PAHO
WHO
September, 2016
Key Messages (from Conclusion)
- Improving access to and utilization of breast care programs can impact breast cancer incidence and survival.
- An essential first step to improving access is identifying the existing structural, sociocultural, personal and financial barriers.
- Strategies for improving equitable access to breast cancer care should be customized to meet the needs of a target community.
- Cancer survivors, advocates and healthcare providers should be engaged in identifying and addressing barriers.
- Programs should consider local resource availability, sociocultural traits of the community and economic variables.
- Health professionals can be advocates and promoters of breast care health through participation in continuing medical education, providing breast counseling to patients and participating in health system improvement projects.
KEY POLICY SUMMARY:
Improve access by addressing structural barriers
· Coordination of services, strong referral networks, patient navigators and other structural changes can improve patient access to timely breast cancer diagnosis and treatment.
· Human resource capacity building may also improve patient access to care. (e.g., training in breast cancer risk factors, clinical breast exams and proper referral procedures) may improve early detection and outcomes.
· Geographic distribution of services impact access to care (local versus centralized). Centralized services should include outreach to outlying communities.
Improve access by addressing sociocultural barriers
· Cancer survivors, advocates, non-governmental organizations and civil society can be valuable partners in identifying and addressing patient access and quality of care issues.
· Community education about risk-factors, early detection and treatment can reduce stigma, myths and misconceptions about breast cancer.
· Strengthening partnerships between health facilities and community partners can improve equitable access to care without duplication of services.
Improve access by addressing personal barriers
· Improving health-literacy and raising awareness about risk-factors and early detection can reduce fear about seeking care for breast concerns.
· Engaging cancer survivors in supportive care can help reduce psychosocial barriers to treatment.
Improve access by addressing financial barriers
· Health insurance, subsidized medicines and support for transportation and housing during treatment can reduce financial barriers.
· Providing financial support for transportation or housing during treatment can reduce barriers.
Follow a resource-stratified pathway
· Breast cancer programs should follow a defined resource-stratified pathway to allow for coordinated, incremental program improvement across the continuum of care.
· A ‘pathway’ is a progression of resource investment, program development, quality improvements and interval health gains.
· Program design and improvements should be based on outcome goals, identified barriers and needs and available resources.
About this Knowledge Summary (KS):
This summary discusses how to improve equitable access to breast cancer care by reducing barriers to breast health services. It covers structural, sociocultural, personal and financial barriers to accessing breast cancer detection, treatment and supportive care.
INTRODUCTION & THE CHALLENGE
Numerous barriers to timely and equitable access to quality breast health care exist across the cancer care continuum and negatively impact cancer outcomes. Improving access to care and reducing disparities in outcomes requires identifying, understanding and addressing those barriers. Barriers differ by location and population, but can generally be characterized as: structural, sociocultural, personal and financial. Raising awareness and reducing barriers to cancer care services can improve patient outcomes, provided appropriate diagnostic and treatment facilities are available, accessible and acceptable.
POLICY ACTION
OVERVIEW
Preplanning
· Identify current and previous efforts to address access to care.
· Identify data that may provide insight into existing barriers and facilitators.
· Identify who will lead the process of identifying and addressing barriers and facilitators.
Planning Step 1: Where are we now? (Investigate and assess)
· Assess breast health services (accessibility, availability, affordability, acceptability)
· Assess community partnerships (advocacy groups, public health services, women’s clinics)
· Identify barriers and facilitators to accessing breast health services (structural, sociocultural, personal and financial).
Planning Step 2: Where do we want to be? (Set objectives and priorities)
· Define target population.
· Identify gaps and introduce new policies and services to reduce barriers to care.
· Set objectives that promote a common goal: improving access to equitable cancer care services.
· Assess feasibility of interventions.
Planning Step 3: How do we get there? (Implement and evaluate)
· Follow a resource-stratified approach to breast cancer care that considers available resources and equitable access to quality care for all women.
· Engage stakeholders (advocates, patients, providers) across disciplines and sectors.
· Address barriers: build health system capacity, raise awareness and reduce financial barriers using a resource-stratified pathway.
· Monitor and evaluate implementation of policy changes.
