NIH Director´s blog (National Institutes of Health
Posted on November 9th, 2021
by Dr. Francis Collins
This is an article based on the blog of Dr. Collins, and complemented by the excerpt of the original publication, edited by the Editor of The Health Strategist blog, by Joaquim Cardoso MSc.
Infographic / Selected Image (from the paper), by the Editor of the blog:
Descriptive analysis
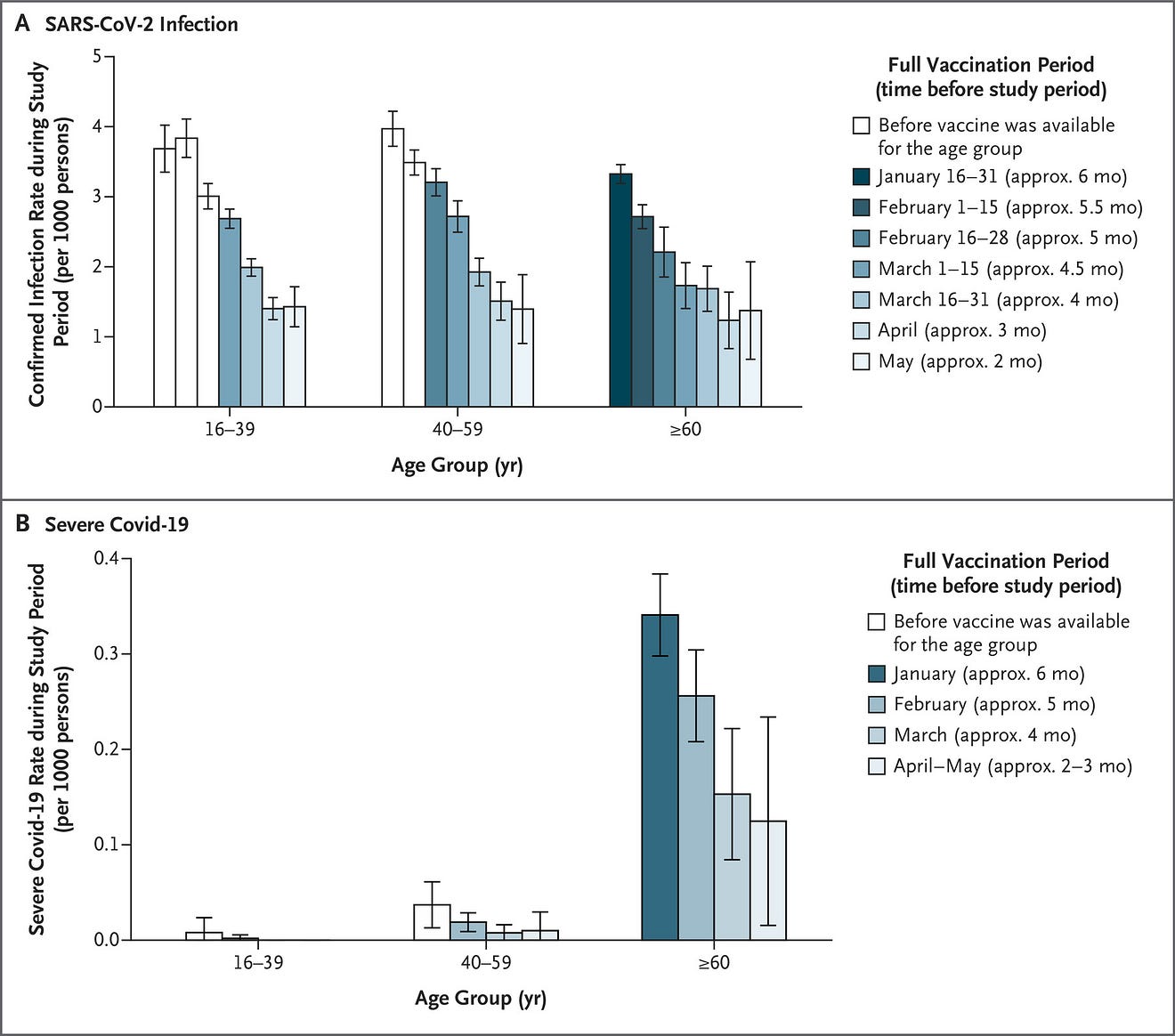
The rate of confirmed SARS-CoV-2 infection showed a clear increase as a function of time from vaccination.
