This is an excerpt from the paper “Can NHS hospitals do more with less?”, published by the Nuffield Trust in 2012; focused in Operational Processes. (Despite of a 9 years old report, most fundamentals are still valid)
Nuffield Trust
December 1, 2012
Dr Jennifer Dixon CBE;
Jeremy Hurst;
Professor Judith Smith;
Sally Williams
Excerpt extracted by: Joaquim Cardoso, MSc.
credit to the image on top: sequence health
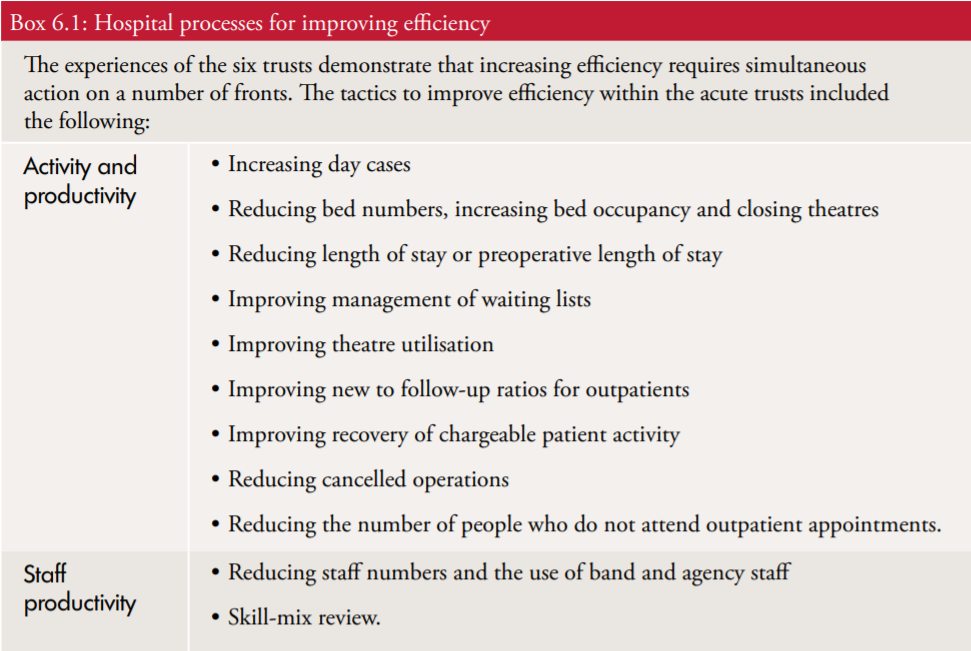
Here we turn to the heart of the efficiency question: hospital processes, examining hospital processes that appear to have been associated with gains in productivity, including, other than workforce productivity itself.
- expanding activity despite a squeeze on resources
- getting care right first time
- increasing day-case surgery
- shortening length of stay
- managing estate costs
Key points
- At the heart of the hospital efficiency question is the potential to change the processes of production to increase outputs for given inputs, or to reduce inputs for given outputs. The possibilities will depend on the initial conditions in a hospital, the timescale available for change and external circumstances
- Historically, it seems that activity increases have been the main source of improvements in crude productivity in NHS hospitals during budgetary contractions. During the forthcoming contraction, if activity increases are constrained successfully, there will be additional pressure to reduce costs. Failing this, the crude efficiency gains may be smaller than has been observed in the past.
