Health Strategy Review
health management, engineering and
technology review
Joaquim Cardoso MSc.
Senior Research and Strategy Officer (CRSO) —
for Health Strategy Research
Chief Editor — for the Health Strategy Review
Chief Advisor — for Health Strategy Advisory
July 25, 2023
Summary
Individuals with SARS-CoV-2 infection can develop symptoms that persist well beyond the acute phase of COVID-19 or emerge after the acute phase, lasting for weeks or months after the initial acute illness.
The post-acute sequelae of COVID-19, which include physical, cognitive, and mental health impairments, are known collectively as long COVID or post-COVID-19 condition.
The substantial burden of this multisystem condition is felt at individual, health-care system, and socioeconomic levels, on an unprecedented scale.
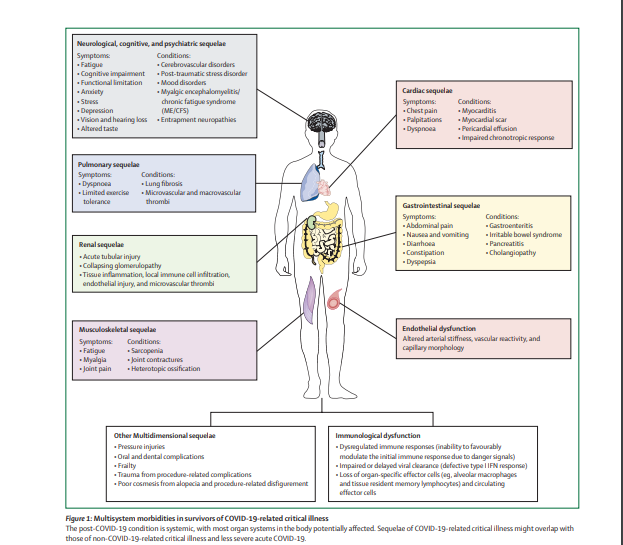
Survivors of COVID-19-related critical illness are at risk of the well known sequelae of acute respiratory distress syndrome, sepsis, and chronic critical illness, and these multidimensional morbidities might be difficult to differentiate from the specific effects of SARS-CoV-2 and COVID-19.
The authors provide an overview of the manifestations of post-COVID-19 condition after critical illness in adults.
The authors explore the effects on various organ systems, describe potential pathophysiological mechanisms, and consider the challenges of providing clinical care and support for survivors of critical illness with multisystem manifestations.
Research is needed to reduce the incidence of post-acute sequelae of COVID-19-related critical illness and to optimise therapeutic and rehabilitative care and support for patients.
Infographic
DEEP DIVE
Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations
The Lancet — Respiratory Medicine
Matteo Parotto, MD; Prof Mariann Gyöngyösi, MD; Kathryn Howe, MD; Prof Sheila N Myatra, MD; Otavio Ranzani, MD; Prof Manu Shankar-Hari, MD; et al.
