Mayo Clinic Proceedings
Victor F. Trastek, MD; Neil W. Hamilton, JD; Emily E. Niles, BS, JD;
February 03, 2014
Credit to the image: 5dvision
Abstract
Our current health care system is broken and unsustainable.
- Patients desire the highest quality care, and it needs to cost less.
- To regain public trust, the health care system must change and adapt to the current needs of patients.
- The diverse group of stakeholders in the health care system creates challenges for improving the value of care.
- Health care providers are in the best position to determine effective ways of improving the value of care.
- To create change, health care providers must learn how to effectively lead patients, those within health care organizations, and other stakeholders.
This article presents servant leadership as the best model for health care organizations because it focuses on the strength of the team, developing trust and serving the needs of patients.
As servant leaders, health care providers may be best equipped to make changes in the organization and in the provider-patient relationship to improve the value of care for patients.
Key Messages (from Conclusion):
The challenges facing health care require strong leadership.
The model of leadership will vary depending on the situation, and in reality a leader may exhibit a blend of leadership models.
The purpose of leadership is to work with others to improve the situation.
Because health care is about people caring for others and there should be alignment with how we treat patients and how we work together as staff, servant leadership may be considered a dominant model.
Servant leadership is best aligned with the professional and ethical duties of health care providers in delivering the high-value care patients deserve.
Servant leadership focuses on trust and empowerment in both the patient relationship and the health care provider team relationships.
The challenges faced by the health care system extend beyond the clinical setting. Servant leadership can also stimulate necessary change so that all health care stakeholders focus on serving others: their patients and their staff.
By aligning health care stakeholders to serve patients and each other, a more sustainable health care system providing an improved value equation of high-quality care and lower cost is possible.
FULL VERSION
Our current health care system is broken and unsustainable. This article provides a leadership-focused solution to address this challenge. The first section defines the health care system stakeholders and then discusses the complex challenges of creating a more effective health care system that improves the value of care for patients by both increasing the quality of care and lowering its cost. The second section analyzes how health care providers can provide the crucial leadership to achieve these goals. In a trusting partnership with their patients, health care providers understand patient needs and available care; however, as the third section explains, the providers need leadership education and development to undertake their leadership roles. The fourth section identifies servant leadership as the best model for health care organizations and providers because it focuses on trust and empowerment in both patient relationships (so that patients can make health decisions in their best interests) and health care provider team relationships that deliver their care.
Challenges Faced by Health Care Providers and Organizations
- Competing Interests of health care System Stakeholders
- Dimension of the Challenges
- Improving Quality and Lowering Cost to Increase Value
Competing Interests of health care System Stakeholders
The health care system has a wide range of stakeholders including patients; health care providers; health care organizations; federal, state, and local governments; health insurance companies; business employers; health care-related businesses; and academia. The separate interests of these stakeholders frequently clash. The primary stakeholders are patients. The main goal of patients is to remain healthy by using the services offered by the health care system. Patients seek health care providers they can trust for preventive care and safe and effective medical advice and treatment. Patients can feel vulnerable as they place their lives in the hands of the health care system in times of desperate need. Interaction with the health care system affects patients’ physical, emotional, and financial well-being.
Health care providers are the stakeholders driving the health care system through their interaction with patients. This group includes doctors, nurses, administrators, and allied health staff (ie, physical therapists, laboratory technicians, and respiratory therapists). Health care providers seek a safe and organized environment to serve patients effectively. They dedicate their working lives toward helping others to be healthy and overcome medical challenges. This desire to serve others is at the heart of the health care providers’ motivation.
Health care organizations are a large group of stakeholders made of hospitals, clinics, outpatient operation centers, and other care sites, including the management and staff of these institutions. The main interest of the health care organization is to provide health care services to the regional community. Not-for-profit health care organizations focus on using available funds efficiently to provide care to patients. For-profit health care organizations may focus more on promoting the business interests of the organization.
