent site of first relapse (rather than local recurrence).
Thus, most distant recurrence is not due to previous local recurrence.
Systemic therapy was associated with reduced distant recurrence rates in our meta-analysis but did not reduce the increased distant recurrence seen with involved margins (<1 mm).
Policy implications for breast cancer care
The American Society of Clinical Oncology guidelines in 2014 suggested that tumour margins (invasive cancer or ductal carcinoma in situ) not touching ink at the specimen edge are acceptable, but the relatively weak evidence available to address this issue was recognised.4
Our study does not support the overall conclusion expressed in these guidelines.
The American Society of Clinical Oncology guidelines in 2014 suggested that tumour margins (invasive cancer or ductal carcinoma in situ) not touching ink at the specimen edge are acceptable, but the relatively weak evidence available to address this issue was recognised.4
Our study does not support the overall conclusion expressed in these guidelines.
Most international guidelines54142 advise a threshold margin to reduce local recurrence.
Our study shows that margin proximity is associated with increased distant recurrence (as well as local recurrence), so the chosen margin width is important and should minimise distant recurrence.4
Some distant recurrences probably result from involved margins, and in the future, multidisciplinary team decisions about margin clearance width should ensure maximal prevention of distant recurrence.62143
A minimum margin of at least more than 1 mm was the margin required to minimise both distant recurrence and local recurrence in this analysis, taking into account the wider confidence intervals in our analyses of close versus negative margins.
The interplay between positive margins and chemotherapy on distant recurrence was analysed both as a metaregression and as a subgroup of studies, which had adjusted for use of chemotherapy.
Within both of these analyses, the association between positive or close margins and adverse oncological outcomes was not attenuated by chemotherapy.
Clear margins were associated with reduced distant recurrence by an absolute value of 5%5 across all studies, a level of benefit for which chemotherapy is commonly offered to patients as an adjuvant therapy.4445
The American Society of Clinical Oncology meta-analysis highlighted the importance of reducing re-excision rates after breast conserving surgery but its focus was on local not distant recurrence.4
Differing rates of margin clearance between different continents and countries might relate to uncertainty over optimal width of clearance in guidelines or to an overemphasis on cosmetic outcomes.
Since the widespread use of systemic therapy, four of the six studies (19 000 patients) considering margin status reported an increased distant recurrence with tumours close to or at inked margins.
A Dutch study from 1980–200819 included in our meta-analysis but with contrasting results to the other studies, had 15.7% missing margin status.
Additionally, less than 50% of included patients received systemic therapy and up to 20% received re-excision rates for positive or close margins, probably accounting for the reduced association between margin status and distant recurrence within this study.4346
A national audit of margin involvement and re-excision rates completed in the Netherlands, was associated with a margin involvement reduction to 2.1%, and reduced distant recurrence and local recurrence.4346
Similar prospective audits might be helpful in other countries where involved margin rates remain high.
Further study of the nature of margin involvement (invasive cancer or ductal carcinoma in situ) and which margins lead to increased distant recurrence is required but previous studies have suggested that neither type nor site of involvement mattered in the development of local recurrence.1517
Patient advocates stated a preference to minimise the risk of local and distant recurrence of breast cancer risk by ensuring a wider margin.
Recognising that wider margins require further surgery, decisions about re-excision should be the product of an informed discussion between clinicians and patients47 with full disclosure of the risks of increased distant recurrence associated with close margins.
Conclusions
We have conducted the largest meta-analysis of the association between margins after breast conserving surgery and outcomes, and show a relation between margin involvement, the development of metastatic disease, and poorer cancer survival.
If, as is likely, the association between margin involvement and higher distant recurrence and mortality is causal, a re-appraisal of existing international guidelines is needed.
These comprehensive data indicate the likelihood that inadequate margin widths result in higher risks of distant recurrence and breast cancer mortality, as well as increased local recurrence.
A margin of no tumour on ink is inadequate and we recommend a minimum tumour free distance of 1 mm from the margin for either invasive disease or ductal carcinoma in situ to ensure optimum oncological outcomes.
A margin of no tumour on ink is inadequate and we recommend a minimum tumour free distance of 1 mm from the margin for either invasive disease or ductal carcinoma in situ to ensure optimum oncological outcomes.
What is already known on this topic
- Oncology guidelines suggest that avoiding a tumour that touches ink margins after breast cancer surgery reduces local recurrence but no data exist for distant recurrence
- Whether width of excision margin is associated with distant cancer recurrence after breast conserving surgery for early invasive breast cancer is unknown
What this study adds
- Tumours at the inked margins (tumour on ink) or close margins (no tumour on ink, but tumour <2 mm) were associated with increased distant recurrence compared with wider margins, independent of the use of postoperative radiotherapy or adjuvant chemotherapy
- Wider margins were also associated with a reduced risk of local recurrence
- Margin width between tumour on ink and 2 mm is associated with increases in distant and local recurrence, and mortality after breast conserving surgery
References and additional information
See the original publication
About the authors & affiliations
James R Bundred, surgical trainee1 2,
Sarah Michael, foundation doctor3 4,
Beth Stuart, medical statistician5,
Ramsey I Cutress, professor of breast surgery5 6,
Kerri Beckmann, medical statistician7,
Bernd Holleczek, professor of epidemiology8 9,
Jane E Dahlstrom, professor of pathology10,
Jacqui Gath, patient group representative11,
David Dodwell, professor of oncology12,
Nigel J Bundred, professor of surgery3 4
Author affiliations
1Leeds Institute of Molecular Medicine,
University of Leeds, Leeds, UK
2Leeds Institute of Emergency Surgery, St James University Hospital, Leeds, UK
3Manchester University NHS Foundation Trust, Wythenshawe, Manchester, UK
4Division of Cancer sciences, University of Manchester, Manchester, UK
5Cancer Sciences, University of Southampton, Southampton, UK
6University Hospital Southampton, Southampton, UK
7Cancer Epidemiology and Population Health Research Group,
University of South Australia, Adelaide, SA, Australia
8Division of Clinical Epidemiology Aging Research,
German Cancer Research Centre (DKFZ), Heidelberg, Germany
9Saarland Cancer Registry, Saarbrücken, Germany
10ACT Pathology, Canberra Health Services and
Australian National University Medical School, ACT, Australia
11Independent Cancer Patients’ Voice, London, UK
12Nuffield Department of Population Health,
University of Oxford, Oxford, UK
Originally published at https://www.bmj.com/content/378/bmj-2022-070346
BMJ 2022; 378 doi: https://doi.org/10.1136/bmj-2022-070346
Published 21 September 2022