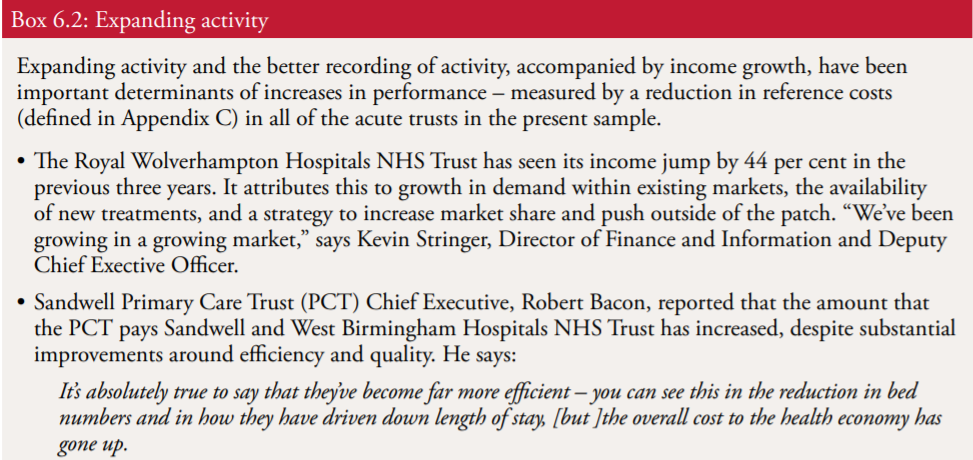
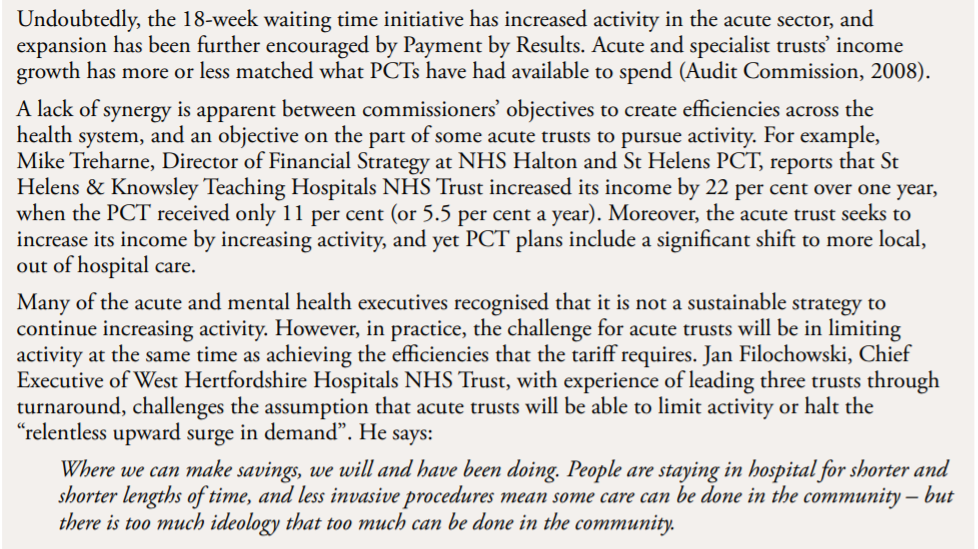
- Expanding activity and better recording of activity have been important determinants of the reduction in reference costs (defined in Appendix C) in all of the acute trusts in the research sample. Their experience relates to a period of general expansion in the NHS. Looking ahead, the emphasis will be on cash-releasing savings.
- The weight of cross-sectional and longitudinal evidence from the US suggests that quality of care in hospitals is positively associated with efficiency. This may be due partly to a direct association — involving ‘getting things right first time’ — and partly to indirect associations involving variations in management effectiveness and in the speed of adoption of new technologies across hospitals.
- The present research found strong and consistent support among executives in the study sites for avoidance of harm and ‘getting things right first time’. All of the trusts in the study had invested in quality and safety initiatives.
- Reducing average length of stay and raising day case rates have added greatly to acute hospital efficiency in the past. However, the acute length of stay in the UK appears to remain well above the OECD average — perhaps because of a relative lack of intermediate and long-term care.
- Past efficiency gains in the HCHS have been associated with bed reductions and hospital consolidation and closures. All of the ‘turnaround’ trusts that this study examined had reduced bed numbers.
- Closing whole sites is the best way to save costs, but hospital closures are unpopular and they raise complex trade-offs.
- Although the literature on the gains from hospital mergers is mixed, it has been suggested that significant efficiency improvements could be made if NHS organisations were to cooperate in the provision of back office functions.
Hospital processes
Improving hospital efficiency is a matter of changing productive processes to increase output (including quality) for any given level of inputs, or to reduce one or more input for any given output.
The weight of evidence from recent US studies…points to the existence of positive statistical associations between quality and efficiency
The opportunities to improve efficiency in any one hospital will depend very much on the initial conditions in that hospital: for example, on whether there is slack in any inputs, whether there are problems with the quality of care, whether a sub-optimal mix of inputs has been chosen or whether there has been failure to adopt the most cost-effective set of affordable technologies.
