Philips
Shez Partovi
Jun 15, 2022
Key messages
By Joaquim Cardoso MSc.
Institute for Continuous
Health Transformation
to achieve Better Health and Better Care at Lower Cost, for All
June 16, 2022
What is the value of converting data into insights:
- The value of converting data to insights is a point that many informatics leaders agree on. In the 2022 Future Health Index report,
- more than three quarters of informatics experts believe predictive analytics can have a positive impact on the cost of care (78%) and
- overall staff experience (76%), … two of the vital components of the Quadruple Aim.
What is going on?
- Healthcare leaders are investing in AI and predictive solutions to power a shift from data overload to insights at scale.
- Yet along that journey, each organization faces its own specific needs and challenges.
What does it take?
- What does it take to achieve insights at scale, … where insight generation is embedded in the very fabric of your organizational workflow?
- The journey starts with figuring out where your health system sits on the digital maturity curve which refers to a range of global frameworks created by HIMSS to enable healthcare organizations to benchmark and improve their digital transformation progress.
- There are seven frameworks, called maturity models, in areas that include the continuity of care, analytics, diagnostic imaging, and electronic health records (EHRs).
- Each model comprises eight stages that broadly move from no digital infrastructure up to multi-vendor, interconnected, and dynamic capabilities.
What are the Key Success Factors?
- Yet even healthcare leaders who are just embarking on this journey will know that it is fraught with challenges, including difficulties accessing, organizing, and sharing data, as well as concerns over data privacy.
- Overcoming these challenges to move smoothly from data to actionable insights at scale takes four steps:
- 1.INTEROPERABILITY: Invest in interoperability — a fundamental (and very human) enabler
- 2. CLOUD: Power your system of action through the cloud
- 3. PARTNERSHIPS: Prioritize strategic partnerships grounded in clinical expertise
- 4. ACHIEVABLE GOALS: Break your goals down into discrete, achievable, and measurable steps
Conclusion:
- To climb the digital maturity curve to insights at scale, health systems need enterprise-wide strategies that enable end-to-end data integration.
- These strategies must be centered around interoperability, cloud, and strategic collaborations with peers and health technology partners, and be evaluated against appropriate goals.
- Successful informatics leaders take a platform approach, prioritize partnerships with clinical experts, and break down organizational objectives into measurable (and achievable) steps.
- Ultimately, as more healthcare organizations climb higher on the digital maturity curve, the more potential there is for the healthcare industry to unlock clinical and operational benefits across the care continuum for patients, providers, health systems and nations alike.
- Perhaps that’s the biggest insight of all.

In healthcare, no two digital transformations are alike, and this message comes across loud and clear from health informatics leaders.
For example, at HIMSS 2022 conference, we heard from some healthcare leaders
- who have teams of experts applying machine learning to 35 years of healthcare data to generate clinical and operational insights,
- and others who were still grappling with a fragmented IT system that leaves them spending most of their budget just keeping the lights on.
Whatever your transformation journey, the opportunities offered by machine-generated insights are clear.
In my previous post, we explored the difference between data and insights, and how AI and predictive analytics can unlock compounding returns for today’s healthcare organizations to deliver insights at scale — from newfound operational efficiencies, to more accurate clinical decisions, and more effective treatment pathways.
The value of converting data to insights is a point that many informatics leaders agree on.
In our 2022 Future Health Index report, which surveyed nearly 3,000 healthcare leaders across 15 countries,
- more than three quarters of informatics experts believe predictive analytics can have a positive impact on the cost of care (78%) and
- overall staff experience (76%),
… two of the vital components of the Quadruple Aim.
You can read a newly published news center article on informatics insights from the Future Health Index report here.
So, if moving from data to insights is a great way to advance the Quadruple Aim, then …
… what does it take to achieve insights at scale, …
… where insight generation is embedded in the very fabric of your organizational workflow?
The journey starts with figuring out where your health system sits on the digital maturity curve [1], …
which refers to a range of global frameworks created by HIMSS to enable healthcare organizations to benchmark and improve their digital transformation progress.
There are seven frameworks, called maturity models, in areas that include the continuity of care, analytics, diagnostic imaging, and electronic health records (EHRs).
Each model comprises eight stages that broadly move from no digital infrastructure up to multi-vendor, interconnected, and dynamic capabilities.
Yet even healthcare leaders who are just embarking on this journey will know that it is fraught with challenges, including difficulties accessing, organizing, and sharing data, as well as concerns over data privacy.
Overcoming these challenges to move smoothly from data to actionable insights at scale takes four steps:
- 1.Invest in interoperability — a fundamental (and very human) enabler
- 2. Power your system of action through the cloud
- 3. Prioritize strategic partnerships grounded in clinical expertise
- 4. Break your goals down into discrete, achievable, and measurable steps

1. Invest in interoperability — a fundamental (and very human) enabler
Ask five people to define interoperability and you’re likely to get five very different answers.
So, let’s be clear: we will define interoperability here as the ability of software systems to exchange and make use of data.
Though, the The reality today is that healthcare data lives in a huge variety of locations, ranging from isolated server racks to cloud platforms.
The siloed nature of data repositories is widely recognized, with almost two thirds (57%) of informatics leaders surveyed in our 2022 Future Health Index thinking that data silos hinder their ability to use data effectively.
Though, the real power of interoperability is not in the technology itself. It’s in the human benefit it delivers by unlocking insights for patients, providers, and health systems.
Though, the real power of interoperability is not in the technology itself. It’s in the human benefit it delivers by unlocking insights for patients, providers, and health systems.
To realize the potential of insights at scale, data — and the actionable insights it holds — needs to be available in formats that can be shared effortlessly, and above all securely, between points of care, whether within or between hospital systems, to the home, or even on the move.
For example, your hospital department head could integrate operational data from one or more EHRs to generate analytics and real-time workflow intelligence that improve operations effectiveness [2].
To realize the potential of insights at scale, data — and the actionable insights it holds — needs to be available in formats that can be shared effortlessly, and above all securely …
Leveraging open APIs and approved standards like IHE-HL7 can help facilitate data exchange across multiple sources across the continuum of care, so that healthcare providers can deliver the right care at the right time with minimal friction.
In other words, by breaking down siloed data and aggregating that data into actionable patient insights, doors to further innovation can be opened to achieve greater returns, such as improving clinical confidence and patient outcomes — other vital components of the Quadruple Aim.
Leveraging open APIs and approved standards like IHE-HL7 can help facilitate data exchange across multiple sources across the continuum of care, so that healthcare providers can deliver the right care at the right time with minimal friction.
With interoperability in place, the next step is to be able to deploy innovation at scale.

