The Health Strategist
institute for health strategy & digital health
Joaquim Cardoso MSc
Chief Strategy Officer (CSO), Researcher & Editor
May 1, 2023
There is a mounting exodus of healthcare workers from the UK’s National Health Service (NHS), with an estimated 18,000 UK-trained doctors now practising overseas, a 50% increase since 2008.
- Pay is not the sole solution to stemming the flow of medics, with many citing workplace culture, burnout and stress as key factors driving the exodus.
- While an improved salary may help, the role of pay in the NHS’s retention problem is often overstated.
Broader and deeper changes are needed, such as increasing the number of managers, investing in equipment and technology, and improving the experience of working on the wards.
- Ultimately, the same things that will fix the NHS in the long run will also make it less difficult to work in.
SELECTED IMAGE(S)

DEEP DIVE

Pay rises alone will not stem the flow of Britain’s medics
Stress, burnout and workplace culture are driving the mounting exodus
Financial Times
JOHN BURN-MURDOCH
May 1, 2023
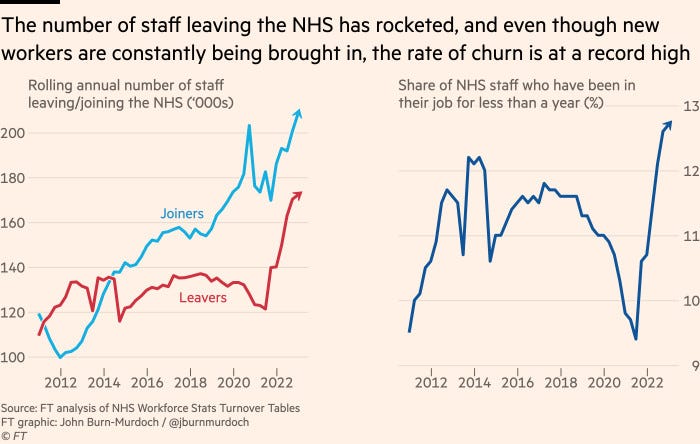
Something troubling is happening to staffing in Britain’s national health service. Despite steady upward trends in the numbers of new doctors and nurses, vacancies continue to rise. In short, the NHS has developed a leak.
And it’s not an easy one to mop up, since it frequently drips into other countries. According to the latest figures, there are now an estimated 18,000 UK-trained doctors practising overseas. This is a 50 per cent increase since 2008. To put it another way, one in seven practising doctors who trained in Britain is now working elsewhere. This is almost three times the average rate among peer countries.