Federal, state, and local governments are stakeholders in the health care system through their concern for citizens’ well-being, payment of health care costs and government employee health care benefits, and their financial and legislative effect on the system. To ensure effectiveness and safety for its citizens, the government monitors and regulates pharmaceuticals, medical devices, and provider practices. In 2011, the federal government spent $769 billion on 3 health insurance programs — Medicaid, Medicare, and Children’s Health Insurance Program — accounting for 21% of the 2011 federal budget.1
In addition, in 2010, the US Census Bureau data indicated that 49.9 million Americans were uninsured. Federal and state governments provide subsidized health insurance for residents who cannot pay on their own. With the new Affordable Care Act, subsidized health care will increase markedly. Local governments provide health services through county hospitals and local health initiatives. All levels of government expend substantial resources to provide health care insurance for their employees. With the health of its citizens and so much money at stake, our government has a strong interest in lowering costs and ensuring that citizens receive high-quality care through preventive care and efficient treatments for disease.
At the core of the health care system lies the patient’s desire to be physically, emotionally, and financially sound. Conflicts among stakeholders emerge over the best way to reach those goals. Government can clash with health insurance companies over the legally required terms in their policies and with businesses over the safety of medical drugs and products. The regulation of health care practices by the government through its health insurance programs, such as Medicaid, Medicare, and Children’s Health Insurance Program, creates conflict with health care providers trying to give patients the best care while conforming to regulations and limited payment structures. Health insurance companies clash with health care providers and their customers over the cost and value of services. Health care providers and those in academia debate the effectiveness of medical practices and treatments in the real world vs laboratory research settings. Health care providers and patients may disagree over the treatments in the patient’s best interest, the quality of care the patient receives, and the price of services. Patients often discover unexpected financial consequences to medical treatments despite insurance coverage.
Conflicts among various stakeholders may spur the positive outcome of critical examination of the interfaces among them; however, this problem solving has yet to occur on a wide scale and a greater examination of the issues between stakeholders will be necessary to reorganize a currently unsustainable health care system.
Dimension of the Challenges
Let us examine the cost and the quality of care, components that make up the value equation for health care. Health care providers must address the issue of quality of care: the need for better and safer outcomes and higher patient satisfaction. The goal of the entire health care system is to cure disease and improve patient health. Poor outcomes and low patient satisfaction may decrease a patient’s perceived value of the medical care provided. Each interaction with a health care provider affects the patient’s perception of the quality of care, affecting patient trust and adherence to treatments and consequently the cost of care. Health care providers and organizations must focus on increasing value by providing more effective and safer treatments while increasing patient satisfaction to remain trusted partners. The cost of health care is predicted to increase by 7.5% in 2013, a rate 3 times higher than the inflation rate. 2 2012 was “the first year the average cost of healthcare for the typical American family of four surpassed $20,000.”3 The proportion of household income devoted to health care costs is increasing considerably and causing families to make tough financial decisions. 4
These costs impose a great burden on patients (insured or uninsured), businesses, and the government. Innovations in medication and technology provide newer more efficient lifesaving tools, but they may simultaneously increase costs.5
The cost of health care services greatly affects the value of care; lowering the cost is a critically important challenge that health care providers and organizations must confront.
Improving Quality and Lowering Cost to Increase Value
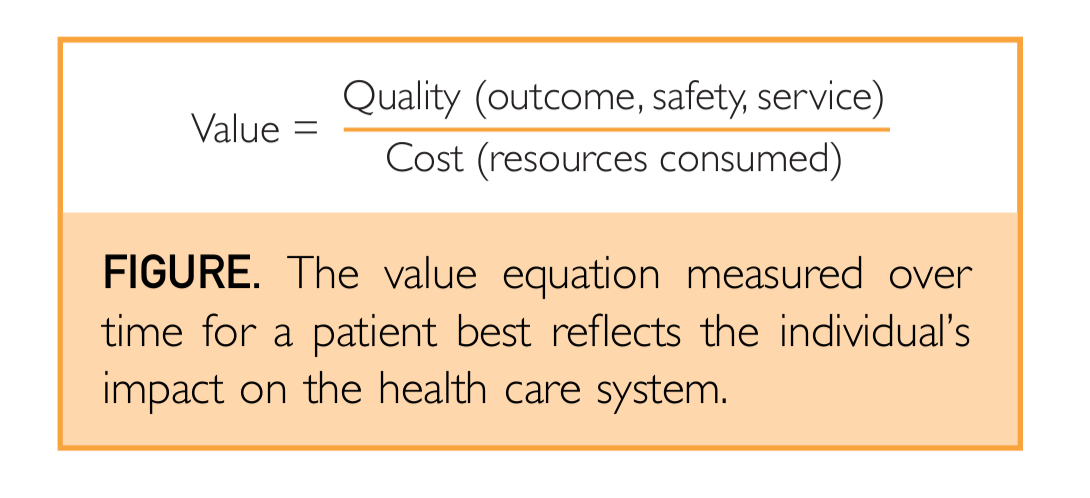
The main challenge for health care providers is to improve the overall value of health care. Value can be measured through an equation comparing quality to the cost of the service provided (Figure). Quality includes the outcomes, safety, and service because it relates to an episode of care. The cost of health care equals the amount of resources used not only for an episode of care but also over the entire time of treatment. Resources used or costs will include health care provider time, diagnostics, therapeutics, and the use of a facility. 6
Restoring sustainability to the health care system requires health care providers to increase the value of health care services by improving outcomes, safety, and service while lowering costs. 6
Figure: The value equation measured over time for a patient best reflects the individual’s impact on the health care system.
