health and tech
institute
Joaquim Cardoso MSc
Founder, Chief Researcher & Editor
February 4, 2023
EXECUTIVE SUMMARY
In February 2023, the World Cancer Day and International Childhood Cancer Day campaigns aim to reduce cancer mortality and improve survival by closing the gap in cancer inequality and inequity.
- Cancer inequality refers to unequal distribution of resources while cancer inequity refers to unjust differences in care or outcomes due to factors such as race, poverty, and disability.
- Cancer mortality is highest in Europe where it is the leading cause of death for those under 65 years old, with educational and sex-based disparities affecting the mortality rates.
- Inequitable access to cancer screening and treatments exacerbates the problem.
- Childhood cancer survivors also face long-term health difficulties and employment challenges.
To address these inequities and inequalities, primary health care needs to be strengthened and policies and programs must be implemented that allocate more resources to disadvantaged groups.
- The EU’s Cancer Beating Plan addresses cancer disparities and has established the European Cancer Inequalities Registry.
- Tackling both inequity and inequality is crucial in improving cancer care.
INFOGRAPHIC
DEEP DIVE

Reduce cancer inequity and inequality to reduce cancer mortality
The Lancet
Editorial
February, 2023
In February, 2023, World Cancer Day (February 4) and International Childhood Cancer Day (February 15) will be commemorated with “Close the Care Gap” and “Better Survival” campaigns, respectively.
The emphasis of these campaigns is to reduce cancer mortality and increase survival.
To achieve these aims, it is essential to bridge gaps in cancer inequality-uneven distribution of resources and cancer inequity-unjust, avoidable differences in care or outcomes.
The difference between inequality and inequity might seem subtle, but it is not: providing everyone with equal resources (ie, equality) will not close the gap in cancer care unless everyone receives the care they need (ie, equity) to achieve similar outcomes.

Considerable progress has been made towards improvement of cancer survival, largely due to the advances in medical research, rollout of screening programmes, and availability of treatments.
However, such progress has also highlighted inequities and inequalities in cancer prevention, diagnosis, and treatment. Factors that contribute to cancer inequality often occur as a result of unequal distribution of resources, whereas the root causes of inequity are due to race, refugee status, poverty, socioeconomic status, gender norms and discrimination, and barriers for minority ethnic populations and people with disability. Cancer inequality is a more commonly used term even when referring to cancer inequities, and thus, often there is little awareness and understanding about the distinction between equity and equality. It is imperative to address both cancer inequity and cancer inequality to improve cancer survival.

Globally, Europeans are disproportionately affected by cancer.
Although Europeans account for only 10% of the global population, 25% of all annual cancer cases occur in Europe and cancer is the number one cause of death among Europeans aged younger than 65 years.
Although Europeans account for only 10% of the global population, 25% of all annual cancer cases occur in Europe and cancer is the number one cause of death among Europeans aged younger than 65 years.
A study by Vaccarella and colleagues found that within and across countries in Europe, cancer mortality rates were substantially affected by inequities in socioeconomic education status.
Individuals with lower education had higher mortality rates than those with higher education across nearly all cancer types.
Sex differences were also identified, whereby 32% of cancer deaths in men and 16% in women were associated with educational inequalities.
Literacy is a modifiable cancer risk factor, and this study highlights the need to address literacy as one of the causes that is compounding cancer inequity and mortality.
Literacy is a modifiable cancer risk factor, and this study highlights the need to address literacy as one of the causes that is compounding cancer inequity and mortality.
In Europe, one in every 300 children born in 2020 is likely to develop cancer by the age of 19 years.
Childhood cancer can lead to substantial short-term and long-term inequalities since cancer is a likely re-occurrence in adult survivors who had childhood cancer.
A study by Chang and colleagues showed that the most deprived adult survivors of childhood cancer had a higher burden of health diseases than the least deprived individuals.
Furthermore, childhood cancer survivors face difficulties in employment late in life.
Frederiksen and colleagues found that by the age of 30 years old, 9.2% of childhood cancer survivors were unemployed for health reasons.
From a scientific perspective, childhood cancers remain rare and therefore it is important to collect more data across countries.
The new childhood incidence data section of the European Cancer Information System brings these data together from across Europe, which will enable policy makers and stakeholders in EU Member States to better monitor trends and outcomes for different diagnostic groups of childhood cancer.