They will depend also on the timescale available for change: in the short run, some resources and costs will be fixed; in the long run, all resources and costs can be varied.
Moreover, the opportunities will depend on changing external circumstances such as whether demand or budgets are expanding or contracting, and whether new, cost-effective and affordable technologies have become available.
Experience suggests that invariably there is variation across hospitals in the relevant parameters, and that usually benchmarking can help to point towards the efficiency frontier.
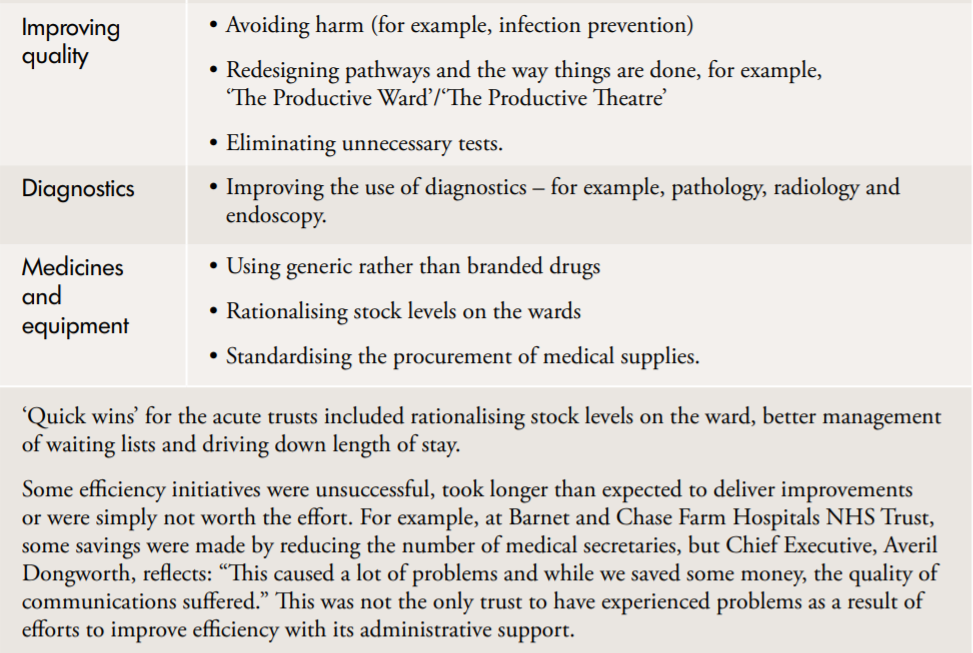
Expanding activity versus reducing costs
From 2009 the NHS was required to switch, in effect, from seeking efficiency gains that could boost activity and quality in the circumstances of rising total expenditure, to seeking efficiency gains that would realise expenditure savings, to be reinvested in quality and innovation, in the circumstances of stationary total expenditure.
Efficiency can rise because activity increases faster than costs, or falls less rapidly than costs. As has been noted previously, there is ample evidence that crude hospital productivity has increased at times of financial squeeze in various health systems due to rising activity (Appleby, 1999[1]; Bazzoli and others, 2004–05[2]). It follows that during contractions, for any increase in hospital efficiency, cost reductions will be incentivised if activity rises are constrained or discouraged. Presumably this is part of the logic behind the measures which are intended to restrain the growth in hospital activity as set out in The Operating Framework for the NHS in England 2010/11 (Department of Health, 2009a[3]). At the same time, if activity restraint is successful, it may inhibit some of the crude efficiency ‘bounce’ which has been traditionally associated with NHS contractions. However, it is possible that quality gains might be higher than in previous ‘bounces’ if savings are successfully recycled into new technologies.
Getting care right first time
It has been often suggested that avoiding harm and promoting quality of care in health care will improve efficiency because ‘doing things right first time’ will avoid unnecessary costs, as well as achieving good clinical outcomes and patient satisfaction. However, it can be pointed out that raising quality beyond a certain point is likely to add more to costs than to benefits, thereby reducing efficiency. To what extent are quality and efficiency complementary, and to what extent are they in competition with one another?7
The weight of evidence from recent US studies that have examined both clinical quality of care (measured partially and in various ways) and efficiency (measured by frontier techniques) across US hospitals, points to the existence of positive statistical associations between quality and efficiency after controlling for other measurable factors (see Deily and McKay, 2006[4]; Harrison and Coppola, 2007[5]; Huerta and others, 2008[6]; Nayar and Ozcan, 2008[7]; Valdmanis and others, 2008[8]). In addition, as noted previously, Skinner and Staiger (2009)[9] found evidence of a positive association between quality and efficiency (or strictly, an inverse association between quality and cost) in their interrogation of 2.8 million longitudinal Medicare records for heart attack patients in the US.