Building trust between health care providers and patients has the potential to increase the value equation in health care.
- Increased trust will improve the ability of stakeholders to collaborate in their efforts to increase quality and lower costs.
The primary relationship in health care is between health care providers and patients. A patient must be able to trust that doctors, nurses, and other allied health staff are competent and knowledgeable and have the patient’s best interest at heart. A high degree of professionalism among health care providers builds trustworthiness with the patient. In addition, trust between the health care provider and the patient enables honest communication and may increase the likelihood that a patient will follow through on treatment, leading to a better outcome and lower long-term costs. 7
- Trust is also an important component of teamwork.
Effective teams communicate more clearly among themselves and with the patient, delivering a better outcome, safer experience, and a higher level of service at a more efficient cost.
Health care administrators as an integral part of the team must trust the providers to deliver excellent value, whereas health care providers must trust the administrators to support their work through effective clinic organization, policies, and management.
Building trusting relationships across stakeholders can create synergy and increase the value equation.
Changes in Health Care Necessitate Leadership
As discussed previously, the diverging purposes and goals of the various stakeholders increase the complexity of the issues that confront the health care system.
Making effective and lasting changes to increase quality of care and lower costs and thus improve value requires leadership.
Of all the stakeholders, health care providers should be at the forefront as leaders because of their unique understanding of and interaction with the patient.
- Health care providers can improve patient outcomes by encouraging patient adherence to therapy.
- They can also decrease patient costs by avoiding unnecessary tests, procedures, and medications.
- Health care providers can identify gaps in technology and medical procedures to lead change that increases the value of health care.
- Last and most importantly, health care providers should always be aligned with the best interests of the patient.
Although the constant and rapid changes in the current health care landscape may be putting pressure on this bedrock concept of health care, it remains the primary value of the entire profession.
As hands-on service professionals, health care providers are capable of effecting change in health care delivery.
Health care providers serve as leaders in their relationship with patients.
- Patients seek their leadership for diagnosis, assessment, advice, and treatment.
- Health care providers lead patients by educating and delivering appropriate care, enabling patients to make well-informed decisions that the patient determines are in his or her best interest.
Trust is an essential component in the relationship between health care providers and patients.
- That relationship is caring, intimate, and crucial for the patient’s well-being, the health care experience, and can improve the value equation in health care.
In addition, health care providers must assume a leadership role beyond their relationship with patients. Teams are integral to health care delivery.
- A health care provider working as a leader will nurture the development of his or her fellow health care providers and ensure professional, ethical, and value-driven standards.
- A strong leader enables teams to function safely and efficiently and keeps the best interests of patients an utmost priority.
Health care providers must also serve as leaders within health care organizations.
- Strong relationships between health care providers and health care organizations can facilitate changes to improve the value of care for patients.
- By assuming a leadership role, health care providers can guide the health care system to improve not only value but sustainability as well.
Leadership is equally important within the health care provider network of peers.
- Health care providers rely on their professional peers to relay important scientific and health care delivery developments.
- Within the group, individuals can serve as leaders through their commitment to professional and ethical behavior.
- This kind of leadership is valuable within a single health care organization, regionally among professional peers, and even nationally, because they have the opportunity to share their work.
Health Care Providers Need Leadership Education and Development
Health care providers need leadership education and development to implement effective change.
There are many different leadership models that define effective leadership, describe leadership behavior, and suggest paths of leadership development.
