A policy report by All.Can International
27 May 2021
This report has been produced by The Health Policy Partnership and The Health Value Alliance on behalf of All.Can International.
Key messages
by Joaquim Cardoso MSc.
Chief Strategy Officer (CSO)
Strategic Cancer Management — multidisciplinary institute
March 4, 2022
- Data are central to quality, innovation and overall efficiency in cancer care
- We are still far from fully harnessing the potential of data to transform cancer care
- Overcoming existing challenges is integral to ensuring sustainability of cancer care

Harnessing data for better cancer care — Executive Summary
A policy report by All.Can International
27 May 2021
This report has been produced by The Health Policy Partnership and The Health Value Alliance on behalf of All.Can International.
About this report
This report aims to offer policymakers, care providers and decision-makers a forward-looking view of opportunities for optimising the use of data to improve efficiency in cancer care.
It starts by defining data and investigating the current role of data in cancer care.
It then describes where data have contributed to improving patient outcomes and efficiency across the cancer care pathway, focusing in particular on their role in addressing inefficiencies viewed as important to cancer patients and their caregivers, based on previous All.Can research.
The report then discusses the challenges that remain in optimising the use of data and provides recommendations for policymakers to overcome these challenges.
Executive summary
Data are central to quality, innovation and overall efficiency in cancer care
Over the past decades there has been considerable progress in cancer care, with many advances enabled by high-quality data.
Having timely access to data has become essential to driving meaningful research, enabling efficient models of care, and improving quality and outcomes for patients.
Innovations in the way we use and collect data, as well as our ability to draw insights from data, offer the potential to improve efficiency at every stage of the care pathway (Figure a).
Figure a. Summary overview of the role of data in driving efficiency at every stage of the cancer care pathway
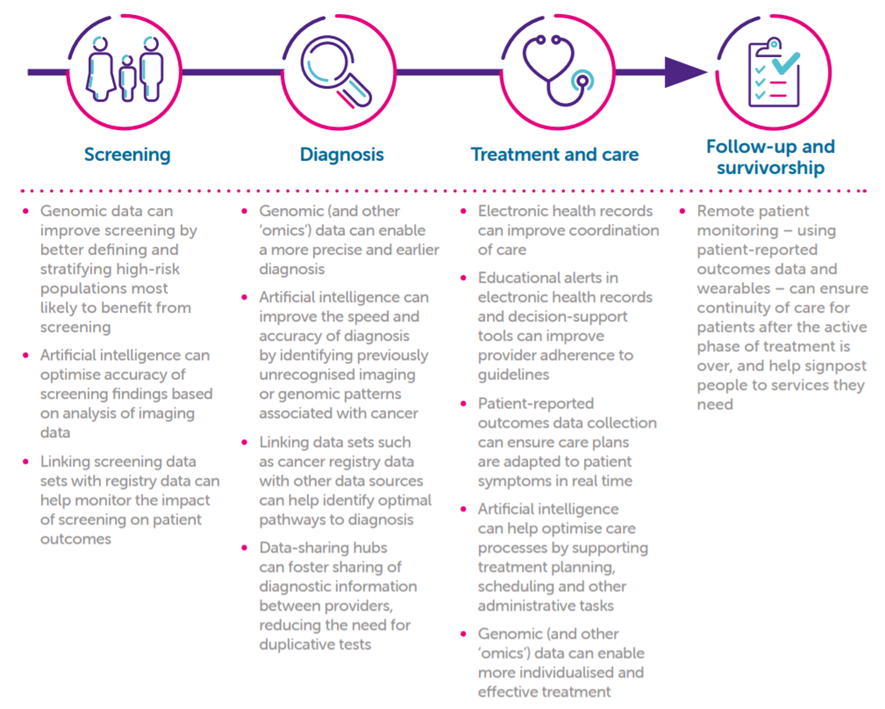
This figure summarises literature review findings from chapter 4, and does not aim to cover the entire realm of data in cancer care
We are still far from fully harnessing the potential of data to transform cancer care
The notion of ‘data rich, information poor’ rings true in cancer care, and many data challenges persist: in data themselves, the systems used to collect them, integrating data into clinical care and using data to draw meaningful insights to drive change.
Common challenges with cancer data include (but are not limited to) those outlined in Figure b.
Figure b. Challenges to achieving the optimal use of data in cancer care

Overcoming existing challenges is integral to ensuring sustainability of cancer care
The COVID-19 pandemic has focused the world’s attention on the role of data in addressing some of the biggest challenges in healthcare and, equally, in cancer care.
As we look to post-pandemic recovery, policymakers are presented with a unique opportunity to build more sustainable, resilient and efficient systems of care, leaving nobody behind. Addressing the challenges in data is essential to achieving this goal.