Some argue that there can’t really be a staffing crisis if the NHS can consistently recruit from overseas to make up for these departures.
This may partially help to fill the shortfall but there are two problems with this view.
The first is that staff recruited from overseas often return to their origin countries. Just 10 per cent of doctors who trained elsewhere before coming to work for the NHS are practising in the UK today, compared with 75 per cent of those who trained in the UK.
The second is that even if recruitment can keep pace with departures, the churn rate itself is a problem. As of last December, one in eight NHS staff had been in their current role for less than a year, the highest figure since this series was first recorded in 2009.
This means more work is carried out by agency staff or less experienced team members, which has been shown to increase the risk of harm to patients.
So what can be done to plug the leak?
As nurses went on strike again on Sunday and talks between the government and junior doctors remain stalled, the most obvious and frequently mentioned solution is pay.
Critics of striking medics argue that everyone’s pay is suffering at the moment. But doctors and nurses have had it worse than most.
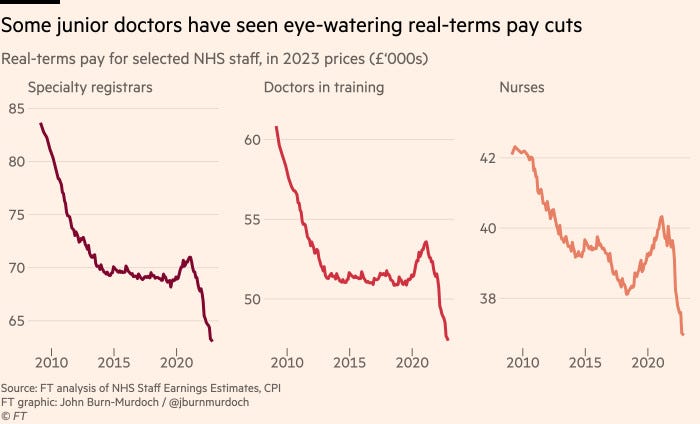
The recent inflation rise has taken the average British worker’s real wages down to 2.5 per cent below their 2009 level, but earnings are down 13 per cent for nurses and 24 per cent for junior doctors over the same period.
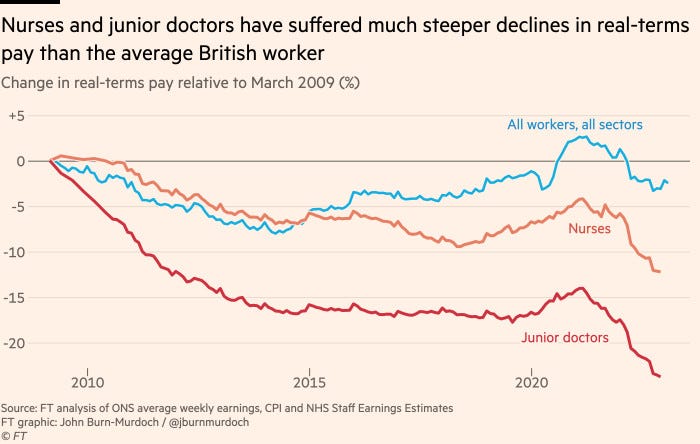
The result is that highly skilled and expensively trained medical professionals are slipping down the UK’s income distribution, while the list of countries where they could earn more grows by the year. ]
As the pay-off for a gruelling decade of training and an intensely stressful job diminishes, it is not surprising that they look elsewhere.
But while an improved salary will surely help, the role of pay in the NHS’s retention problem is often overstated.
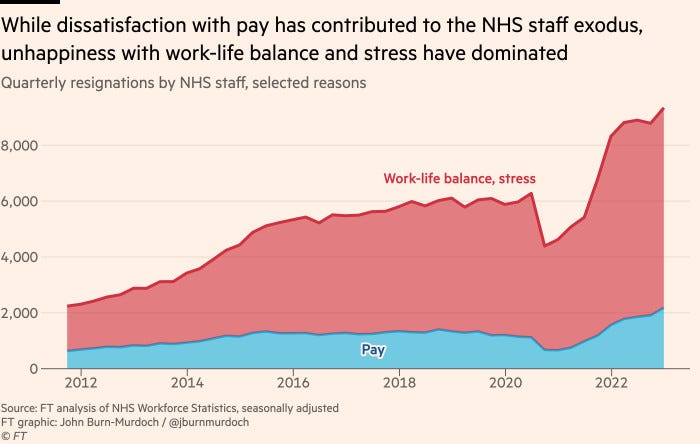
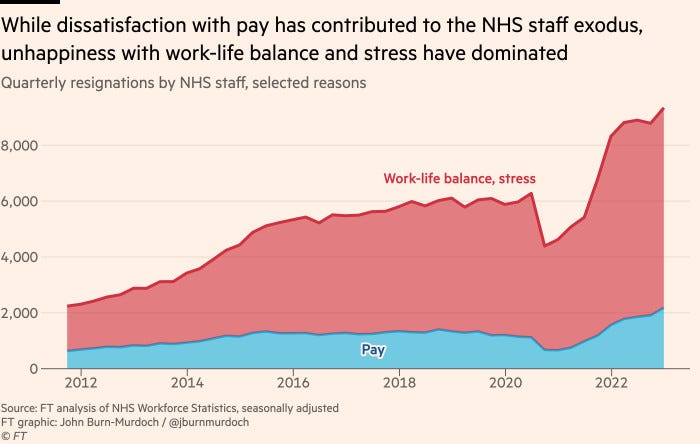
When a cohort of doctors who recently left the UK were asked what had prompted them to go, they were about twice as likely to point to workplace culture, burnout and stress as to financial reasons.
This is corroborated by NHS data, which shows that the huge increase in voluntary resignations over the past two years has been driven by people citing problems with their work-life balance.
The most damning assessments come from a series of interviews with UK-trained doctors who have gone overseas, carried out for the General Medical Council.
- While pay was mentioned by some, qualitative factors dominated, including that
- other countries’ healthcare systems provide “less bureaucracy and more time to spend on clinical practice”
- “highly modern and technology-centred institutions”,
- a feeling of being “supported and valued by the state and employer”, “an easier, less intense lifestyle” and — according to an interview with respondents who left the UK for India — “no shortage of staff”.

The government’s hardball stance on pay will do little to dispel British healthcare workers’ growing sense of being under appreciated, but even once a deal is reached, broader and deeper changes are needed if an NHS career is to regain its allure.
- Increasing the anaemic numbers of managers to free up nurses and doctors to do what they were trained for, and
- investing in equipment and technology to improve the experience of working on the wards would be good places to start.
Ultimately, the same things that will fix the NHS in the long run will also make it less difficult to work in right now.
Originally published at https://www-ft-com.ezp.lib.cam.ac.uk.