- Among persons 60 years of age or older who were fully vaccinated in the second half of January,
– the rate was 3.3 confirmed infections per 1000 persons during the study period,
– as compared with 2.2 confirmed infections per 1000 persons who became fully vaccinated in the second half of February
– and 1.7 confirmed infections per 1000 persons fully vaccinated in the second half of March (Figure 3A).
- Similar results were observed in the other age groups and when the analysis was categorized according to age in decades (Figure 3A and S1).
- However, primarily health care workers and severely immunocompromised adults became fully vaccinated during the first three vaccination periods (January 16 to February 28) in the 16–39-year-old group and during the first two vaccination periods (January 16 to February 15) in the 40–59-year-old group; thus, the results for those vaccination periods in these age groups may be biased owing to selective samples and should be interpreted with caution.
A similar pattern was observed in the analysis of severe Covid-19 in the group of persons 60 years of age or older (Figure 3B).
- In this analysis, vaccination periods were defined as January, February, March, and the combined April–May period because of the small numbers of severe cases in each age group.
- The rate of severe Covid-19 among persons 60 years of age or older who were fully vaccinated in January was
– 0.34 cases per 1000 persons over the study period and decreased
– to 0.26 cases per 1000 persons among those who were fully vaccinated in February,
– 0.15 cases per 1000 persons fully vaccinated in March, and
– 0.12 cases per 1000 persons fully vaccinated in the April–May period.
- The numbers of severe cases in the younger age groups were too small for conclusions to be drawn.
ARTICLE (By Dr Collins)
The winter holidays are approaching, and among the many things to be grateful for this year is that nearly 200 million Americans are fully vaccinated for COVID-19.
That will make it safer to spend time with friends and family, though everyone should remain vigilant just to be on the safe side.
Though relatively uncommon, breakthrough infections are possible. That’s why the Centers for Disease Control and Prevention (CDC) recommends booster shots for several at-risk groups, including folks 65 years and older, those with underlying medical conditions, and people whose occupations place them at high risk of exposure.
One of the main studies providing the evidence for CDC’s recommendation was recently published in the New England Journal of Medicine [1].
It found that vaccine-induced immunity, while still quite protective against infection and severe illness from COVID-19, can wane after several months.
The study is yet another highly informative report from Israel, where public health officials launched a particularly vigorous national vaccination campaign in December 2020.
More than half of adult Israelis received two doses of the Pfizer vaccine within the first three months of the campaign.
By May 2021, Israel had extremely small numbers of confirmed COVID-19 cases-just a few dozen per day.
But the numbers crept back up in June 2021. The rise also included a substantial number of breakthrough infections in vaccinated individuals. The vast majority of those cases in June-98 percent-were caused by the emerging Delta variant.
Researchers led by Yair Goldberg, Technion-Israel Institute of Technology, Haifa, wondered whether this resurgence of COVID-19 could be fully explained by the rise of the more infectious Delta variant.
Or, they wondered, did the waning of immunity over time also play a role?
To find out, the researchers looked to over 4.7 million fully vaccinated Israeli adults, more than 13,000 of whom had breakthrough infections from July 11 to 31, 2021 with SARS-CoV-2.
The researchers looked for an association between the rate of confirmed infections and the time that had passed since vaccination.
Without any significant waning of immunity, one shouldn’t see any difference in infection rates among people who were fully vaccinated at the earliest opportunity versus those vaccinated later.
The results were clear: the rate of confirmed COVID-19 infection revealed a slow but steady waning of immunity over time.