In contrast, Jha and others (2009)[10] found modestly worse process quality for certain conditions in low-cost hospitals in the US but comparable rates of risk-adjusted mortality, where efficiency was measured using the ratio of observed to expected cost per case. Pink and others (2003)[11] found that patient satisfaction in hospitals in Ontario was inversely associated with the ratio of actual to expected cost per case, although the magnitude of the effect was small and it was swamped by the effects of other hospital characteristics on satisfaction.
If all hospitals were equally efficient and remained so, negative associations would be found between clinical quality and efficiency because activity and quality would have to be traded off for given inputs, or quality and costs would have to be traded off for given activity. However, it appears that hospitals are far from equally efficient, probably because of differences, among other things, in their management culture and/or their rate of adoption of new, cost-effective, affordable technologies. This makes it possible for an indirect and positive association to appear between efficiency and quality, as both react favourably to better management and the speedier adoption of cost-effective technologies.
It has been estimated that adverse events occur in 1 to 3 per cent of all hospital admissions
Where does this leave the argument that there is a direct connection between quality and efficiency — because ‘doing things right first time’ and avoiding adverse events can save costs? Of course, there is much evidence about alarmingly high rates of adverse events in hospitals and about the overuse, underuse and misuse of hospital procedures. For example, it has been estimated that adverse events occur in 1 to 3 per cent of all hospital admissions, according to studies from a variety of countries — far above the level in other potentially risky industries such as aviation (Kohn and others, 1999[13]; Mattke, 2004[14]). It is clear from the US literature that adverse events are associated with excess deaths and excess charges per admission (Zhan and Miller, 2003[15]). They are associated also with excess re-admissions (Friedman and others, 2009[16]). However, interventions to raise quality themselves will have costs, and it is an open question in each instance as to whether the benefit gains and cost savings from such interventions will exceed the initial outlay. In an American review article, Kilpatrick and others (2005)[17] concluded that there was simply not enough evidence to establish whether there is a business case for most quality interventions: that is, whether positive financial returns are available.8
In his report for the Health Foundation in the UK, Ovretveit (2009)[18] came to a similar conclusion about the general lack of evidence to establish that quality interventions can save costs. Nevertheless, he identifies a shortlist of quality interventions for which net savings have been established. Of course, it is not necessary for quality interventions to save money for them to be worth adopting, on paper — they merely have to be more cost-effective than alternative uses of resources. However, at a time of dwindling overall resources, it may be difficult for new quality initiatives that incur additional costs to displace established, if less cost-effective, uses of resources.
As noted previously, a study by Valdmanis and others (2008)[19] is among those which have found a positive relationship between quality and efficiency in American hospitals. This study established that the 1,377 hospitals in the sample could have increased the total amount of outputs by 26 per cent on average in 2004 by eliminating inefficiency. Only about 3 percentage points of this inefficiency was due to adverse events sensitive to nurse staffing in the hospitals — the measure of quality used in the study — suggesting that the direct effects of quality on inefficiency which were identified were relatively small.
Increasing day surgery and reducing length of stay
Two important process changes which can permit activity to be increased and inputs to be reduced are increasing the day surgery rate and reducing the average length of stay in hospitals. It is clear from studies such as the National Beds Inquiry (Department of Health, 2000)[20] that the gains in productivity in the Hospital and Community Health Services (HCHS) in the 1980s and 1990s, as noted previously, were due at least partly to a combination of rising day surgery and falling length of stay. At a time (1980–94) when overall admissions were rising by 3.4 per cent a year, day surgery admission rose by 12.4 per cent a year, whereas average length of stay fell by 3.3 per cent a year. Partly as a result of these two trends, the number of acute and general beds fell by 2.6 per cent a year over the same period.9
The efficiency benefits included
- reductions in length of stay by 2.2 days and
- in the use of costly antibiotics. Millar recalls:
Six months later we saw the money come falling out of the sky. Length of stay was going down, costs in imaging, diagnostics and antibiotic therapy were all coming down.