July 2023
Key messages
- Many individuals with SARS-CoV-2 infection have symptoms that persist well beyond or develop after the acute phase; these sequelae of COVID-19, known collectively as long COVID or post-COVID-19 condition, can last for weeks, months, or years after the acute illness
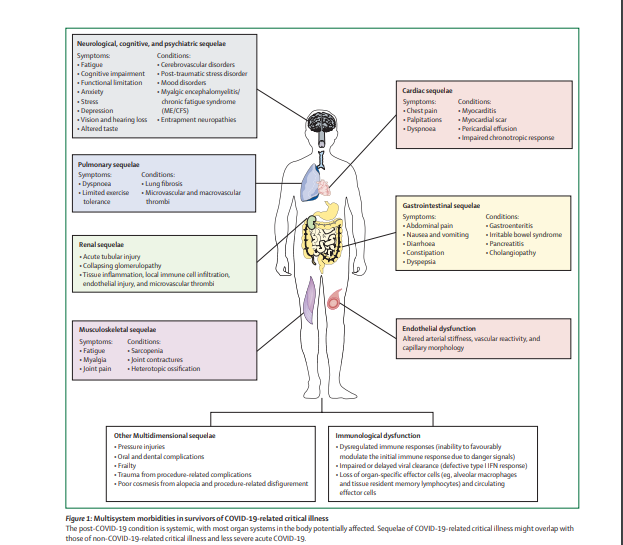
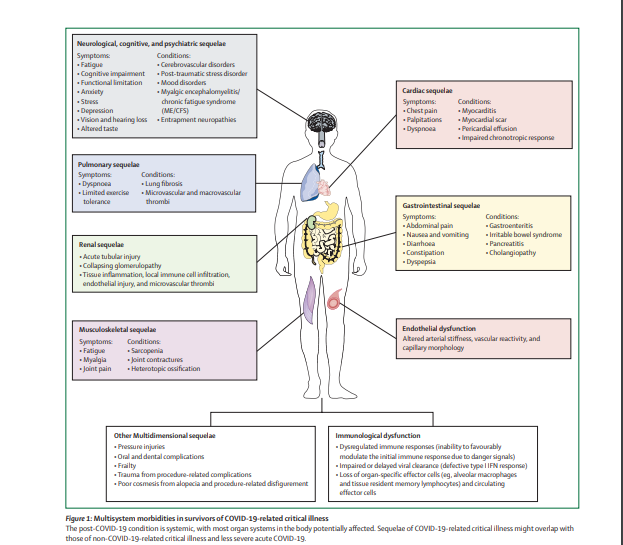
- The post-COVID-19 condition is systemic, with most organ systems in the body potentially affected; potential mechanisms include pathophysiological changes related to virus-specific effects, immunological and inflammatory dysregulation damage in response to the acute infection, and expected sequelae of critical illness
- Challenges that must be addressed in providing therapeutic and rehabilitative care and support for people with multisystem post-COVID-19 condition include the novelty of the condition, the overwhelming number of individuals affected, the need to coordinate multidisciplinary expertise, and the need to reach vulnerable and neglected populations; models of care have been proposed, drawing on previous experiences with survivors of critical illness
- The intersection of socioeconomic factors, pre-existing comorbidities, support and health-care access, and the consequences of critical illness is complex and might contribute to disparities in presentation, experiences, and outcomes of post-COVID-19 condition for patients and caregivers
- Research is needed to understand the causes and pathophysiological mechanisms of post-COVID-19 condition, to distinguish the effects of COVID-19 from those of critical illness per se, to develop specific preventive and therapeutic interventions for post-acute sequelae of COVID-19-related critical illness, and to understand and meet the needs of all those affected
Introduction
Many individuals with SARS-CoV-2 infection have symptoms that persist well beyond the acute phase or emerge after the acute phase, lasting for weeks, months, or even years after the initial acute illness.
Various terms have been proposed to describe this collection of symptoms, which span physical, cognitive, and mental health domains and multiple organ systems, including long COVID, post-acute sequelae of SARS-CoV-2 infection or COVID-19, or post-COVID-19 syndrome. In 2021, WHO conducted a multidisciplinary expert consensus process and adopted the term post-COVID-19 condition, which they defined as a “condition that occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis”.