- Among individuals 60 years or older who were fully vaccinated last January, the number of confirmed breakthrough infections was 3.3 per 1,000 people during the three weeks of the study.
- Those who were vaccinated in February and March had lower infection rates of 2.2 per 1,000 and 1.7 per 1,000, respectively.
- The data revealed a similar pattern in those aged 40 to 59 and those aged 16 to 39.
An important question is whether these breakthrough infections were serious enough to require hospitalization.
While such cases were much less common, more than 400 of those with confirmed COVID-19 breakthroughs went on to develop severe illness.
And, again, the data show a similar pattern of waning immunity.
The rate of severe COVID-19 among adults 60 years of age or older who were fully vaccinated in January was 0.34 cases per 1,000 persons.
The rate of severe illness dropped to 0.26 cases per 1,000 among those vaccinated in February and 0.15 cases per 1,000 for those vaccinated in March.
The researchers report that the number of severe COVID-19 cases among the younger fully vaccinated groups were too small to draw any conclusions.
While the Delta variant surely has played a role in the resurgence of COVID-19 in recent months, these findings suggest that waning immunity also is an important factor.
Understanding these dynamics is essential for making critical policy decisions. In fact, these data were a key factor in the decision by the Israeli Ministry of Health in July 2021 to approve administration of COVID-19 booster shots for individuals who’d been vaccinated at least 5 months before.
Back in the U.S., if you were among those who got your vaccine on the early side-good for you.
If it’s been more than six months since your original shots, and if you are in one of the risk groups, you should consider a COVID-19 booster shot to remain optimally protected in the months ahead.
I’ll be getting my Moderna booster this week.
While you’re at it, consider getting your annual flu shot taken care of, too. The CDC guidelines state that it’s perfectly OK to get your COVID-19 and flu shots at the same time.
Originally published at https://directorsblog.nih.gov on November 9, 2021.
REFERENCE(S)
_________________________________________________________
[1] Waning immunity after the BNT162b2 vaccine in Israel. Goldberg Y, Mandel M, Bar-On YM, Bodenheimer O, Freedman L, Haas EJ, Milo R, Alroy-Preis S, Ash N, Huppert A. N Engl J Med. 2021 Oct 27.
Waning Immunity after the BNT162b2 Vaccine in Israel
October 27, 2021
List of authors.
- Yair Goldberg, Ph.D.,
- Micha Mandel, Ph.D.,
- Yinon M. Bar-On, M.Sc.,
Omri Bodenheimer, M.Sc., - Laurence Freedman, Ph.D.,
- Eric J. Haas, M.D.,
- Ron Milo, Ph.D.,
- Sharon Alroy-Preis, M.D.,
- Nachman Ash, M.D.,
- and Amit Huppert, Ph.D.
Abstract
BACKGROUND
In December 2020, Israel began a mass vaccination campaign against coronavirus disease 2019 (Covid-19) by administering the BNT162b2 vaccine, which led to a sharp curtailing of the outbreak. After a period with almost no cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, a resurgent Covid-19 outbreak began in mid-June 2021. Possible reasons for the resurgence were reduced vaccine effectiveness against the delta (B.1.617.2) variant and waning immunity. The extent of waning immunity of the vaccine against the delta variant in Israel is unclear.
METHODS
We used data on confirmed infection and severe disease collected from an Israeli national database for the period of July 11 to 31, 2021, for all Israeli residents who had been fully vaccinated before June 2021. We used a Poisson regression model to compare rates of confirmed SARS-CoV-2 infection and severe Covid-19 among persons vaccinated during different time periods, with stratification according to age group and with adjustment for possible confounding factors.