The savings in bed days enabled the Trust to reduce its bed base by 200. On C.difficile alone it claims to have saved 212 lives annually and 16,000 bed days, equating to £7.8 million in savings. It is now extending its focus to preventing other types of harm, including patient falls, medication errors, peri-operative care and the deteriorating patient.
The executives at the six trusts demonstrated a genuine commitment to preserving quality, and regarded it as a business imperative that would be important in future to attracting scarce resource. In critical times, the onus on the NHS to make the right decisions, first time, will become even greater.
Although average acute length of stay has declined for many years in the UK, recent OECD comparisons (which exclude day cases) suggest that average stay in the UK, at 7.2 days in 2007, remained well above the OECD average at 6.5 days. The US reported 5.5 days, Sweden reported 4.5 days and Denmark 3.5 days (OECD, 2009)[21]. Denmark, incidentally, is a country which is renowned for the quantity and quality of its long-term care services. It also has a significant number of specialists working in the community outside hospitals (Hurst, 2002)[22]. These comparisons suggest that there may be scope for further reductions in average length of stay in the UK — perhaps depending on the provision of additional domiciliary, residential and nursing home capacity.10 The NHS Institute, like its predecessor, the NHS Modernisation Agency, continues to advocate increases in day surgery and reductions in length of stay on a shortlist of areas with potential for productivity improvements (NHS Institute for Innovation and Improvement, 2006)[23].
There is evidence from the US literature that shorter length of stay has played a part in improving efficiency
There is evidence from the US literature that shorter length of stay has played a part in improving efficiency in US hospitals. As noted previously, Rosko (2004)[24] found an increase in efficiency in a sample of US teaching hospitals following implementation of the Balanced Budget Act in 1997. Younis and Forgione (2009)[25] looked at approximately 4,000 hospitals over the period 1996–2000 and found a reduction in average length of stay for Medicare patients following implementation of the Act, after controlling for other determinants of length of stay. Bazzoli and others (2004–05)[26], who examined the effect of the Act on 1,218 acute, non-profit hospitals between 1996 and 1999, also reported reductions in length of stay, but found no difference in the rate of reduction between hospitals experiencing more financial pressure and those experiencing less.
A Norwegian study (Martinussen and Midttun, 2004)[27], which used frontier techniques to measure variations in hospital efficiency across 51 hospitals, has suggested that increasing day surgery was positively and significantly linked to hospital efficiency over the period 1999–2001, after controlling for certain other determinants of efficiency. More specifically, an increase in the day surgery rate of about 10 per cent was associated with an increase in the efficiency index of 1.64 percentage points. Unexpectedly long lengths of stay were negatively associated with efficiency. This study was not able to control for quality or to take account of any whole-system effects.
The NHS Institute provides data, which is regularly updated, for NHS acute providers to benchmark themselves in respect of length of stay and day case surgery rates (among other indicators). It also provides estimates of the savings that could be made if lengths of stay above the median were reduced by 25 per cent and day surgery rates below the upper quartile were increased to the upper quartile (see NHS Institute for Innovation and Improvement, 2009)[28].
Bed numbers, Private Finance Initiative schemes and efficiency in estate use
The period of gains in the efficiency of the NHS in the 1990s was associated with bed reductions (Department of Health, 2000)[30]. To the extent that the current NHS operating framework (Department of Health, 2009a)[31] will put downward pressure on both the volume of growth and the price of hospital services over the next three to four years, eventually reductions in capacity will be necessary if trusts are to remain efficient. However, it will be difficult to reduce capital inputs such as buildings and land over such a period, especially if only parts of a site become surplus to requirements. Wards and other facilities can be closed or mothballed, but capital charges can remain. In other words, at times of contraction, building and land costs can impose diseconomies if services are not concentrated on fewer sites, for example. The NHS Confederation has pointed out that it will assist in making savings if whole sites can be closed, and The King’s Fund has concluded that reconfiguration across hospital sites is the only way that some trusts can achieve financial balance while avoiding unacceptable deterioration in quality of care over the next five years (Palmer, 2011)[32].
