Health Systems -Transformation Institute (HSTI)
research institute & knowledge portal
Joaquim Cardoso MSc*
Founder and CEO
November 14, 2022
*MSc from London Business School — MIT Sloan Program
Source: Elsevier
Executive Summary:
An overview of the papers:
- The richness of the papers [in this publication series] lies in the fact that they aim to identify important lessons from the COVID-19 response across five main health system dimensions: preventing transmission; providing health services effectively; ensuring sufficient infrastructure and workforce capacity; paying for services; and governance)
- The varied evidence and analyses contained here are not only important for the valuable lessons learned but also as concrete contributions to the efforts now underway to rebuild and strengthen our health systems as we emerge and recover from the pandemic.
While the COVID-19 pandemic has been a severe health system shock it is by no means an isolated one
- Previous shocks such as the global financial crisis and potential new ones around the corner, like the Ukrainian refugee crisis, all serve to highlight how the resilience of health systems may be tested, often to limits that are difficult to bounce back from.
The COVID-19 pandemic uncovered a number of well-known chronic vulnerabilities and deficiencies in our health systems that need to be addressed.
- In terms of its policy legacy, this crisis provides a window of opportunity to examine and learn which actions can contribute to stronger, better performing health systems.
- A good overview and some key messages for resilience and recovery can be found in the European Commission co-funded project ‘State of health in the EU’, with its 29 Country health profiles and Companion report published in December 2021.
- Let’s not forget that the last stage of a shock cycle is ‘recovery and learning’, but this is not a one way street; rather the feedback loop between the two are what makes the pandemic a powerful agent of transformative change.
Looking to the future we’d like to offer two final considerations that could provide some guidance on forging necessary change.
1.Firstly, as the lessons emerging from this Special Issue make clear, the emphasis now should be on transformation and implementation.
2.Secondly, we should always remain mindful that viruses are not the only things that cross borders — effectively countering many other potential threats to health and health systems, be they economic, environmental, social or epidemiological, requires European and/or international co-operation.
ORIGINAL PUBLICATION (full version)

Lessons learned from the COVID-19 pandemic [editorial]
Science Direct (Elsevier)
Reinhard Busse, Natasha Azzopardi , Isabel de la Mata , Josep Figueras
Available online 9 April 2022
It is with great pleasure and satisfaction that we lend our support to the collection of papers in this Special Issue of Health Policy which draws on the body of evidence gathered in the COVID-19 Health Systems Response Monitor (HSRM) and its network of international experts.
The HSRM is a joint undertaking of the WHO Regional Office for Europe, the European Commission, and the European Observatory on Health Systems and Policies.
The richness of the papers lies in the fact that they aim to identify important lessons from the COVID-19 response across five main health system dimensions:
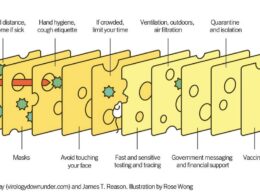
- preventing transmission;
- providing health services effectively;
- ensuring sufficient infrastructure and workforce capacity;
- paying for services; and
- governance
as well as through dedicated cross-country comparisons covering all European Union and a large portion of WHO European Region Member States as well as Canada and the United States.
This body of work could not have been possible without the hard work and commitment of all the COVID-19 HSRM network members.
This Special Issue builds on and complements an ever growing range of network outputs, including the HSRM Monitor platform itself as well as policy briefs and snapshots, a major study on health system resilience, three issues of Eurohealth and a series of webinars, to name a few.
And while the academic papers published here are aimed at the research community, the analyses are essentially powered by the conviction to be as policy-relevant as possible for the wider constituencies of policy advisors and senior government officials, who will undoubtedly find valuable information to add to their arsenal of policy tools to meet the forthcoming challenges that await our health systems.
For this reason, our gratitude to the institutions and individuals who make up the HSRM, to the journal Health Policy, to the editors of this Special Issue and to all of the contributing authors is redoubled.
The varied evidence and analyses contained here are not only important for the valuable lessons learned but also as concrete contributions to the efforts now underway to rebuild and strengthen our health systems as we emerge and recover from the pandemic.
While the COVID-19 pandemic has been a severe health system shock it is by no means an isolated one.
Previous shocks such as the global financial crisis and potential new ones around the corner, like the Ukrainian refugee crisis, all serve to highlight how the resilience of health systems may be tested, often to limits that are difficult to bounce back from.
While the COVID-19 pandemic has been a severe health system shock it is by no means an isolated one.
Previous shocks such as the global financial crisis and potential new ones around the corner, like the Ukrainian refugee crisis, all serve to highlight how the resilience of health systems may be tested, often to limits that are difficult to bounce back from.

The COVID-19 pandemic uncovered a number of well-known chronic vulnerabilities and deficiencies in our health systems that need to be addressed.
In terms of its policy legacy, this crisis provides a window of opportunity to examine and learn which actions can contribute to stronger, better performing health systems.
A good overview and some key messages for resilience and recovery can be found in the European Commission co-funded project ‘State of health in the EU’, with its 29 Country health profiles and Companion report published in December 2021.
Let’s not forget that the last stage of a shock cycle is ‘recovery and learning’, but this is not a one way street; rather the feedback loop between the two are what makes the pandemic a powerful agent of transformative change.
Let’s not forget that the last stage of a shock cycle is ‘recovery and learning’, but this is not a one way street; rather the feedback loop between the two are what makes the pandemic a powerful agent of transformative change.