WHAT WE KNOW
Disparities in breast cancer outcomes vary widely between low- and middle income countries (LMICs) and high-income countries (HIC) as well as within countries. Despite lower incidence rates in LMICs, mortality-to-incidence ratios are significantly higher than those in HIC. This is in part due to late stage diagnosis in low-resource settings where over 80% of women present with advanced and late stage disease, requiring metastatic disease management and palliative care rather than curative care. In contrast, in HICs, over 80% of breast cancer patients present with early stage disease and are potentially curable.
Barriers to utilization of breast care services negatively impact breast cancer outcomes. Delays in presentation with a breast complaint can be attributed to structural, sociocultural, personal and financial barriers. Structural barriers can include the geographic location of services, transportation needs, insufficient diagnostic or treatment services and shortages of essential medicines and insufficient or undertrained workforce. They also include inefficient or poorly coordinated services requiring multiple visits to initiate definitive diagnosis, poor referral networks and inadequate patient navigation. Women who live in remote or rural areas are less likely to undergo screening, less likely to access care, including supportive care, and suffer greater psychosocial effects of diagnosis and treatment. Sociocultural barriers include myths and misconceptions about the causes and treatment of cancer, stigma, language, discrimination, social class, gender and religious beliefs. Personal barriers may include mistrust of the health system, fear of a cancer diagnosis, low health-literacy or competing family and work obligations. Financial barriers to accessing care include direct, out-of-pocket payment for services and indirect costs such as transportation, housing, childcare and lost wages.
Identifying the type of barriers (e.g., structural, sociocultural, personal or financial) that impact the target population can help identify the best intervention for improving access to care. For example, programs to improve structural barriers should emphasize multidisciplinary team approaches, protocols for referrals, and quality control metrics that track time from presentation with breast concern to diagnosis and time from diagnosis to treatment. Programs to reduce sociocultural and personal barriers would ideally engage community stakeholders and breast cancer survivors in education campaigns and supportive services.
Workforce capacity and services integration: Health systems often face shortages of healthcare providers, especially those trained in screening, detecting, diagnosing and treating cancer. Integrating breast cancer care programs into maternal or women’s health services, for example, is potentially synergistic but in already strained primary care settings this may create additional barriers unless human resource allocations are adequately addressed. Introducing or expanding existing programs without providing additional human resources can result in ‘caregiver burnout’ as health professionals encounter more challenging working conditions, higher workload and inadequate infrastructure to perform their work (see Table 1).
Treatment (medicines and therapies): Increasing awareness of breast cancer and improving access to detection without addressing treatment can have negative consequences. Access to standard medications deemed essential for optimal breast cancer care can be limited by policy, cost and distribution systems. At a minimum, patients would have access to medications on the WHO Model List of Essential Medications (e.g., pain medications, tamoxifen). Access to pain medicine is a fundamental right and global health policy priority, yet opioid analgesics are often undervalued as an essential treatment. Many patients remain unable to access these medicines due to a lack of balance between controlled drug laws and access for medicinal use. Expanding access to breast cancer medicines beyond essential medicines can be challenging and research should consider therapeutic interventions relevant to LMIC populations. Surgery and radiotherapy are significant treatment modalities for breast cancer. Simple surgery techniques may be taken up by general surgeons at primary and secondary care centers to reduce the burden on specialist surgeons in cancer centers. While there are also deficits in availability of radiotherapy facilities in LMICs, at least one specialist cancer centre should be equipped with this intervention. According to the International Atomic Energy Agency (IAEA) as of 2008, only 30% of the world’s radiotherapy facilities were in developing countries, where 85% of the world’s population lives. Existing radiation equipment is often outdated or out of service. Limited access and long waits for radiotherapy can result in suboptimal breast cancer care and can limit effective treatment options.
Stigma, myths and misconceptions: In communities where cancer is highly stigmatized, women may be less likely to access breast health services, as feelings of shame may lead them to remain silent or attempt to hide their condition. Stigma is shaped by local beliefs and perceptions which may be based on myths and misconceptions about cancer. Beliefs and perceptions of health care are shaped by culture and society and influence healthcare-seeking and decision-making behavior. “Fatalism” is the belief that one does not have any control over disease, life, or death. The belief that breast cancer is inevitably fatal is reinforced when breast cancer cases within a community are not detected and treated at an early stage, when treatments can lead to cure or long-term survival. Women may opt not to utilize detection or screening services or pursue follow-up evaluation after a positive screening if they believe cancer is not treatable, or worse, if they believe detection speeds death.