If downsizing is expected to be permanent or there are already plans in the pipeline for rationalising facilities which can be modified, it may be possible to concentrate services on fewer sites, at least in large urban areas, in the required timescale, thereby releasing buildings and land and restoring the remaining hospitals to something like their former average size before the contraction. However, from a whole-system viewpoint, such concentration is likely to have adverse effects for patient access. In addition, it may have adverse effects for competition, which could impact negatively on efficiency, judging by some of the studies cited elsewhere in this report.
Private Finance Initiative (PFI) schemes, which provide, typically, private premises, equipment and cleaning and catering services to the NHS on long-term contracts, represent a new and growing challenge in the search for savings. There are approximately 100 PFI schemes in the NHS at the time of writing, and there are more in the pipeline. PFI schemes can commit trusts to substantial annual payments for up to 30 years. They usually cost more than the equivalent public provision — perhaps because they provide a higher standard of service — and they frequently represent between 5 per cent and 15 per cent of a PFI trust’s income. The Audit Commission (2006)[33] has identified an association between large new building projects (mostly PFI schemes) and financial deficits in the NHS. There is relatively little flexibility in PFI contracts, and because of this it has been suggested that there will be pressure to concentrate hospital activity on PFI sites at the expense of non-PFI sites if there is contraction (Hellowell and Pollock, 2007)[34].
In addition, there is the question of reducing waste in the NHS estate. In a novel and preliminary analysis, May and Price (2009)[35] used frontier analysis to compare total income and patient-occupied area per unit site-area across 115 acute trusts, among others.
Of the trusts, 92 appeared to be more than 10 per cent inefficient, and 63 were more than 20 per cent inefficient. May and Price estimate that wasted space across the whole NHS estate might be costing £500 million a year.
Economies of scale, hospital mergers and sharing back office functions
To the extent that there are already plans to rationalise hospital capacity in the pipeline which can be accelerated, and to the extent that there is space that can be freed up on some existing sites, there may be the possibility to go further and concentrate services on even fewer sites than would be required to adjust for contraction, thereby increasing the average size of hospital. This raises the question of the existence of economies or diseconomies of scale in hospitals.
Operating hospitals at the right scale and with an optimum mix of departments can be an important source of efficiency. However, from a whole-system viewpoint, if the scale of operations is to be changed, there will be trade-offs to be considered between clinical quality, cost per case and access for patients (Bloor and others, 2000)[36]. As hospitals increase in size and decline in numbers in any given geographical area, there may be gains in clinical quality (from volume and clinical concentration effects); there may be other economies or diseconomies in scale which affect cost per case; and there will be reductions in access for patients, as the average distance of the population from the hospitals increases.
There is a voluminous literature relating to a wide range of diseases, which finds positive associations between clinical outcomes and the volume of specific treatments undertaken across hospitals. However, comprehensive, critical reviews of this literature both in the US (Halm and others, 2002)[37] and in the UK (NHS Centre for Reviews and Dissemination, 1996)[38] have concluded that many of the studies lack methodological rigour, mainly due to inadequate risk adjustment. Patient selection may explain some or all of the positive associations found between volume and outcomes. The studies which control better for risk tend to find smaller effects.
There is also a large literature on the effect of changes in size on unit costs in hospitals. Reviews suggest that cost per case declines as hospitals increase in size to about 200 beds. There appear to be roughly constant returns to scale between 200 and 600 beds; however, above approximately 600 beds diseconomies of scale seem to set in, possibly because larger hospitals become more difficult to manage. All of the studies concerned make either no measurement or incomplete measurement of the quality of care.
It is for policy-makers to weigh the likely trade-offs that exist between clinical quality, cost per case, access costs and competition as hospitals increase in size
In addition, there is copious evidence that patient access declines with distance from hospital (‘distance decay’). The evidence on the effects of this on outcomes is mixed. However, concentration of hospitals almost certainly transfers costs from hospitals to patients, as access becomes more difficult for some.
Moreover, there may be deleterious effects on efficiency through the weakening of competition if there are fewer hospitals further apart. It is for policy-makers to weigh the likely trade-offs that exist between clinical quality, cost per case, access costs and competition as hospitals increase in size.