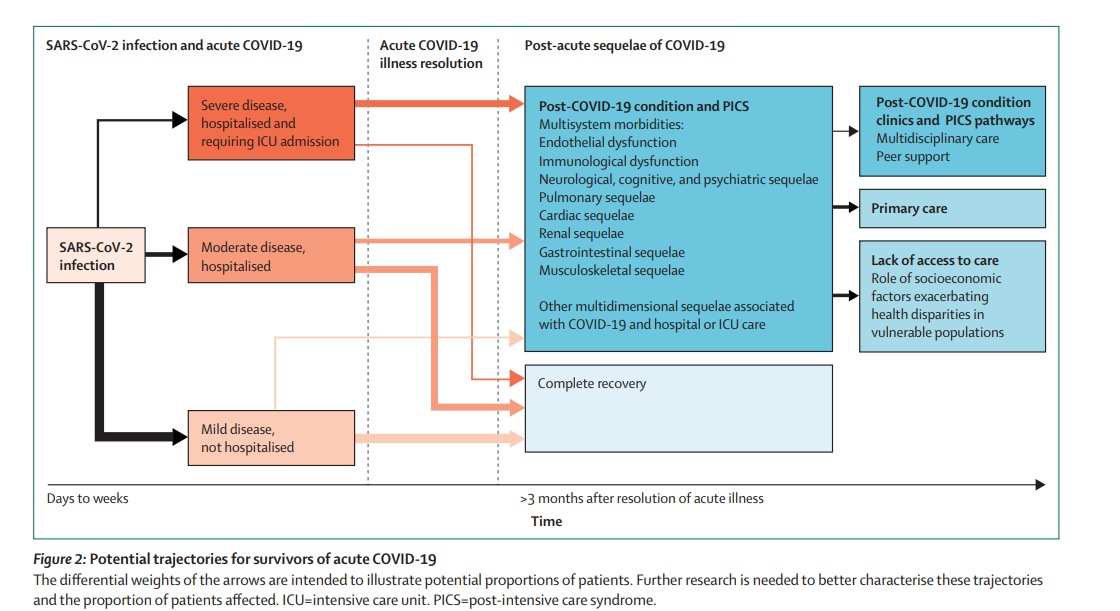
The proportion of patients affected by post-COVID-19 condition might be in the range of 10–30% of those infected with SARS-CoV-2, although understanding of this condition is still evolving. Many individuals are therefore presenting with this new and complex systemic condition, and there is an urgent need to identify individuals at risk, the overlapping contribution of various factors (other than the direct effects of, and the host response to, SARS-CoV-2) to the post-acute sequelae of COVID-19 (eg, the consequences of critical illness), and potential approaches to