RESULTS
Among persons 60 years of age or older, the rate of infection in the July 11–31 period was higher among persons who became fully vaccinated in January 2021 (when they were first eligible) than among those fully vaccinated 2 months later, in March (rate ratio, 1.6; 95% confidence interval [CI], 1.3 to 2.0). Among persons 40 to 59 years of age, the rate ratio for infection among those fully vaccinated in February (when they were first eligible), as compared with 2 months later, in April, was 1.7 (95% CI, 1.4 to 2.1). Among persons 16 to 39 years of age, the rate ratio for infection among those fully vaccinated in March (when they were first eligible), as compared with 2 months later, in May, was 1.6 (95% CI, 1.3 to 2.0). The rate ratio for severe disease among persons fully vaccinated in the month when they were first eligible, as compared with those fully vaccinated in March, was 1.8 (95% CI, 1.1 to 2.9) among persons 60 years of age or older and 2.2 (95% CI, 0.6 to 7.7) among those 40 to 59 years of age; owing to small numbers, the rate ratio could not be calculated among persons 16 to 39 years of age.
CONCLUSIONS
These findings indicate that immunity against the delta variant of SARS-CoV-2 waned in all age groups a few months after receipt of the second dose of vaccine.
EXCERPTS FROM THE ORIGINAL PUBLICATION
Introduction
Key to the containment of the coronavirus disease 2019 (Covid-19) pandemic is mass vaccination of the population. However, the success of this policy is challenged by breakthrough infection and disease in fully vaccinated persons. One potential cause of breakthrough infection is the emergence of new variants of concern1 that escape immunity, thus reducing the effectiveness of the vaccine. Several studies investigating the effectiveness of the BNT162b2 vaccine (Pfizer–BioNTech) against the beta (B.1.351)2,3 and delta (B.1.617.2)4–6 variants showed only modest rates of breakthrough infection and disease, whereas other studies showed higher rates.7,8
A second potential cause of breakthrough infection is waning of the immunity conferred by the vaccine. Mass vaccination with the BNT162b2 vaccine began in December 2020, and little is known about waning immunity over time. A recent study on longer-term follow-up of the participants in the phase 2–3 randomized trial of the BNT162b2 vaccine9 showed a reduction in vaccine efficacy from 96% (in the period of 7 days to <2 months after receipt of the second dose) to 84% (in the period of 4 months to approximately 7 months after receipt of the second dose), which indicated a decrease in protection by a factor of four (i.e., [100−84]÷[100−96]). Preliminary reports of waning effectiveness of the same vaccine have come from a health maintenance organization in Israel10 and from the United States,11 and a decrease in vaccine-induced neutralization titers during the first 6 months after receipt of the second dose of vaccine has been reported.12
Israel conducted a very successful vaccination campaign using the BNT162b2 vaccine.13–15 Starting in December 2020, more than half the adult population received two doses of vaccine within 3 months. The vaccination campaign, together with social measures, led to a sharp curtailing of the outbreak. By May 2021, infection rates had decreased to a few dozen cases daily, most of which were in unvaccinated persons or in persons returning from abroad. However, the number of polymerase-chain-reaction (PCR) tests that were positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) started to rise exponentially in June 2021, with a substantial number of infections being reported in vaccinated persons (Figure 1). This rise in community transmission was followed by a concomitant increase in the numbers of severe cases and deaths, in both the vaccinated and unvaccinated populations. Genetic analysis showed that as of June 2021, more than 98% of the positive cases in Israel were attributed to the delta variant.16 In this study, we estimated the role of waning immunity in the observed breakthrough against the delta variant.
Methods
See the original publication
Results
See the original publication
Discussion
The centralized health care system in Israel succeeded in vaccinating most of the Israeli population relatively early and in a short time.13–15
This population is, therefore, useful for studying the effects of the BNT162b2 vaccine on the spread of SARS-CoV-2 infection and severity of Covid-19, as well as for studying the waning of vaccine protection over time.
The appearance and rapid predominance of the delta variant in June 2021 resulted in a dramatic increase in the number of new SARS-CoV-2 infections among fully vaccinated persons, which aroused concern regarding decreased efficacy of the vaccine over time (Figure 1).