Relating an illness to events, situations or experiences in life is another cultural construct similar to fatalism that may interfere with a woman seeking medical evaluation and treatment. Other misconceptions about breast cancer (e.g., that cancer is contagious or a curse from god) and breast cancer diagnosis (e.g., that the diagnosis process requires removal of the breast rather than a small biopsy), may also limit a women’s willingness to seek breast cancer care. Breast cancer survivors who are willing to speak publically about their experience can play a vital role in reducing stigma, dispelling damaging myths and misconceptions and changing beliefs and perceptions.
Psychological support: Psychological issues related to a breast cancer diagnosis and the associated stigma include depression, anxiety and distress. Clinical assessment tools and protocols for treatment of depression and anxiety are available. Treatment includes supportive care (counseling) and if available and appropriate, pharmaceutical therapies such as anti-depressants and anti-anxiety medications. Long-term stress can also have physiologic effects such as lower immune responses, fatigue and insomnia, which may impact health outcomes. Addressing a patient’s mental health can improve her physical outcome. Fear is a common response to serious health concern or a stigmatized condition. Fear related to breast cancer can be related to physical aspects of disease or treatment (e.g., fear of pain and discomfort from biopsy or surgery, fear of nausea, hair loss or other toxic effects from radiation or chemotherapy), or to psychosocial aspects (e.g., fear of a changing role at home or work, fear of loss of femininity or distorted body image).
Family dynamics: A diagnosis of breast cancer can shift family roles and strain family dynamics. A woman may avoid seeking care for breast concerns if she fears that her spouse will leave her. If family members (husband, children, relatives) react negatively to a diagnosis of breast cancer, a woman may be left unsupported physically, psychologically, socially and financially, and require additional supportive services from the community and/or health system. Many women who self-identify a breast problem do not seek timely medical evaluation for these reasons. Body image is also a concern expressed by women diagnosed with breast cancer.
Patient-provider dynamics: Attitudes toward healthcare providers shaped by passed experiences or sociocultural and religious beliefs impact utilization of the healthcare system. In some settings, a lack of trust in the healthcare system and a preference for traditional healers can be a barrier to accessing care in a healthcare system. Consulting traditional healers first for breast cancer can delay early detection and reduce possible curative treatment options. Lack of trust in the health system includes concerns over reports of corruption and medical fraud, mistrust of individuals or groups of healthcare providers and reports or personal experience of negative or suboptimal care. Examples of suboptimal care include: suboptimal doses of treatment, expensive and unnecessary medications and interventions, paternalistic patient-provider relations, withholding diagnostic information from patients, a lack of female providers and culturally insensitive communication or practices.
Coordination of care, referral networks and patient navigation: Cancer care is complex and can last months or years requiring series of test and rounds of treatment and follow-up. Navigating this process can be challenging for patients and their families especially when referral networks fail, services are not coordinated or patients face delays, lack information about their treatment, or must travel long distances. Patient navigation refers to how patients, their families and caregivers access and navigate available health services. Patient navigators are health professionals (nurses, physicians, social workers) or trained community workers or volunteers (breast cancer survivors, advocates) who assist patients in navigating the system by helping with appointment scheduling and coordination of care. More sophisticated patient navigation services may include arranging financial support, facilitating communication between providers and ensuring patients adhere to treatment recommendations. Studies from HICs report that patient navigators improve rates of breast cancer screening, quality of life and patient satisfaction.
Cost of care: The inability to pay for care or the fear that services will lead to economic devastation prevents many women from seeking care at all resource levels. Women are more likely to seek care if they have health insurance or personal wealth. Conversely, user fees (private, out-of-pocket health expenditures) limit access to services. According to the WHO, government-financed health services in most low income countries are increasingly dependent on user fees paid by patients, which are nearly double public health expenditures. Early detection and screening can result in more cost-effective treatment of early stage disease than
PLANNING STEP 1: WHERE ARE WE NOW?
POLICY ACTION:
INVESTIGATE AND ASSESS
Assess access to breast health services for all women
· Examine data on breast cancer incidence in the target service area (early detection, diagnostic, treatment, palliation facilities).