Inequitable access to cancer screening and treatments further accentuates cancer mortality.
Although many European countries have cancer screening programmes, disparities exist by economic status.
A study by Bozhar and colleagues found that income-based inequality in breast and colorectal screening was highest in southern Europe, and individuals with a low household income were less likely to utilise cancer screening than those with a high household income.
Furthermore, many people cannot access life-saving treatments such as chemotherapy, due to the absence of universal health coverage and costs.
Cancer survival rates among people living in rural areas are lower than people living in urban areas due to inaccessibility of resources.
To close this inequity gap, uniform population-based screening policies need to be targeted and tailored to the most vulnerable groups in society and mobile services should be provided for individuals living in remote areas.

Collectively, inequities in the prevention, diagnosis, and treatment of cancer can be reduced by
… by strengthening primary health care delivered in communities; equipping health-care professionals with skills and knowledge about how inequity influences cancer care; and implementing policies and programmes with more resources allocated to the most disadvantaged groups.
… by strengthening primary health care delivered in communities; equipping health-care professionals with skills and knowledge about how inequity influences cancer care; and implementing policies and programmes with more resources allocated to the most disadvantaged groups.
Tackling inequities and inequalities is also an initiative of the EU’s Cancer Beating Plan, …
… which addresses cancer disparities associated with countries, age, sex, income, education, and urbanisation and led to the setup of the European Cancer Inequalities Registry.
The EU’s Cancer Beating Plan is ambitious but highlights the issue of cancer inequality and inequity for many governments, which should be commended.
As the European population gets older, the number of patients with cancer will increase in the future.
Both inequity and inequality represent different facets of cancer care disparities that need to be addressed separately, since a one-size-fits-all-approach is not applicable in the context of cancer care.
Both inequity and inequality represent different facets of cancer care disparities that need to be addressed separately, since a one-size-fits-all-approach is not applicable in the context of cancer care.
Originally published at https://www.thelancet.com.
REFERENCE PUBLICATION

A CANCER PLAN FOR EUROPE: INTRODUCTION
Cancer concerns us all in one way or another.
- In 2020, 2.7 million people in the European Union were diagnosed with the disease,
- and another 1.3 million people lost their lives to it 1 .
Cancer is an individual diagnosis that has important impacts on patients, but it also severely affects the lives of their families and friends.
Today, Europe accounts for a tenth of the world’s population, but a quarter of the world’s cancer cases.
Unless we take decisive action, lives lost to cancer in the EU are set to increase by more than 24% by 2035 2 , making it the leading cause of death in the EU.
The overall economic impact of cancer in Europe is estimated to exceed €100 billion annually.
Moreover, the COVID-19 pandemic has severely impacted cancer care, disrupting prevention and treatment, delaying diagnosis and vaccination, and affecting access to medicines.
Since the pandemic began, the number of cancer diagnoses has decreased, foreshadowing a future increase in cases.
Unless we take decisive action, lives lost to cancer in the EU are set to increase by more than 24% by 2035 , making it the leading cause of death in the EU.
The overall economic impact of cancer in Europe is estimated to exceed €100 billion annually.
The EU has been working to tackle cancer for decades and its actions, for example on tobacco control and protection from hazardous substances, have saved and prolonged lives.
However, the last European action plan against cancer was developed in the early 1990s and the world has seen major progress in cancer treatment in the years since.
Personalised medicine — tailored to individual situations and needs — has radically changed patients’ prognoses.
Meanwhile, research and innovation, such as mRNA3 technologies, alongside digital technologies, have dramatically advanced our understanding of cancer initiation and progression, prevention and diagnosis.
Europe urgently needs a renewed commitment to cancer prevention, treatment and care that recognises the growing challenges, and opportunities to overcome them, including the developments in cancer care.
We need a whole-of-government approach
- that focuses on the patient and maximises the potential of new technologies and insights;
- strengthens cooperation and opportunities for EU added value;
- eradicates inequalities in access to cancer knowledge, prevention, diagnosis and care;
- and delivers improved health outcomes to patients.