A comparison of the rate of confirmed infection among persons vaccinated at different times revealed a clear increase in the rate as the time from vaccination increased in all age groups, with and without correction for measured confounding factors (Figure 3A and Table 2). The rate of confirmed infection among persons 60 years of age or older who became fully vaccinated in the second half of January was 1.6 times as high as that among persons in the same age group who became fully vaccinated in March. The data show a similar increase in rate with increasing time since vaccination in the other age groups. The rate of severe Covid-19 cases also increased as a function of time from vaccination. Serologic studies in Israel have shown a correlated time-dependent reduction in neutralization titers,12,20 which might be the biologic mechanism governing the observed waning immunity, and thus support the finding in this population-based research.
In contrast to early findings from the United Kingdom,5 approximately two thirds of the cases of severe Covid-19 in Israel during the study period occurred in persons who had received two doses of the BNT162b2 vaccine.
Two major differences exist between the studies.
- First, the current analysis used data from July 2021, a time when, for most of the Israeli population, at least 5 months had passed since receipt of their second dose of vaccine.
The U.K. data were collected during the period of April through June 2021, with a much shorter time from vaccination to infection. - Second, Israel has followed the original Pfizer–BioNTech protocol of administering the second dose 3 weeks (21 days) after the initial injection in most recipients, whereas the time between doses in the United Kingdom has typically been longer.6
A comparison of vaccinated persons with unvaccinated persons is of interest in order to predict the future burden on the health system.
We therefore obtained data on the entire Israeli population from the Israeli Central Bureau of Statistics and calculated the number of unvaccinated persons indirectly. Moreover, unvaccinated persons might differ from the vaccinated population in important characteristics that could result in biased estimates. Nevertheless, we estimated the effectiveness of the vaccine against confirmed SARS-CoV-2 infection (see Supplementary Analysis 1). Vaccinated persons were found to be protected even after 6 months, as compared with unvaccinated persons. However, vaccine effectiveness was considerably lower than it had been closer to the vaccination date. Our findings are in line with findings from the randomized trial of the BNT162b2 vaccine, which showed a reduction in vaccine efficacy against symptomatic infection from 96% in the first 2 months after vaccination to 84% at 4 to 7 months after vaccination, when averaged over all age groups combined.9
Observational studies are subject to confounding bias and detection bias.
We examined these biases by using different sensitivity analyses (see Supplementary Analysis 2) and obtained similar results. Nevertheless, some sources of bias might remain; for instance, any effects that were due to differences in coexisting conditions between the vaccination periods could not be controlled for, because coexisting conditions are not recorded in the national database.
We did not separate the contribution of vaccine breakthrough due to waning immunity from the contribution due to the change in the dominant variant from alpha (B.1.1.7) to delta.
Our analysis showed only the clear effect of waning vaccine-induced immunity against the delta variant. In addition, we were not able to quantify the extent of waning in the months immediately after vaccination (when the prevalence was extremely low in Israel).
Understanding the extent of waning immunity is critical for policy making, especially regarding vaccination strategies.
The results presented here provided an epidemiologic basis for the decision by the Israeli Ministry of Health on July 30, 2021, to approve the administration of a booster (third dose) of Covid-19 vaccine to persons who had been vaccinated at least 5 months previously.
The findings also suggest the need to follow the effects of waning immunity closely and to inform policymakers worldwide who are facing decisions regarding the administration of booster vaccinations.
Authors affiliations
From Technion–Israel Institute of Technology, Haifa (Y.G.), the Hebrew University of Jerusalem (M.M.),
and the Israeli Ministry of Health (O.B., E.J.H., S.A.-P., N.A.), Jerusalem,
the Weizmann Institute of Science, Rehovot (Y.M.B.-O., R.M.),
the Gertner Institute for Epidemiology and Health Policy Research,
Sheba Medical Center Tel Hashomer,
Ramat Gan (L.F., A.H.),
Tel Aviv University, Tel Aviv (A.H.),
and Ben Gurion University, Beersheva (E.J.H.) — all in Israel.
Originally published at https://www.nejm.org