There are a handful of studies (such as Harris and others, 2000[39]; Ferrier and Valdmanis, 2004[40]; Fulop and others, 2005[41]; Kjekshus and Hagen, 2007[42]), some using frontier techniques, which have investigated the effect of hospital mergers on the efficiency of hospitals, but the results fail to find statistical significance or are mixed. Dickinson and others (2006)[43] reviewed the literature on best practice in organisational mergers and transitions from an NHS perspective, and identified a need for different styles of management at specific stages in the merger process. They also identified a need for a relentless focus on management of the human aspects of transition, in order to mitigate the likely dips in performance that come with a process of major organisational change.
One way that economies of scale may be achieved is through hospital cooperation, which does not actually involve consolidation of all services on one site, at least in the short run, but allows a reduction in the duplication of services — such as back office services — and concentration of purchasing power. As part of the QIPP national workstream, the Foundation Trust Network has reviewed the scope for making efficiencies in NHS back office functions such as finance, human resources, information management and technology and estates. It has identified the scope for releasing potentially £600 million a year for front-line services by sharing back office functions across NHS organisations, and by other methods of streamlining such services (Foundation Trust Network, 2010)[44].
References
[1] Appleby J (1999) ‘Government funding of the UK National Health Service: what does the historical record reveal?’, Journal of Health Service Research and Policy 4(2), 79–89.
[2] Bazzoli GJ, Lindrooth R, Hasnain-Wynia R and Needleman J (2004–05) ‘The Balanced Budget Act of 1997 and US hospital operations’, Inquiry 41(4), 401–17.
[3] Department of Health (2009a) The Operating Framework for the NHS in England 2010/11. London: Department of Health.
[4] Deily M and McKay N (2006) ‘Cost inefficiency and mortality rates in Florida hospitals’, Health Economics 15(4), 419–31.
[5] Harrison J and Coppola N (2007) ‘Is the quality of hospital care a function of leadership?’, The Health Care Manager 26(3), 263–72.
[6] Huerta T, Ford E, Peterson l and Brigham K (2008) ‘Testing the hospital value proposition: an empirical analysis of efficiency and quality’, Health Care Management Review 33(4), 1–9.
[7] Nayar P and Ozcan Y (2008) ‘Data envelopment analysis comparison of hospital efficiency and quality’, Journal of Medical Systems 32(3): 193–9.
[8] Valdmanis V, Rosko M and Mutter R (2008) ‘Hospital quality, efficiency, and input slack differentials’, Health Services Research 43(5), 1830–48
[9] Skinner J and Staiger D (2009) Technology Diffusion and Productivity Growth in Health Care. National Bureau of Economic Research Working Paper No 14865. Cambridge, MA: National Bureau of Economic Research.
[10] Jha A, Orav J, Dobson A, Book R and Epstein A (2009) ‘Measuring efficiency: the association of hospital costs and quality of care’, Health Affairs 28(3), 897–906.
[11] Pink G, Murray M and McKillop I (2003) ‘Hospital efficiency and patient satisfaction’, Health Services Management Research 16(1): 24–38.
[12] Audit Commission (2008) The Right Result? Payment by Results 2003–2007. London: Audit Commission.
[13] Kohn L, Corrigan J and Donaldson M eds (1999) To Err Is Human: Building a safer health system. Washington, DC: National Academy Press.
[14] Mattke S (2004) ‘Monitoring and improving the technical quality of medical care’, in OECD, Towards High Performing Health Systems: Policy studies. Paris: OECD.
[15] Zhan C and Miller MR (2003) ‘Excess length of stay, charges and mortality attributable to medical injuries during hospitalisation’, Journal of the American Medical Association 290(14): 1868–74.
[16] Friedman B, Encinosa W, Jiang J and Mutter R (2009) ‘Do patient safety events increase readmissions?’, Medical Care 47(5), 583–90.
[17] Kilpatrick K, Lohr K, Leatherman S, Pink G, Buckel J, Legarde C and Whitener L (2005) ‘The insufficiency of evidence to establish the business case for quality’, International Journal for Quality in Health Care 17(4), 347–55.
[18] Ovretveit J (2009) Does Improving Quality Save Money? London: The Health Foundation.
[19] Valdmanis V, Rosko M and Mutter R (2008) ‘Hospital quality, efficiency, and input slack differentials’, Health Services Research 43(5), 1830–48.
[20] Department of Health (2000) Shaping the Future NHS: Long term planning for hospitals and related services: Consultation document on the findings of the National Beds Inquiry — supporting analysis. London: Department of Health.