Some models may work best in particular situations and be less useful in others. Health care providers need the opportunity and the resources to identify the models that best fit the health care industry and to develop effective leadership skills.
Although there is now a trend to obtain a Master of Business Administration degree, most physicians with a Doctor of Medicine degree acquire leadership training on the job or from individual courses in leadership and management from organizations such as the American College of Physician Executives, Harvard, Stanford, and Wharton.
A 2011 review of 26 studies on student attitudes found that “medical students perceive a need for leadership and management education.”8
Some medical schools are seeking to expand leadership development opportunities through dual-degree programs such as the Creighton University School of Medicine Program for Leadership Development and Boonshoft School of Medicine’s Physician Leadership Development Program.
Mayo Clinic in Arizona has proposed a simultaneous master’s degree in Science of Health Care Delivery in collaboration with Arizona State University. All these are important steps toward building leadership development programs for health care providers.
Leadership skills are not learned over the course of a day, a week, or even a semester. Rather, leadership develops over the course of an individual’s career and lifetime.
Leadership opportunities could be explored at the undergraduate level. Medical schools, nursing programs, and other health care educators should enable students to pursue leadership development through programs tailored to their professional needs and integrated when possible to promote team learning.
A current example is the plan to offer modules of the master’s degree in the Science of Health Care Delivery from Arizona State University to medical students and other trainees in health care.
This plan adds to the learning experience by instilling skills and tools to improve value and to better deliver care.
Leadership development should continue throughout their working careers. These opportunities must be in line with current research on the best methods for leadership development.
Because leadership development is an ongoing process, health care institutions must provide resources, opportunities, and encouragement for health care providers to develop and grow as leaders.
A 2006 qualitative study on leadership development in health care found that there was a perception within health care that health care leadership development lagged 10 to 15 years behind leadership development in other industries.9
… there was a perception within health care that health care leadership development lagged 10 to 15 years behind leadership development in other industries.9
Several factors account for this lag.
- The study identified conflict within organizations on the best practices for leadership development and the lack of a specific model of leadership for health care.
- Health care providers are also disinclined to participate because of time constraints, interference with their clinical workload, and decreased productivity from lost patient visits.
- Financial constraints on health care organizations have put leadership development on the back burner.
The attitudes and challenges described indicate the need for greater rather than less commitment to leadership development throughout the health care system.
The attitudes and challenges described indicate the need for greater rather than less commitment to leadership development throughout the health care system.
The commitment to develop health care leaders must come from both health care organizations and individual health care providers.
Providers need to take control of their leadership development.
When people “feel a sense of autonomy over their environment,” they are more motivated to change and grow.10
By taking personal responsibility for their growth, health care providers will be motivated to demand leadership development opportunities from their employers and seek opportunities for their personal growth.
Building a system of leadership development throughout the health care system that spans early training to end of career will be an ongoing process. Research will reveal the effectiveness of leadership models and leadership development practices.
Alignment of Leadership Models to the Health Care Industry
Health care providers can assume many leadership roles as a part of their professional responsibilities.
A summary of 4 leadership models that have been used in the health care industry is given in the subsections that follow. An examination of their goals and strategies can help identify a model that can best lead to the reforms necessary to achieve the primary goal of increasing value by improving care and lowering costs.
- Transactional Leadership
- Adaptive Leadership
- Transformational Leadership
- Servant Leadership
It is important to state that there are many components of leadership that are critical to success including integrity and professionalism, setting vision, strategy, operating tactics and aligning resources, inspiring others, and, most importantly, execution — actually moving the ball in a positive direction. A particular model of leadership implicitly includes all these components but may promote different ways in how execution of the plan is accomplished.
Transactional Leadership
Transactional leadership is a model based on systems of reinforcement and punishment. This model has been considered the most prevalent leadership model used in health care.11
Transactional leaders set goals and performance standards for their employees and in return promise to provide rewards (usually monetary) if those standards are met. An employee who does not meet standards may face discipline or punishment. The model relies on extrinsically motivating the employee to work for his or her personal interest.