2. Power your system of action through the cloud
At the heart of every advanced insight strategy is a secure cloud-based platform that can serve as an agile toolkit to power your system of action by scaling machine learning quickly and easily throughout your organization and spurring further innovation.
By 2024, research suggests that healthcare providers that have adopted a digital health platform Alongside secure, scalable storage, computing power, and AI toolkits, the cloud also enables dynamic new business models like will outpace competition and partners by 80% in the speed of digital transformation and new feature implementation [3].
Alongside secure, scalable storage, computing power, and AI toolkits, the cloud also enables dynamic new business models like software as a service.
These subscription-based solutions for healthcare providers deliver more predictable, controllable payments and a different level of service upkeep.
Though, the real power of interoperability is not in the technology itself. It’s in the human benefit it delivers by unlocking insights for patients, providers, and health systems.
At Philips, we’ve taken a platform approach to informatics innovation to deliver data-driven actionable insights that advance precision care, support patient-centric, connected care and enable transitions of care.
Our HealthSuite platform combines the core strengths of industry-leading cloud hosting and security, with deep clinical and operational knowledge.
To date, more than 100 types of medical devices have been integrated into HealthSuite, with over 145 billion clinical images securely archived on the cloud platform.
At Philips, we’ve taken a platform approach to informatics innovation to deliver data-driven actionable insights that advance precision care, support patient-centric, connected care and enable transitions of care.

3. Prioritize strategic partnerships grounded in clinical expertise
No care provider is an island.
Organizations need to prioritize partnerships in order to successfully implement digital health technologies and climb the digital maturity curve.
We know from the 2022 Future Health Index report that healthcare leaders are keen to partner with health technology companies — especially those who cover a broad range of areas including strategic vision, specialized healthcare management consulting services, guidance for data analysis, access to innovative technology, and flexible payment models.
No care provider is an island.
Organizations need to prioritize partnerships in order to successfully implement digital health technologies and climb the digital maturity curve.
They’re also keen to learn from each other.
They’re also keen to learn from each other.
For example, late adopters of predictive analytics have expressed a desire to set up ‘mentorships’ with early adopters.
Co-creating with an expert health technology company can enable data scientists, software developers, and clinicians to build a model that fits each provider’s unique needs and help ease the adoption challenges of deploying AI in practice.

4. Break your goals down into discrete, achievable, and measurable steps
For any leader starting out on the journey to insights at scale, the fourth crucial enabler is to begin with discrete, achievable goals in mind.
It’s vital to measure the impact of your insights too
For any leader starting out on the journey to insights at scale, the fourth crucial enabler is to begin with discrete, achievable goals in mind.
It’s vital to measure the impact of your insights too.
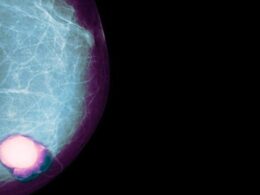
Let’s take another example in imaging, where health systems in many countries face a shortage of radiology technicians.
As we discussed in my previous blogpost, a good place to start is operational forecasting.
For example, a Chief Nursing Officer (CNO) not only wants to know exactly what staffing levels are like today, but more importantly they want to know what staffing needs will be — say — tomorrow, or next weekend.
This kind of care traffic control system can help a CNO predict potential patient care bottlenecks in a hospital, and anticipate patient flow capacity and match resources and staffing to patient care needs.
It’s vital to measure the impact of your insights too.
Let’s take another example in imaging, where health systems in many countries face a shortage of radiology technicians.
Vendor-agnostic imaging solutions can enable technicians in a central command center to seamlessly connect with technologists at scan locations across their organization and support them to ensure optimal patient imaging, reducing cost of recalls, and improving patient satisfaction.
One such implementation in the US has enabled one health system to increase its imaging staff capacity and retain more than $350K of MRI procedure revenue that would have otherwise been lost to another provider or deferred [4], together with a saving in personnel travel cost of over $60K per year [5].

Climbing the curve together
To climb the digital maturity curve to insights at scale, health systems need enterprise-wide strategies that enable end-to-end data integration.
These strategies must be centered around interoperability, cloud, and strategic collaborations with peers and health technology partners, and be evaluated against appropriate goals.
Ultimately, as more healthcare organizations climb higher on the digital maturity curve, the more potential there is for the healthcare industry to unlock clinical and operational benefits across the care continuum for patients, providers, health systems and nations alike.
Perhaps that’s the biggest insight of all.
About the author
Shez Partovi
Chief Medical, Innovation & Strategy Officer, Royal Philips
Shez Partovi obtained his medical degree from the McGill University, in Montreal, Canada and completed his neuroradiology subspecialty at Barrow Neurological Institute in Phoenix, AZ. He is a serial entrepreneur and has launched several health IT companies, including 2 on telehealth.
Originally published at https://www.philips.com.