clinical care and support. Patients who are critically ill and admitted to the intensive care unit (ICU) with acute COVID-19 might be at an increased risk of a range of post-acute sequelae.
In this Series paper, we provide an overview of the multisystem manifestations of the post-COVID-19 condition, with a primary focus on adult survivors of critical illness. The first paper in this Series reviewed pulmonary and extrapulmonary origins of respiratory symptoms after acute COVID-19 and considered approaches to clinical care and rehabilitation.
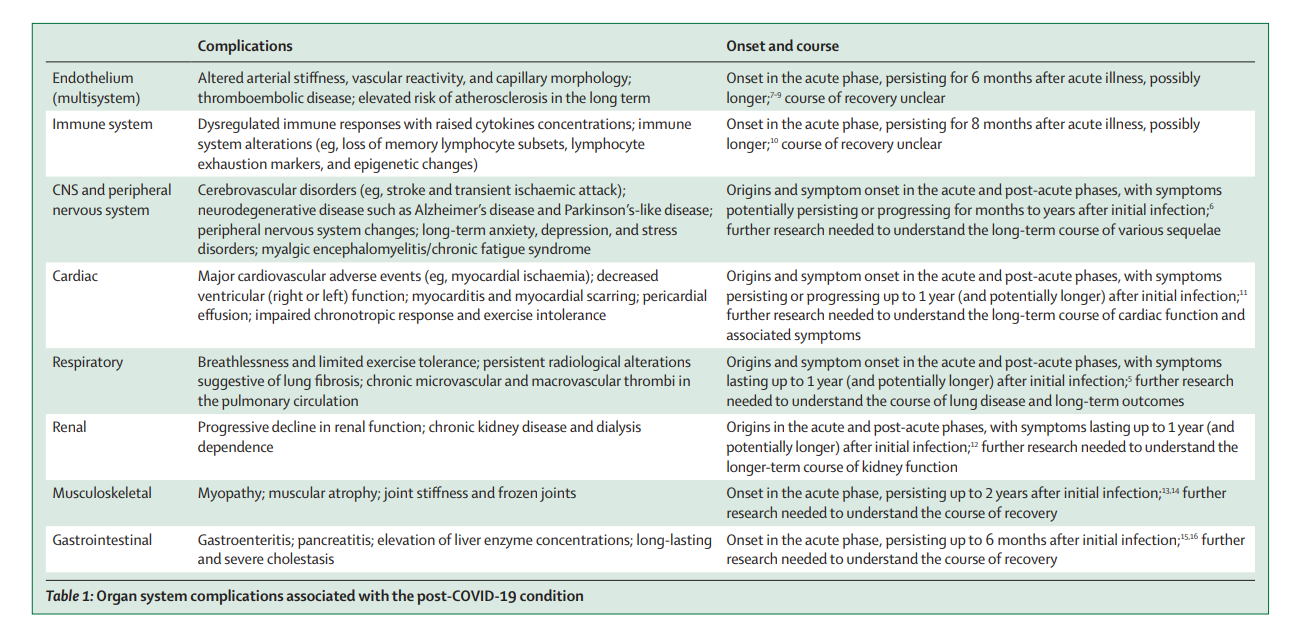
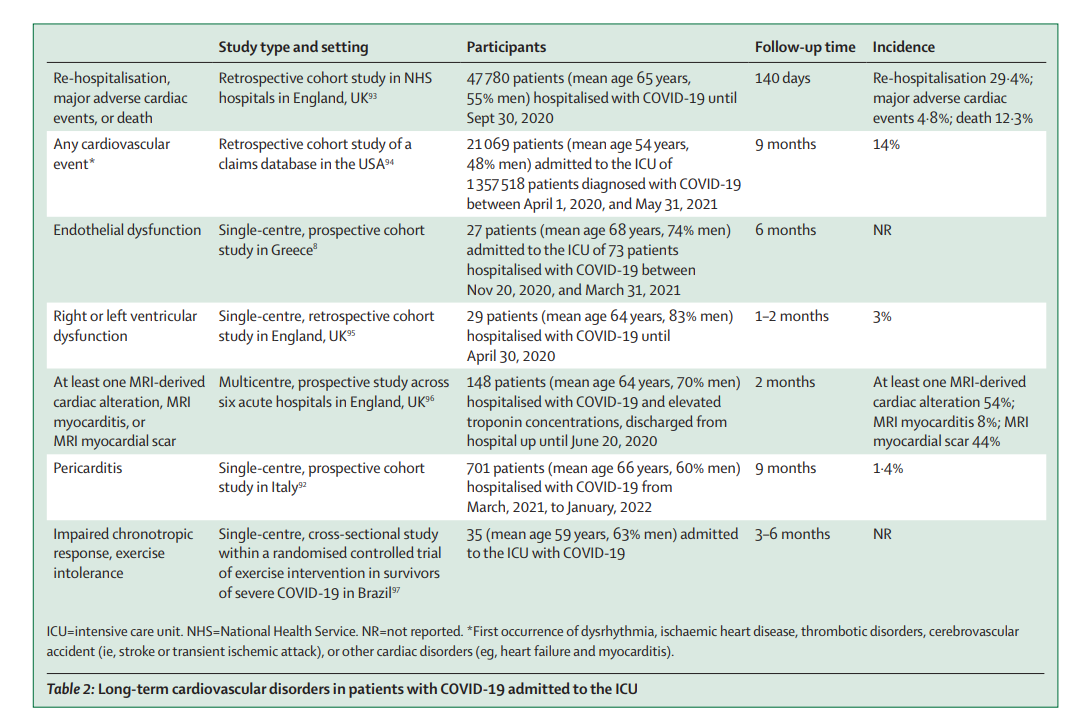