Many health care providers enter their profession because they primarily want to help people. The intrinsic motivation to improve the lives of others by providing excellent care conflicts with transactional leadership. In a transactional leadership model, the employee’s “personal interests” are the sole motivating factor for gaining a specified performance. In doing so, the employee’s performance may be undermined, especially in employees with “high initial levels of intrinsic motivation.”12
Because of this conflict, an employee’s performance may suffer, leading to negative outcomes for the organization and ultimately lack of employment.12
The transactional leadership model is unable to account for the complex motivations of health care providers and the professional and ethical duties to their patients. Transactional leadership fails to build trust between the leader and the follower, an essential part of the health care provider-patient relationship. This model does not require a leader to take the ethical and moral road and to provide high-value care to the patient. In health care, leadership must take the ethical considerations of a patient’s life into account.
Adaptive Leadership
Adaptive leadership is used to enable a group to overcome challenges created by change. Adaptive challenges occur when core beliefs and values lead to failures or when a competing value becomes more relevant.13
Difficulties executing teamwork and complex systematic problems resulting from industry changes are typical adaptive challenges for organizations. An adaptive leader identifies adaptive challenges and confronts difficult realities of the situation and old values or beliefs contributing to the adaptive challenge. The leader helps to regulate the distress of the group and facilitates collaborative efforts to create solutions. A solution to an adaptive challenge often involves new values, behaviors, relationships, roles, and approaches to work.13,14
An adaptive leader is not focused on providing technical solutions to problems, but rather seeks to effect change through a process of individual and group reflection and collaboration.14
Health care providers have been encouraged to use the adaptive leadership model in the clinical, research, and health care policy settings.14
Patients frequently face adaptive challenges when confronting a high-risk illness. Through adaptive leadership, a health care provider enables patients to effect lifesaving changes by confronting them with the reality of their medical condition and the effects of failure to overcome their adaptive challenge; however, adaptive challenges can create a high level of distress for those involved; patients in a fragile medical condition or with emotional sensitivity may not be well served by a blunt confrontation. Such interaction could harm trust in the health care provider-patient relationship.
Teamwork in the health care setting can require more technical solutions and decisive actions than adaptive leadership allows. In an emergency situation, a direct chain of command serves to create the organization that sudden chaos demands. Although all group members certainly help to overcome obstacles in these setting, there is likely not enough time for wide group collaboration and conversation to address a dire situation.
Despite the potential risks of applying adaptive leadership, the practice of collaborative problem solving and honest confrontation could promote innovation and effective changes at various levels of the health care system; however, adaptive leadership may not match the ethical requirements of health care service. Adaptive leadership fails to provide an explicit requirement that change and action to overcome an adaptive challenge must take into account moral and ethical aspects of human life.
Transformational Leadership
Transformational leaders work to inspire their followers to look past their own self-interest and to perform above expectations to promote team and organizational interests. The transformational leader’s vision and values are central to the mission of the group. The leader believes deeply in the vision and values central to the group’s purpose. To gain the participation of followers, a transformational leader must advocate for his or her vision and persuade followers to adopt it. 15
Transformational leadership includes 4 factors: idealized influence, inspirational motivation, intellectual stimulation, and idealized consideration. Idealized influence refers to the charismatic nature of the transformational leader that causes followers to believe that the leader is passionate about the cause and worthy of the followers’ attention. Inspirational motivation refers to the leader’s ability to articulately persuade and inspire others to join in the mission. Through intellectual stimulation, the transformational leader challenges others to fully embrace the mission and to give up old values in competition with the new mission. The leader also inspires them to create innovative solutions and ways to carry out the mission. A transformational leader addresses each follower’s doubts with a new mission through individual consideration. 15
Transformational leaders provide large-scale inspiration and motivation for a vision or mission; however, the transformational leader’s vision is central to this model and this may inhibit its ability to effect change in health care. Fulfilling the health needs and wishes of patients is the goal and duty of health care providers. At the same time, health care providers must educate patients for them to make well-informed choices about their own health care. Patient treatment must be individualized and not forced to conform to a single vision dependent on a transformational leader’s singular mission.
Servant Leadership
Servant leadership, a model first articulated by Greenleaf, 16 focuses on serving the highest needs of others in an effort to help others achieve their goals.
Servant leadership focuses on the leader’s development through awareness and self-knowledge. Self-reflection and awareness enable a leader to understand his or her purpose, beliefs, and individual characteristics.
This process of reflection leads to moral insights that develop one’s personal conscience as well as core ethical and moral beliefs.
As a component of the moral core, Greenleaf called for servant leaders to take into consideration the effects of their actions and the actions of the individuals that they serve “on the least privileged in society.”