· Determine level of accessibility to breast cancer services in terms of geographic distribution and transportation.
· Determine availability of essential medicines, advanced medicines and basic and specialty services (surgical services, pathology services, radiation therapy, chemotherapy, palliative care and supportive care).
· Determine distribution and types of health professionals (primary care, specialists, support staff) and diversity of staff (gender, ethnicity, cultural connection to service community).
· Determine level of health professional knowledge of breast cancer care, utilization of multidisciplinary teams and referral networks and competency of health professionals in culturally sensitive communication skills relevant to breast health.
Assess community partnerships
· Examine existing and potential collaborations with survivor and advocacy groups. Advocacy groups (breast cancer awareness, psychosocial support, policy input) can have different functions depending on the setting and resources available.
· Examine existing and potential outreach collaborations with women’s and children’s health services or public health services.
Identify patient barriers and facilitators
· Identify structural barriers (human resources, diagnostic and treatment services, referral network, essential medications, geographic location, transportation, patient navigation).
· Identify socio-cultural barriers (stigma, religion, gender, social class).
· Identify personal barriers (fear, education, experience, health literacy, health status, competing family and work priorities, psychosocial, supportive and home care services)
· Identify financial barriers (socioeconomic, direct and indirect, opportunity cost, childcare, lost wages).
· Determine socioeconomic status of service population and identify possible high-risk, marginalized and disenfranchised populations.
WHAT WORKS
Data collection and analysis: Quantitative and qualitative data are essential to identifying barriers to access in a target population. Accurate data and record keeping is an essential component of breast cancer care. Population-based data can help identify barriers, bottlenecks, loss-to-follow-up and other areas for health system improvement. According to the WHO, the following information should be routinely collected: demographic and socioeconomic data (including information that can be used as a unique patient identifier), legal data such as consents and authorizations, financial data relating to fees and clinical patient data (diagnosis and treatments). Breastcancer-specific data should be documented, including tumor site, stage and time and type of treatment. Other valuable data include: economic indicators, access to finances for healthcare, public transportation costs and location of health facilities. Qualitative research through focus groups and interviews with key informants and representatives of the target population can provide insight into beliefs, perceptions and experiences that impact access to care. This data can help profile the high-risk populations, identify competing health priorities and identify healthcare infrastructure barriers and available supportive care services.
Location, coordination of services and strengthening points of contact and referral networks: Location and capacity considerations must be part of breast cancer program improvements. Each health facility within a health system can play a role in promoting breast cancer care, but this requires coordination, such as designating some health facilities to offer specialty services through referrals from other health facilities. Selecting which health facility offers which services requires balancing priorities such as proximity to a given population, against transportation barriers. Understanding where women in the target population receive primary care can inform resource allocations for health professionals and their patients. Health centers, district hospitals and primary care clinics are often the primary point of contact for women with breast complaints. While specialty centers can improve outcomes (e.g., breast surgery outcomes can be superior in higher-volume facilities, high-volume pathology laboratories can produce more accurate results), having all patients receive treatment at a centralized facility is not practical if a significant portion of a population lives in remote areas.
Timely communication between providers will ensure that women receive integrated, effective care. Standard protocols for referrals should be developed between the primary point of contact and follow-up breast cancer diagnosis and treatment facilities. Building local capacity and strengthening referral networks can help ensure timely and appropriate access to both local and centralized specialty care. For example, a facility with fewer resources available may perform diagnostic tests, initiate surgical treatment and then refer to a regional center for chemotherapy. This requires health system referral networks and coordination of services to minimize delays in services, which can improve outcomes.
Investing in human resources capacity: When increasing breast cancer awareness and improving access to breast health services, it is essential to plan for how the health system will handle increases in breast concerns and detection of suspicious cases. Programs to address human resources capacity for healthcare are needed at all resource levels. Strategies to build capacity should combine non-monetary and monetary policies that can improve health worker retention and performance such as providing continuing medical education, ensuring decent working conditions and wages and promoting a culture that supports employees. A multi-sectored and integrated-systems approach can help address existing and anticipated human resource deficits. Examples of integrated approaches include investing in and training community health workers engaged in maternal child health to counsel on breast awareness, or adapting palliative care programs developed for communicable diseases (e.g. HIV/AIDS) to include non-communicable diseases including breast cancer.