[21] OECD (2009) ‘Health at a glance 2009’. www.oecd. org/health/healthataglance . Accessed 30 March 2010.
[22] Hurst J (2002) ‘The Danish health care system from a British perspective’, Health Policy 59(2), 133–43.
[23] NHS Institute for Innovation and Improvement (2006) Delivering Quality and Value: Focus on: productivity and efficiency. London: Department of Health.
[24] Rosko M (2004) ‘Performance of US teaching hospitals: a panel analysis of cost inefficiency’, Health Care Management Science 7(1): 7–16.
[25] Younis M and Forgione D (2009) ‘The relationship between the Balanced Budget Act and length of stay for Medicare patients in US hospitals’, European Journal of Health Economics 10(1): 57–63.
[26] Bazzoli GJ, Lindrooth R, Hasnain-Wynia R and Needleman J (2004–05) ‘The Balanced Budget Act of 1997 and US hospital operations’, Inquiry 41(4), 401–17.
[27] Martinussen P and Midttun L (2004) ‘Day surgery and hospital efficiency’, Health Policy 68(2): 183–96.
[28] NHS Institute for Innovation and Improvement (2009) Converting the Potential into Reality: 10 steps a provider can take to realise the benefits of Better Care, Better Value indicators. London: Department of Health. www.library.nhs.uk/Improvement/ ViewResource.aspx?resID=332251 . Accessed 4 April 2011.
[29] Barnet and Chase Farm Hospitals NHS Trust (2007) Annual Report 2006/07.
[30] Department of Health (2000) Shaping the Future NHS: Long term planning for hospitals and related services: Consultation document on the findings of the National Beds Inquiry — supporting analysis. London: Department of Health.
[31] Department of Health (2009a) The Operating Framework for the NHS in England 2010/11. London: Department of Health.
[32] Palmer K (2011) Reconfiguring Hospital Services: Lessons from South East London. London: The King’s Fund.
[33] Audit Commission (2006) Learning the Lessons from Financial Failure in the NHS. London: Audit Commission.
[34] Hellowell M and Pollock A (2007) Private Finance, Public Deficits: A report on the cost of PFI and its impact on health services in England. Edinburgh: Centre for International Health Policy.
[35] May D and Price I (2009) ‘A revised approach to performance measurement for health care estates’, Health Services Management Research 22(4), 151–7.
[36] Bloor K, Barton G and Maynard A (2000) The Future of Hospital Services: Management updates. London: The Stationery Office
[37] Halm E, Less C and Chassin M (2002) ‘Is volume related to outcome in health care? A systematic review and methodologic critique of the literature’, Annals of Internal Medicine 137(6), 511–20.
[38] NHS Centre for Reviews and Dissemination (1996) ‘Hospital volume and health care outcomes, costs and patient access’, Effective Health Care 2(8), 1–16.
[39] Harris J, Ozgen H and Ozcan Y (2000) ‘Do mergers enhance the performance of hospital efficiency?’, Journal of the Operational Research Society 51(7): 801–11.
[40] Ferrier G and Valdmanis V (2004) ‘Do mergers improve hospital productivity?’, Journal of the Operational Research Society 55(10): 1071–80.
[41] Fulop N, Protopsaltis G, King A, Allen P, Hutchings A and Normand C (2005) ‘Changing organizations: a study of the contexts and processes of mergers of health care providers in England’, Social Science and Medicine 60(1), 119–30.
[42] Kjekshus L and Hagen T (2007) ‘Do hospital mergers increase hospital efficiency? Evidence from a National Health Service country’, Journal of Health Services Research and Policy 12(4), 230–5.
[43] Dickinson H, Peck E and Smith J (2006) Leadership in Organisational Transition: What can we learn from research evidence? Summary Report. Birmingham: Health Services Management Centre, University of Birmingham.
[44] Foundation Trust Network (2010) QIPP National Workstream: Back office efficiency and management optimisation. London: Department of Health. www.dh.gov.uk/prod_consum_dh/groups/dh_ digitalassets/@dh/@en/@ps/documents/digitalasset/ dh_124878.pdf . Accessed 1 April 2011.
Originally published at:https://www.nuffieldtrust.org.uk