As a moral core develops, the servant leader implements those internalized virtues and attitudes to the skills, behaviors, and interactions involved in leadership.17
Spears 18 identified the qualities and characteristics of servant leadership:
- listening,
- empathy,
- healing,
- awareness,
- persuasion,
- conceptualization,
- foresight,
- stewardship,
- commitment to the growth of people, and
- building community.
These characteristics, along with a moral core, drive servant leaders to help people meet their goals and overcome challenges.
Many of these characteristics involve interpersonal interaction and contribute to strong relationships and trust between leaders and others.
If, as discussed in the section on Improving Quality and Lowering Cost to Increase Value, a patient has a high degree of trust in the health care provider and the health care team has a high degree of mutual trust, then that trust will improve the quality of care and lower the cost of care, thus improving value.
For example, ongoing provider-patient high-trust relationships will facilitate more efficient and lower cost care because repeated diagnostic procedures and treatments can be prevented.
These strong trust relationships can create a steady stream of patients for health care providers and decrease the need for provider marketing, thereby potentially decreasing the cost of care to the patient.
Servant leadership aligns well with the needs for leadership in health care because health care providers’ work, and their life calling, is to serve their patients.
The ethical and moral aspects of servant leadership require a health care provider to put the physical, emotional, and financial needs of the patient first.
The skill set of listening, empathy, awareness, healing, and persuasion all contribute to a healthy health care provider-patient relationship. These interpersonal skills overlap with patient-centered communication, which has “been linked to outcomes such as patient satisfaction, adherence, and more positive health outcomes.” 19
Servant leadership, as it overlaps with patient-centered communication, would build trust between health care providers and patients.
Servant leadership will enable health care providers to create positive patient outcomes by promoting change in patient health behavior.
Self-determination theory describes how factors such as autonomy, competence, and relatedness interact to motivate individuals to change. 20 Autonomy refers to the level of intrinsic motivation driving behavioral change.
Competence refers to the patient’s confidence and ability to change. 20 Relatedness refers to the patient’s perception “of being respected, understood, and cared for.” 20
Health care providers can affect these factors and motivate patients to change. 20 Health care providers, functioning as servant leaders, can provide patients with the skills, tools, and feedback necessary for self-determination.
As discussed earlier, teamwork is an essential element of health care delivery. Doctors, nurses, administrators, and allied health staff work together in teams to diagnose and treat patient illness.
Servant leaders can build a community in which team members are committed to putting the patient’s interest first and organize team members to achieve the goal of providing high-value patient care.
By helping other health care providers pursue and achieve their goals, servant leaders can inspire high performance and innovation throughout health care. More efficient medical procedures, innovative medical equipment technology, and new treatments are possible in an environment in which servant leaders encourage and serve other health care providers to achieve their goals, which in turn will translate to better safety, outcomes, service, and efficiencies within the health care system, increasing the value equation for the patient.
Although there is a great deal of alignment of servant leadership when working with a team (big or small) in caring for patients, it does not fit every situation. It may lack the speed needed when an issue is urgent, such as a code or an operating room emergency.
Depending on the leaders’ abilities, this model can at times present lack of clarity and not be the best to address conflict.
In the final analysis, it depends on how the leader leads and the strength of the team that has been developed.
Conclusion
The challenges facing health care require strong leadership.
The model of leadership will vary depending on the situation, and in reality a leader may exhibit a blend of leadership models.
The purpose of leadership is to work with others to improve the situation.
Because health care is about people caring for others and there should be alignment with how we treat patients and how we work together as staff, servant leadership may be considered a dominant model.
Servant leadership is best aligned with the professional and ethical duties of health care providers in delivering the high-value care patients deserve.
Servant leadership focuses on trust and empowerment in both the patient relationship and the health care provider team relationships.
The challenges faced by the health care system extend beyond the clinical setting. Servant leadership can also stimulate necessary change so that all health care stakeholders focus on serving others: their patients and their staff.
By aligning health care stakeholders to serve patients and each other, a more sustainable health care system providing an improved value equation of high-quality care and lower cost is possible.
References
See the original paper
Originally published at https://www.mayoclinicproceedings.org.
PDF version
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fwww.mayoclinicproceedings.org%2Faction%2FshowPdf%3Fpii%3DS0025-6196%252813%252900889-6&clen=288339