Call to action
As part of the digitisation agenda, policymakers must implement lasting changes across systems of care and policy frameworks to enable data to achieve their full potential for the benefit of all people with cancer.
Commitment is needed to embed optimal use of data across all facets of cancer care, in all settings, for all people living with and beyond cancer.
Data quality
- Create national cancer data quality standards and build them into regular, mandatory auditing of cancer care.
- Implement technological solutions for automatic data entry, minimising the risk of human error and administrative burden on care teams.
Data equity
- Demand greater equity in cancer research and care by ensuring appropriate representation of people of different races and ethnicities, sex and cancer types in cancer data sets.
- Hold institutions accountable for providing equitable cancer care by capturing performance on key quality indicators according to patients’ race, ethnicity, sex and socioeconomic status in accreditation systems.
- Ensure proportionate allocation of funds towards specialist cancer registries to collect data on populations of cancer patients for whom data are less available.
Patient-relevant data collection
·
- Encourage systematic and standardised collection of patient-generated health data, such as measures of patient-reported outcomes and patient experience, in key national health data sets.
- Include these data in regular monitoring and performance evaluations of cancer care to guide improvements to care most relevant to patients.
Interoperability
- Develop common data standards, specifications and processes to improve the national and international interoperability of data sets.
- Scale-up existing national and international initiatives on data standardisation and interoperability
Health data governance
·
- Build harmonised data governance legislation to facilitate health data linking and sharing between providers, and ideally between countries.
- Enable the creation of federated data networks when national and international data linkages are not possible.
- Invest in creating national health data codes of conduct to facilitate the safe use of health data, limiting barriers to data sharing while protecting patient privacy.
Data burden on healthcare professionals
- Build in positive incentives for data collection and use across the cancer care pathway, to foster a culture of value-based healthcare.
- Embed data-analytic solutions into care processes to enable rapid processing and feedback of data insights to clinical teams to guide decision-making.
- Provide appropriate funding and resourcing to train and upskill the healthcare workforce so that they keep pace with innovations in data collection and use.
Patient trust
- Create public awareness and education campaigns to convey the power of meaningful data to better manage cancer care.
- Engage with patients to discuss how data are being used, and address misconceptions around the nefarious use of health data.
- Continuously adapt legislation and tools to give citizens appropriate control over their own health data, so they may act as their own data ‘gatekeepers’.
Drawing insights from data
- Apply appropriate regulatory standards to fundamentally protect citizens’ rights and values by ensuring that:
o data sets from which insights are drawn are adequate, equitable and sufficiently representative to train artificial intelligence algorithms while minimising potential biases
o the analytics used (including artificial intelligence algorithms) are standardised, transparent and subject to rigorous evaluations of clinical safety and effectiveness
o the insights drawn from data analysis are of high quality

Introduction
Cancer care is advancing at a speed never seen before, and data are at the core of many of these advances.
With an increasingly rich array of data at our disposal, we are seeing the potential for more accurate diagnosis, personalised treatment and better insights on the impact of treatment and care for patients.
Mobile applications and smart devices now enable the collection of health data in a person’s daily life outside of the clinical setting, allowing for remote monitoring and identifying critical health events sooner.
Advances in data analytics, facilitated by artificial intelligence (AI), machine learning and improvements in data processing, are helping us solve some of the most complex challenges in healthcare at a scale and speed that were previously impossible.
Many of these advances are still in early stages of implementation, but could be transformational to the future of cancer care.
The COVID-19 pandemic has had a dramatic impact on cancer care, but it has also demonstrated the importance of data and digital solutions to addressing challenges.
Many countries saw partial or complete disruption to their cancer services — and it will be some time before they fully recover.[1]
Healthcare systems around the world rapidly deployed and expanded telemedicine and remote monitoring systems to ensure continuity of care.[2]
The pandemic also accelerated the use of data to reconfigure cancer services, improve patient monitoring and fast-track decisions on regulation, reimbursement and funding.[3]
It is important to recognise that significant barriers still hinder our ability to fully harness the power of data to improve patient care.
The notion of ‘data rich, information poor’ is true for many healthcare systems. Data siloes, a lack of interoperability, unclear actionability of existing data, complex data governance, and limited ability to re-use data for other purposes are all ongoing challenges in many countries.[4] [5] [6]
Moreover, we often fall short in our ability to analyse and extract meaningful insights from the data available to guide decision-making.
All of these challenges must be addressed as a matter of urgency if we are to build sustainable healthcare systems that can continue to improve care for people with cancer.
Pressures on healthcare resources have only increased in the wake of the COVID-19 pandemic.
In this context, optimal efficiency of care must be a core goal of any healthcare system — ensuring resources are being used to deliver the best possible outcomes for patients.
In this context, optimal efficiency of care must be a core goal of any healthcare system — ensuring resources are being used to deliver the best possible outcomes for patients.