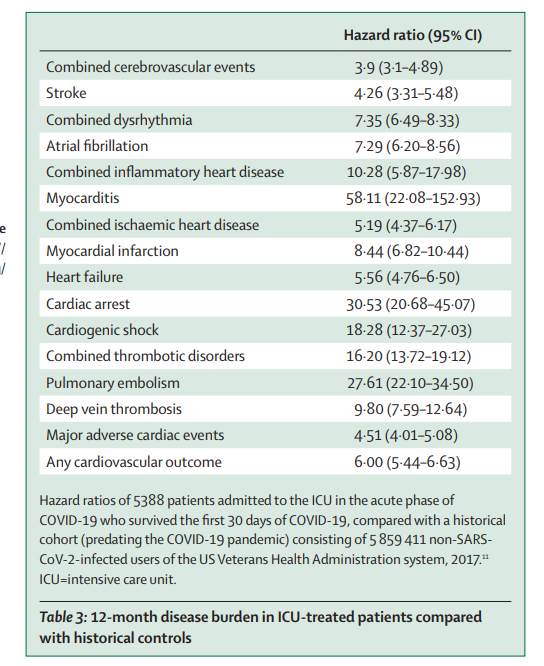
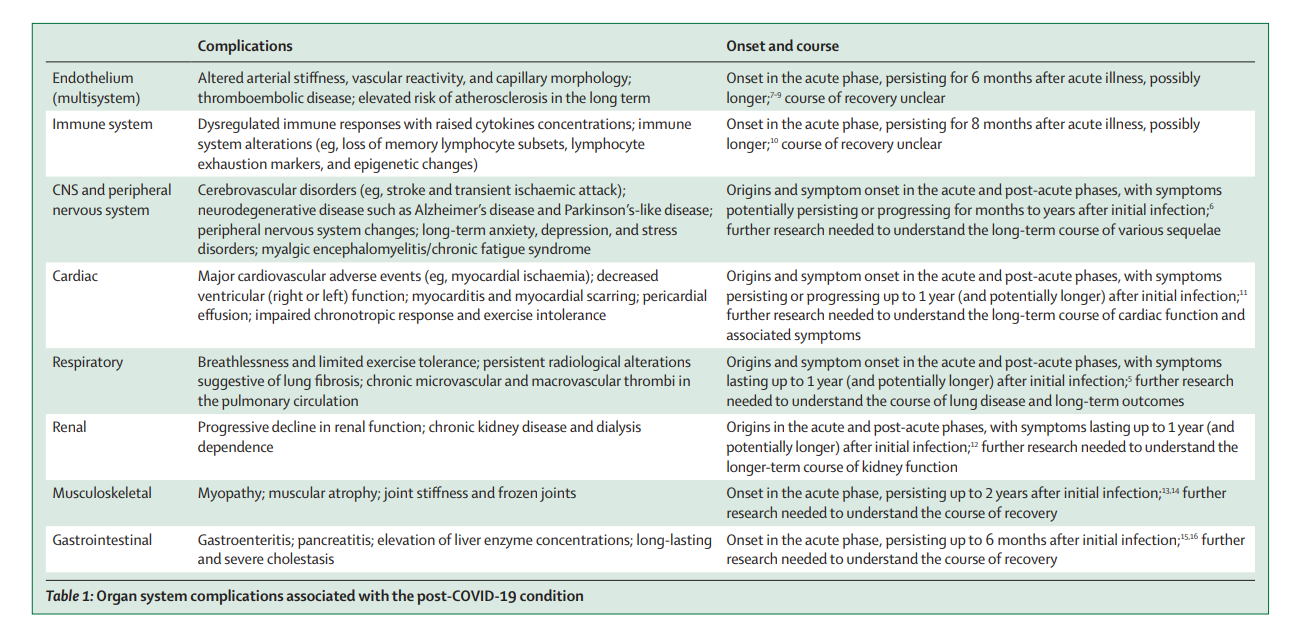
The second paper focused on the pressing need to mitigate neurological, cognitive, and psychiatric sequelae of COVID-19-related critical illness. We consider the multisystem, longitudinal effects of endothelial dysfunction and immune system dysfunction before reviewing organ system sequelae of COVID-19, which are summarised in table 1. We highlight the challenges of providing appropriate care and support for patients with a novel, heterogeneous, multisystem condition and outline priorities for research.