When experts are available, a multidisciplinary (or interdisciplinary) team approach should be employed. Multidisciplinary breast programs can led to improved treatment plans and reduce duplication of care. In low-resource settings, a multidisciplinary team may include only 2–4 members (i.e.., surgeon, pathologist, nurse, medical oncologist), but can help ensure services are coordinated. Tumor boards have been used successfully in LMICs, and can provide patient oversight and standardize procedures. These synergies can reduce overall costs to comprehensive cancer care. Health systems can also partner with academic institutions and other stakeholders to develop training programs to increase the number of health professionals trained in breast health (see Table 1).
Education and community outreach: Efforts to improve access to care must also consider cultural, social and psychosocial barriers to accessing care. Patient education and community outreach can improve participation in early detection programs and reduce misconceptions about breast cancer and breast cancer treatment. Educational programs will vary by region or country, and core messages should address the target population’s cultural and social barriers. Strategic messaging about breast health can be conveyed by health professionals during patient encounters, or through organized breast awareness campaigns that involve breast cancer survivors, advocacy groups, community health workers, local volunteers and health professionals. Early detection interventions can include personalized reminders to women or small media campaigns.
Financing models and cost sharing: National health plans should consider political, social and cultural factors impacting health system costs when proposing financing models and target populations for breast cancer programs in LMICs. Communication and collaboration between health systems and other financial stakeholders should be ongoing to reduce cost and increase access to advanced therapies such as Her2neu monoclonal antibody therapy or aromatase inibitors. Strategies include matching the cost of medicines to the patients’ ability to pay (i.e., subsidized medicines). Governments, health systems and other stakeholders can also improve access to medications through negotiations with pharmaceutical companies regarding prices, manufacturing of generic medications and drug donation programs. Alternative financing models, such as conditional cash payments, prepayment, or insurance schemes, may reduce financial barriers, but are limited in scope and have the potential for corruption and misuse. Limiting the amount of out-of-pocket patient expenditure can reduce catastrophic health expenditure scenarios for patients and encourage participation. As the HIV/ AIDS epidemic demonstrated, without access to affordable treatment, people are unlikely to participate in screening.
PLANNING STEP 2: WHERE DO WE WANT TO BE?
POLICY ACTION:
IDENTIFY OBJECTIVES AND PRIORITIES
Identify community and health system partnerships
· Equitable access to timely diagnosis and treatment requires community and health system collaboration (e.g., local, centralized, women’s clinics, public health services, civil society, academic institutions).
· Community leaders, health professionals, breast cancer specialists, survivors, advocates, health care management personnel and policymakers should contribute to program planning and to provide feedback on interventions.
· Partnerships with stakeholders should aim to minimize barriers and patient cost of care.
Set achievable objectives
· Objectives should promote a common goal: improving access to equitable, quality cancer care.
· Consider policy interventions to reduce structural barriers (recruitment and training of health professionals or access to essential medicines, including opioid analgesics).
· Consider policy interventions to reduce sociocultural barriers (education and strategic messaging to reduce stigma, myths and misconceptions about breast cancer).
· Consider policy interventions to reduce personal barriers (assess psychosocial needs and provide supportive care for patients, possibly through engaging survivor networks).
· Consider policy interventions to reduce financial barriers (alter the payment structure and reduce the risk of catastrophic health expenditures).
Set priorities and determine feasibility of interventions
· Follow a resource-stratified pathway that considers how allocation of resources, payment for services and sociocultural issues impact utilization of services.
· Use available and relevant economic metrics and modeling including cost effective analysis to set priorities.
· Consider feasibility and affordability of interventions over the long-term.
· Demonstration projects may help ensure program feasibility (quality and sustainability) prior to population-wide implementation.
HOW DO WE GET THERE?
Identify and address patient access barriers: Engaging the relevant stakeholders (e.g., healthcare providers, patients, survivors, advocates, caregivers) in identifying and assessing the existing barriers to accessing early detection services and treatment is the first step in reducing access barriers. Qualitative research methods including observation, interviews and focus groups with breast cancer patients/survivors, key informants and other stakeholders as well as surveys and other assessment tools can be used to identify barriers and inform program direction (see Planning Comprehensive Breast Cancer Programs). Demonstration projects can be used to assess the impact and effectiveness of interventions to reduce barriers. In low-resource settings where cost parameters and effectiveness of cancer programs are not well known, focusing on a limited geographic area that has a high-risk population can be more cost-effective and allows for adjustments to be made before scaling up or additional investments.