Methodology
This report is based on a structured analysis of peer-reviewed and grey literature, 16 expert interviews and consultation with the All.Can Data Working Group and the External Advisory Committee.
The report does not attempt to cover all facets of the complex ecosystem of data in healthcare. For reasons of feasibility, it focuses on data generated during routine clinical care. Data collected in clinical trials are out of scope.
The report and its contents fully respect All.Can’s core principle of being non-promotional and do not include references to any specific products.
A full description of the research methodology is available on the All.Can website: www.all-can.org/what-we-do/ research/data-paper-project/.
Authors
This report has been produced by The Health Policy Partnership and The Health Value Alliance on behalf of All.Can International.
Its creation was led by the All.Can Data Working Group, made up of All.Can International members.
The authors are grateful for the expert advice received from our External Advisory Committee on iterative versions of this report and to contributors who were interviewed for the project.
Disclaimer
All.Can International is a not-for-profit organisation (ASBL) registered in Belgium.
Its work is made possible with financial support from
· Bristol Myers Squibb (main sponsor),
· Roche (major sponsor),
· MSD and
· Johnson & Johnson (sponsors),
· Baxter and
· Illumina (contributors),
with additional non-financial (in kind) support from
· Helpsy,
· The Health Value Alliance and
· Goings-On.
In alignment with its statutes and bylaws, all activities and outputs of All.Can represent consensus of members, who have full editorial control.
In addition to the support provided by the companies listed above,
· Novartis has contributed financially to the development of this policy report.
Table of Contents (TOC)
- Executive summary
- Call to action
- 1. Introduction
- 2. Health data
Defining health data
Use of data and data analytics
Data in cancer care - 3. Defining efficiency in cancer care
Efficiency in cancer care
Efficiency across the cancer care pathway - 4. The role of data in driving efficiency in cancer care
Screening
Diagnosis
Treatment and care
Follow-up and survivorship - 5. Challenges and opportunities
Challenges inherent in data
Challenges with data systems
Challenges embedding data into clinical practice
Challenges in drawing insights from data - 6. Conclusion
- Glossary
- References
About All.Can
All.Can is an international, multi-stakeholder, non-profit organisation aiming to identify ways we can optimise the use of resources in cancer care to improve patient outcomes.
All.Can brings together representatives from patient organisations, policymakers, healthcare professionals, research and industry.
It is made up of All.Can International as well as All.Can national initiatives established in 18 countries (at the time of writing).
All.Can Data Working Group
Sangeeta Agrawal, Helpsy Health
Antonella Cardone, European Cancer Patient Coalition
Ivana Cattaneo, Novartis
Dave Duplay, Vital Options International
Caroline Falciola, F. Hoffmann-La Roche
Alex Filicevas, World Bladder Cancer Patient Coalition; All.Can president
Stefan Gijssels, Digestive Cancers Europe
Petra Hoogendoorn, Goings-On
Agnieszka Krukowska, Johnson & Johnson
Laura McDonald, Bristol Myers Squibb
Jan van Meerbeeck, Antwerp University Hospital
Matthijs Van Meerveld, Merck Sharp & Dohme
Borna Mueller, F. Hoffmann-La Roche
Vivek Muthu, Marivek Consulting
Kathy Oliver, International Brain Tumour Alliance
Titta Rosvall-Puplett, Bristol Myers Squibb
Christobel Saunders, University of Western Australia
Julian Shepelev, Baxter Healthcare
Puneet Singhal, Merck Sharp & Dohme
Henriette Thole, Novartis
Veronica Zilli, Johnson & Johnson
Matthew Hickey, The Health Value Alliance
Shannon Boldon, The Health Policy Partnership
Suzanne Wait, The Health Policy Partnership
External Advisory Committee
Fatima Cardoso, Advanced Breast Cancer Global Alliance
Sybo Dijkstra, Digital Europe
Nigel Hughes, Janssen and European Health Data and Evidence Network
Adrian Jonas, National Institute for Health and Care Excellence
Sabrina Montante, Istituto Superiore di Sanità
Ray Pinto, DigitalEurope
David Roder, University of South Australia
Abdullahi Sheriff, GE Healthcare Europe
Francesco Pignatti, European Medicines Agency (observer role)
Independent contributors
Miriam Gargesi, Illumina
Dipak Kalra, European Institute for Innovation through Health Data
Gregory Katz, University of Paris School of Medicine, PromTime
Steve Laws, Varian Medical Systems
Volker Liebenberg, Illumina
Laura O’Hanlon, Myriad Genetics
References
See the original publication
Originally published at: https://www.all-can.org