Table 1- Organ system complications associated with the post-COVID-19 condition
Other sections
see the original publication
Conclusions and future directions
The COVID-19 pandemic has shown the consequences of a dysregulated endothelium, an exuberant inflammatory response, and an altered immune system in the acute setting, with nearly 7 million deaths globally as of June 30, 2023. Importantly, in COVID-19 survivors, residual dysfunction of the endothelium and the immune system continues, with a complex interplay that manifests in many of the multisystem sequelae that we describe in this Series paper. As every organ system is reliant on homoeostasis of the endothelium and appropriate immune responses, it is perhaps unsurprising that multisystem dysfunction ensues for many individuals. COVID-19 survivors are a large proportion of the global population, and timely discussion of the data available is needed to address the burden of post-acute sequelae, acknowledging that much remains to be learnt about the biological and clinical consequences of COVID-19.
The post-COVID-19 condition is systemic, affecting various organ systems. It results in increased use of health-care resources, decreased quality of life, and increased susceptibility to subsequent viral or bacterial infection, and leads to heightened vulnerability to perioperative morbidity and mortality for individuals who require a surgical procedure for any (unrelated) indication. With a large and growing global population of survivors of COVID-19, the impact on individuals, health-care systems, communities, and society is likely to be substantial.
The post-COVID-19 condition might be explained partly by pathophysiological changes related to virus-specific effects, immunological and inflammatory dysregulation damage in response to the acute infection, and expected sequelae of post-critical illness. However, understanding of causes and risk factors, underlying pathophysiological mechanisms, and the course of biological and clinical features of post-COVID-19 condition remains incomplete and continues to evolve. Better characterisation of the specific consequences of SARS-CoV-2 infection and COVID-19 versus the effects of critical illness per se is needed (panel). Many survivors of COVID-19-related critical illness have persistent weakness, which is probably related to ICU-acquired weakness from severe illness, immobility, paralytics, or deep coma. A central issue to elucidate is the way in which reported symptoms relate to organ dysfunction or chronic disease in the post-acute phase.
Identifying steps that can be taken during the acute phase of COVID-19 to prevent or reduce the range and severity of post-acute sequelae — based on an understanding of causes, risk factors, aetiology and pathophysiology — is a priority for clinicians, researchers, patients, and other stakeholders. At present, there are no specific treatments for post-COVID-19-condition. Health-care teams should assess for potentially modifiable symptoms and consider treatments for similar conditions in individuals without COVID-19 that might offer benefit in this population.
Progress in understanding of aetiology and pathophysiology will provide a foundation for the development of specific, targeted treatments for the post-acute sequelae of COVID-19.
Socioeconomic factors are fundamental determinants of health after COVID-19. Individuals from low-income and middle-income countries, those from marginalised communities, and those who are socially disadvantaged are probably disproportionately affected; however, these groups are systematically under-represented in research studies owing to several contributing factors (insufficient local resources, compromised access to health care, poor education, poor health advocacy and literacy, institutional racism, and poverty), which limits understanding of intersectionality in COVID-19 and leaves an important global health knowledge gap to fill (panel).
Overall, the burden of post-COVID-19 condition has important individual, health-care system, and socioeconomic implications on an unprecedented scale. A substantial proportion of survivors of COVID-19-related critical illness are affected by multisystem involvement, with a degree of overlap with PICS. Further research will help to characterise the nature of and risk factors for post-COVID-19 condition, to develop potential preventive and therapeutic treatments and models of care and support, and to address the needs of vulnerable populations and patients in low-income and middle-income countries.
References
See the original publication