Advocacy and community outreach: Health systems can benefit from partnering with and supporting local advocacy groups to draw attention to the need for improved access to care as well as to ensure breast cancer awareness messages are consistent, culturally appropriate and reflect available services. Breast cancer survivors are valuable advocates, as they are living testimony that women can survive breast cancer and lead productive and quality lives. They can also provide important information about the health system from a patient perspective and help inform health policymakers about local, national and global breast cancer issues. Local advocates can provide cultural context to breast cancer awareness programs and address community misconceptions about breast cancer or breast cancer treatment. Outreach programs should include women and men, and engage the community. For example, outreach to religious groups and traditional healers has been shown to be effective in increasing referral to care for pregnancy and infectious-disease-related conditions in some settings, and may be effective with breast cancer early detection as well.
Establishing national cancer centers: Centralized centers of excellence can serve as core resources within a larger health care network offering multidisciplinary expertise in clinical care, clinical guidelines, research priorities, public policy, advocacy and training. However, for a centralized center of excellence to succeed, improvements in existing referral processes are often needed and patient access to centralized services must be addressed. Investment in comprehensive care centers must be balanced against geographic limitations in patient access to care, and the need to advance the capacity of district, provincial and general hospitals that function as the primary point of contact for most cancer patients.
Patient navigation and patient information: Studies in LMICs indicate that patient navigation can reduce the number of health encounters and unnecessary steps to receiving appropriate care. Patient-centered decision aids are another tool that can be used by patient navigators to improve a woman’s understanding of her health, the implications of a breast cancer diagnosis and her treatment plan.
Decision aids can be shared by telephone calls, text messages, educational videos, emails, or one-on-one meetings. Decision aids allow women to take a more active role in decision-making. The use of healthcare decision aids during diagnosis and treatment visits have been shown to improve patient knowledge regarding the diagnostic process and treatment options (such as breast-conserving surgery versus mastectomy). Patient treatment summaries that patients can share with members of their healthcare team can help avoid duplication of tests or misinformation about a patient’s condition, treatment or preferences.
Economic modeling and process metrics: Economic modeling and metrics are important policy tools and can help identify strategies to reduce financial barriers to accessing care, assess programmatic performance and ensure sustainability of a breast cancer program. Cost-effectiveness analyses can assess the relative benefit of a health program or intervention. For example, studies show that treating early-stage breast cancer with surgery and radiotherapy is more cost-effective than systemic chemotherapy for metastatic disease. Cost effectiveness analysis can provide useful information, but has limitations; it often assesses interventions as vertical programs, and cannot easily capture the benefit of integrated services. Economic modeling could also predict the health care cost passed to the patient versus to the health system, recognizing that a major barrier to care is the cost of interventions passed on directly to the patient. Process metrics can be used at a local level to track improvement along a resource-stratified pathway (see Table 3). Process metrics may be designed to minimize its own cost to the program while at the same time contributing to overall quality assurance efforts. When possible, metrics can be integrated into the WHO Health Metrics Network (see WHO HMN Toolkit 2014).
Resource-stratified pathway: Access to care is a key principle of the resource-stratified pathway approach. A resource-stratified pathway approach to breast cancer programs is a stepwise progression of resource investment, program development and interval health gains. It must consider how allocation of these resources (local versus centralized), payment for services (health insurance versus out-of-pocket) and sociocultural issues impact utilization of services. Resource allocations should consider not just the type of services or resources required for a program (pathology lab, radiation equipment, surgical expertise, chemotherapy medications), but the location of services (transportation and housing barriers), health professional capacity (expertise in breast cancer care and culturally sensitive communication skills), and patient access issues, including sociocultural barriers. Progression along a resource-stratified pathway will be different for each region or country, and must consider the advantages of centralized services alongside the potential barriers to equitable access that arise from centralization. Investment strategies must consider improved access to breast cancer services for all women. A phased introduction of programs addressing screening, diagnosis and pathology and treatment may be appropriate (see Tables 1 & 2).
PLANNING STEP 3: HOW DO WE GET THERE?