Europe’s Beating Cancer Plan is the EU’s response to these needs.
It reflects a political commitment to leave no stone unturned to take action against cancer.
Mobilising the collective power of the EU to drive change to the benefit of our citizens, the Cancer Plan contains concrete, ambitious actions that will support, coordinate and complement Member States’ efforts to reduce the suffering caused by cancer.
It marks the beginning of a new era in cancer prevention and care, where patients have access to high-quality screening, treatments and the latest state of the art technologies, with support at EU level that allows scale and specialisation, while fully respecting Member States’ responsibilities in health policy 4 .
In doing so, it delivers on the political guidelines of Commission President von der Leyen.
It is also a direct response to the strong and clear calls from the European Parliament for action in this area.

The aim of Europe’s Beating Cancer Plan is to tackle the entire disease pathway.
It is structured around four key action areas where the EU can add the most value:
- (1) prevention;
- (2) early detection;
- (3) diagnosis and treatment; and
- (4) quality of life of cancer patients and survivors.
Over the coming years, it will focus on research and innovation, tap into the potential that digitalisation and new technologies offer, and mobilise financial instruments to support Member States.
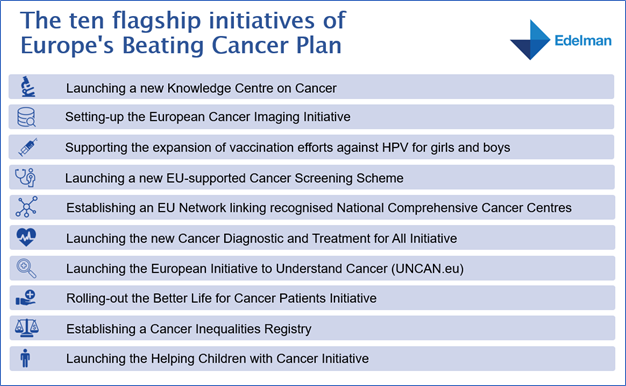
With its policy objectives, supported by ten flagship initiatives and multiple supporting actions, the Cancer Plan will help Member States turn the tide against cancer.
It will enable expertise and resources to be shared across the EU — supporting countries, regions and cities with less knowledge and capacity.
It will help researchers to exchange findings between small and large Member States and to have access to crucial health data on the potential causes of cancer and promising treatments for it.
Medical staff and hospitals will be able to tap into a wealth of shared information.
Ultimately it will ensure that patients across the EU can benefit from better care and treatment.
Europe’s Beating Cancer Plan is a key pillar of a stronger European Health Union and a more secure, better-prepared and more resilient EU.
It outlines substantive actions to mitigate the impact of the COVID-19 pandemic on cancer care and support structural improvements for a more sustainable cancer pathway.
In addition, the new, ambitious EU4Health programme and other EU instruments will provide substantial financial support with €4 billion to Member States in their efforts to make their health systems more robust and more able to address cancer.
In addition, the new, ambitious EU4Health programme and other EU instruments will provide substantial financial support with €4 billion to Member States in their efforts to make their health systems more robust and more able to address cancer.

The COVID-19 pandemic and the experience with vaccine development have clearly shown us that when we come together, when we pool our efforts and resources, it is possible to make unprecedented progress.
It requires the unique convening power of the EU, fixing goals, setting clear deadlines, committing the necessary funding and connecting the main actors through effective partnerships.
Applying this approach to cancer can deliver effective results.
By working as a team and combining efforts at national and EU level, we can overcome individual weaknesses, reduce fragmentation, and deliver a more effective and more equal response to cancer.
The strength and success must also build on engaging and communicating with the wider public to support our joint efforts.
Recognising the value of partnerships, the Cancer Plan is based on a ‘Health in All Policies’ multi-stakeholder approach and is the result of an extensive consultation process.
It reflects the views of stakeholder groups and patients, the European Parliament and Member States.

A broad array of EU policies will support the Cancer Plan with digitalisation, research and innovation as the starting point for a new approach to cancer care in the EU.
Actions will span across policy areas, from employment, education, social policy and equality, through marketing, agriculture, energy, the environment and climate, to transport, cohesion policy, and taxation.
This will enable the Cancer Plan to tackle cancer drivers in our schools and in the workplaces, in research labs, in our towns and cities, and in our rural communities; and to do so using innovation, healthy choices and improvements to our environment.
Cooperation will also be pursued internationally within the established cooperation framework with the World Health Organisation (WHO) and the long-standing collaboration with its International Agency for Research on Cancer.