Looking to the future we’d like to offer two final considerations that could provide some guidance on forging necessary change.
1.Firstly, as the lessons emerging from this Special Issue make clear, the emphasis now should be on transformation and implementation.
Many of the examples of best practices and innovations collected here are not new in themselves.
What is new is the newfound capacity to govern, and transform health systems to implement reforms in key areas such as primary health care, financing, the health workforce or digital health.
In other words, key areas of focus now should be on how to harness innovations and rethink their implementation.
2.Secondly, we should always remain mindful that viruses are not the only things that cross borders — effectively countering many other potential threats to health and health systems, be they economic, environmental, social or epidemiological, requires European and/or international co-operation.
The public good that results from such co-operation may require some pooling of national decision-making in policy-making in order to tackle common threats, but as demonstrated by the co-operation in producing and purchasing effective vaccines, the pay-offs can be enormous.
Let us all strive to learn from the pandemic and strengthen our health systems to be more resilient to future health system shocks.
About the authors & affiliations
Reinhard Busse
Head, Department Health Care Management, Technical University of Berlin; Co-director, European Observatory on Health Systems and Policies
Natasha Azzopardi
Muscat Director, Country Health Policies and Systems, WHO Regional Office for Europe
Isabel de la Mata
Principal Advisor for Health and Crisis Management, European Commission
Josep Figueras
Director, European Observatory on Health Systems and Policies
Originally published at: https://www.sciencedirect.com


APPENDIX: AN OVERVIEW OF THE PUBLICATION
European Health Observatory
Debora Miranda
Lessons from the pandemic response across Europe and beyond will help policy-makers prepare for future shocks
A compilation of lessons learned from the COVID-19 response is now available in a Special Issue of the journal Health Policy.
An international group of experts and institutions compared the performance of 50 countries, mainly in the WHO European Region, and considered why some have managed the pandemic more successfully than others.
The Special Issue stems from the work of the COVID-19 Health System Response Monitor (HSRM), a collaboration set up in March 2020 between the European Observatory on Health Systems and Policies, WHO/Europe and the European Commission.
As the early days of the pandemic left policy-makers and health professionals scrambling for information on how to manage the impact of the pandemic, HSRM filled thein the knowledge gap by collecting up-to-date information on how health systems were responding to the crisis.
“From increasing intensive care unit (ICU) bed capacity or expanding the health workforce, to managing vaccination rollouts, the measures put in place by health systems can help to explain why some countries have been able to keep death rates comparatively low even in the presence of severe COVID-19 outbreaks,” reads the foreword of the Special Issue.
As Reinhard Busse, Natasha Azzopardi Muscat, Isabel de la Mata and Josep Figueras from the three organizations explain, well-functioning health systems have often been able to limit disruptions to service delivery, preventing increases in waiting times, but others have been forced to convert into almost exclusively COVID-care: “For many countries, the inability of the health system to cope with the pressures of COVID-19 was a significant factor behind repeated lockdowns”.
Comparing how countries responded between March 2020 and late 2021
All articles are based on the content featuring in the HSRM, focusing on a specific topic or comparing responses from groups of countries.
The papers identify lessons from the COVID-19 response across five main health system dimensions:
- In the article on preventing transmission, authors emphasize the importance of governance in introducing measures to reduce COVID-19 infection.
- To ensure sufficient infrastructure and workforce capacity, authors consider a range of options that are relevant for countries tackling backlogs of care in their systems, such as redeploying staff, using private providers and using inter-regional and cross-border patient transfers.
- Common strategies for adapting service delivery included postponing elective care, reconfiguring hospital wards and transforming primary care models, for example to use multidisciplinary teams.
- Authors also show that more can be done to better prepare financing systems for unexpected drops in public revenues, smoothing provider income losses due to reduced demand, and covering extra costs related to providing new types of services.
- Governance is another important theme. Although public health measures were relatively easier to implement earlier in the pandemic, this shifted over time as populations pushed back against restrictions, particularly in countries with lower trust in government.
The second set of articles of the Special Issue highlight the breadth of the Health Systems and Policy Network, covering experiences from 33 countries mostly from the WHO European Region, including all European Union members, plus Canada and the United States.
For example, the authors show how in Nordic countries with strong welfare systems and high levels of trust in government, COVID-19 experienced less devastating impact, and how inconsistent messaging and alignment between health experts and political leadership in English-speaking countries was a key factor in weak compliance with public health measures.
A source for policy-makers responding to future challenges
Despite the difficulty in maintaining measures over a long period of time, making it virtually impossible for any country to manage the pandemic consistently well, there are many examples of good practices and innovations that could help countries prepare for similar shocks, such as coping with the rapid influx of refugees in 2022.
Editors of the Special Issue Ewout van Ginneken, Erin Webb, Anna Maresso, Jonathan Cylus and the HSRM network suggest that countries use experiences from the HSRM archive to test their health systems and identify weaknesses in the context of different shocks:
“One of the key advantages of this resource is that countries do not need to rely solely on their own policy experiences but also can explore concrete examples that have been applied elsewhere, being mindful of course of specific country contexts”.
Moving forward, making health systems more resilient requires, among other measures, supporting the workforce, tackling backlogs of care, implementing new models of care, strengthening mental health services, and using digital health services appropriately.
Moving forward, making health systems more resilient requires, among other measures, supporting the workforce, tackling backlogs of care, implementing new models of care, strengthening mental health services, and using digital health services appropriately.