POLICY ACTION:
IMPLEMENT AND EVALUATE
Establish political and financial support
· Secure necessary political and financial resources for policy interventions.
· Consider alternative financing models, such as conditional cash payments, prepayment, or insurance schemes to reduce financial barriers.
· Incorporate economic modeling and process metrics related to access to care into program development and expansion (see Table 3).
Launch, disseminate and implement
· Partner with national and local stakeholders, survivors and advocates to coordinate dissemination of policy changes and implementation of programs plans (goals, objectives and best practices).
· Balance national and centralized program implementation and expansion with resources to assure equitable access to services.
Monitor and evaluate
· Establish assessment, process and quality metrics and outcome measures.
· Collect and analyze data to assess the impact of policy interventions and identify additional barriers, bottle-necks and loss-to-follow up
CONCLUSION
- Improving access to and utilization of breast care programs can impact breast cancer incidence and survival.
- An essential first step to improving access is identifying the existing structural, sociocultural, personal and financial barriers.
- Strategies for improving equitable access to breast cancer care should be customized to meet the needs of a target community.
- Cancer survivors, advocates and healthcare providers should be engaged in identifying and addressing barriers.
- Programs should consider local resource availability, sociocultural traits of the community and economic variables.
- Health professionals can be advocates and promoters of breast care health through participation in continuing medical education, providing breast counseling to patients and participating in health system improvement projects.
Table 1. Breast Care Programs: Human Resource Allocation
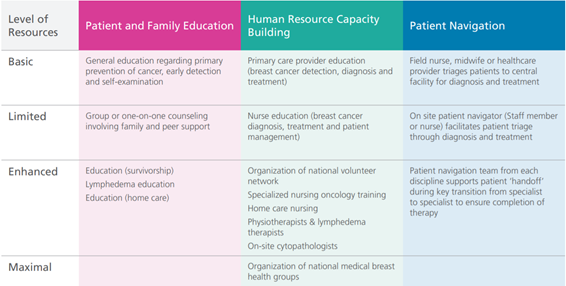
Adapted from Anderson BO, Yip CH, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the Breast Health Global Initiative Global Summit 2007. Cancer. 2008 Oct 15;113(8 Suppl):2221–43.
Table 2. Breast Care Programs: Support Systems Resource Allocations
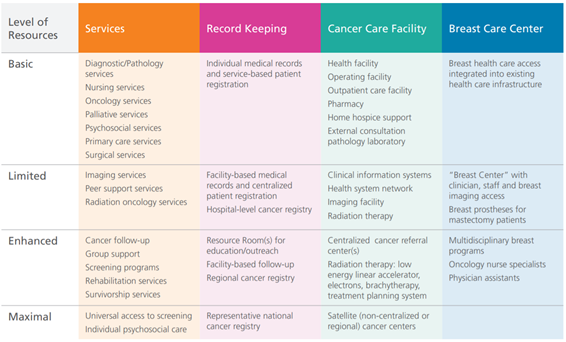
Adapted from Anderson BO, Yip CH, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the Breast Health Global Initiative Global Summit 2007. Cancer. 2008 Oct 15;113(8 Suppl):2221–43.
Table 3. Process Metrics for LMIC Breast Healthcare Programs from Anderson 2008
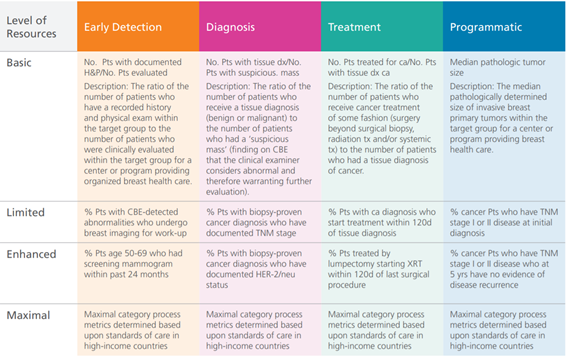
Anderson BO, Yip CH, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the Breast Health Global Initiative Global Summit 2007. Cancer. 2008 Oct 15;113(8 Suppl):2221–43.
Originally published at: https://www.paho.orgPLANNING: IMPROVING ACCESS TO BREAST CANCER CURE
About this Knowledge Summary This summary covers planning for breast cancer programs, including long-term planning. It…www.paho.org